Urinary Tract Infection Duration of Treatment in Male Veterans
Received: 14-Jun-2022 / Manuscript No. JIDT-22-66558 / Editor assigned: 20-Jun-2022 / PreQC No. JIDT-22-66558 (PQ) / Reviewed: 04-Jul-2022 / QC No. JIDT-22-66558 / Revised: 07-Jul-2022 / Manuscript No. JIDT-22-66558 (R) / Published Date: 14-Jul-2022 DOI: 10.4172/2332-0877.1000510
Abstract
Background: This study aims to determine if longer antimicrobial treatment duration (>7 days) for UTI in male outpatient veterans is associated with a difference in early or late recurrence rates compared to a shorter antimicrobial treatment duration (≤ 7 days).
Methods: This study included adult, male patients of VA Eastern Kansas Health Care System with an index UTI episode between August 1st, 2020 and August 1st, 2021. If UTI recurred, infection was classified as either early (≤ 30 days) or late (>30 days) recurrence. Logistic regression models were used to evaluate the duration of antimicrobial treatment on recurrence.
Results: The effects of duration of treatment on early recurrence (P:0.5041, OR:0.660, CI:0.194-2.237) and duration of treatment on late recurrence (P:0.5024, OR:0.703, CI:0.251-1.969) both showed statistical insignificance.
Conclusion: There was no difference between long and short duration on both early and late recurrence, therefore it may not be necessary for male patients to be treated for the recommended longer duration of treatment.
Keywords: Urinary Tract Infection (UTI); Antimicrobial treatment; Diagnosis
Background
Urinary Tract Infections (UTIs) are some of the most common bacterial infections, affecting 150 million people each year worldwide [1]. Risk factors include age, female gender, sexual intercourse, presence of a catheter, and an increasing number of comorbidities [2]. A UTI is diagnosed through urine cultures and symptom presentation; then, it is categorized as either complicated or uncomplicated. Uncomplicated cases include patients that are otherwise healthy and have no underlying causes that could potentiate an infection. Complicated UTIs are those that pose a higher risk of treatment failure due to factors that compromise the urinary tract or host defense [1].
Women are 30 times more likely to experience a urinary tract infection than men [3]. UTIs in the female population are frequently studied however, the male population has not been studied as extensively [4]. In fact, the treatment guidelines for acute, uncomplicated cystitis issued by the Infectious Diseases Society of America (IDSA) specifically exclude men due to lack of evidence and literature [5]. The reported incidence in men without an indwelling catheter is 0.9 to 2.4 cases per 1000 [1]. Even though this is not all that common, there is still significant importance in acquiring literature surrounding this population.
Urinary tract infections are less common in men for many reasons. Men have a longer urethra with the opening further away from the rectum. A male UTI is usually due to an abnormality or obstruction in the urinary tract [4]. Because of this, men have historically been considered complicated cases, thus requiring longer treatment duration than women. According to the IDSA guidelines, the standard duration of therapy for an uncomplicated UTI in a female patient is 3 to 5 days. In men, the exact duration of antimicrobial therapy is unknown, however, treatment is generally recommended for 7-14 days. There is no clear evidence to support this longer duration of treatment. Extended treatment duration increases costs, decreases adherence, increases antimicrobial resistance, and enhances the likelihood of adverse drug reactions [4]. In a recent study by Drekonja and colleagues, a longer treatment duration (>7 days) for outpatient men with UTIs are associated with no reduction in recurrence [4]. More studies are needed to determine if greater risk is associated with a shorter duration of treatment. In this study, we aimed to determine if a longer antimicrobial treatment duration (>7 days) for male urinary tract infections in outpatient veterans is associated with a difference in recurrence rates compared to a shorter antimicrobial treatment duration (≤ 7 days).
Methodology
This is a retrospective, single-site, cohort study using clinical data from veterans. The null hypothesis is that there is no difference in urinary tract infection recurrence rates between longer antimicrobial treatment and shorter antimicrobial treatment. The VA Informatics and Computing Infrastructure (VINCI) provide a nationwide view of VA patient data, including the VA’s Corporate Data warehouse containing retrospective medical record data. VINCI personnel identified the cohort of outpatient male Veterans that were diagnosed with a UTI between August 1, 2020 and August 1, 2021. Then, chart reviews were completed on each individual patient to determine if inclusion criteria were met and, if so, to record variables of interest.
We included the following:
• Male veterans within the VA Eastern Kansas Health Care System
• 18 years of age or older
• Prescribed an outpatient antibiotic for a bacterial UTI
• Diagnosed with UTI within the selected time frame
The following are reasons for exclusion:
• Female patients
• Hospital admission
• Multiple/complex bacterial infections
• Multiple antibiotics prescribed at the same time
• Asymptomatic UTI
• Catheter use
• Male urinary conditions that could affect the data such as prostatitis, orchitis or epididymitis
• UTI diagnosed by provider outside VA
• Fungal UTI
During chart review, we collected baseline characteristics such as gender, race, age, height, weight, and serum creatinine. We also collected data on comorbidities that could have the potential to affect UTI recurrence. This includes whether the patient had BPH, diabetes, multiple sclerosis, neurogenic bladder, spinal cord injury, chronic kidney disease, stroke, and dementia. Lastly, we documented their symptoms of UTI, whether they had a previous UTI, the date of the index case and recurrence case and the pathogens if they had micro labs done.
VINCI personnel pulled the initial cohort based on several ICD-10 codes defining urinary tract infection diagnosis (see protocol). During chart review, the first UTI diagnosis within the selected time frame was considered the index case. Then, recurrence of that infection was evaluated. Early recurrence was UTI ≤ 30 days after that index UTI and late recurrence was >30 to ≤ 90 days after the index UTI.
For antimicrobial use, we evaluated the outpatient antibiotic filled within 72 hours of diagnosis of UTI. The number of days the antibiotic was dispensed was considered the treatment duration. Short duration was classified as ≤ 7 days and long duration was classified as >7 days. At times, patients with symptoms of a UTI were empirically prescribed an antibiotic while awaiting confirmatory cultures. Upon return of the culture, the antibiotic was changed if the empirically prescribed antimicrobial was not appropriate. The treatment duration started when the second antibiotic was given. Cases that required more than one antimicrobial prescription were outside our scope of interest for this study. A categorical variable was created to reflect the type of antibiotic used: beta lactams, sulfamethoxazole-trimethoprim, fluoroquinolones, or nitrofurantoin.
Cultures were documented from the index case as well as the recurrent case. If a recurrent case culture was different than the index culture, the patient was considered to have a new infection, not a recurrent one. If a recurrent case culture was not taken, or if no growth was found on either the index culture or recurrent culture, then it was still considered to be a recurrent infection. If the index and recurrent culture was the same, it was also considered to be a recurrent infection.
The primary outcome was to determine if there was a difference between shorter and longer antimicrobial treatment duration when estimating the odds of early and late recurrence of UTI in outpatient male veterans. The secondary outcomes we assessed included the impact of antimicrobial selection on odds of UTI recurrence, evaluating whether predisposing risk factors were associated with UTI recurrence, determining the most common pathogen seen in male patients with UTI and determining the most common antimicrobial used for treatment of index infections in the current sample.
All statistical analyses were completed using SAS Enterprise Guide version 8.2 within the VINCI workspace. Baseline characteristics were evaluated using descriptive statistics. The 2-sided alpha level was set at 5% for significance testing. The primary outcome looking at duration of treatment on UTI recurrence was evaluated using a logistic regression model. For secondary outcomes, a univariate logistic regression analysis was completed evaluating the effect of potential risk factors such as age, BPH, Neurogenic bladder, spinal injury, diabetes, chronic kidney disease, stroke, dementia and history of UTI on both early and late recurrence. A univariate logistic regression analysis was also completed evaluating the effect of antimicrobial selection on early and late recurrence. Only predictors associated with a p-value <0.25 in the preliminary univariate analyses were included in the final multivariate model to avoid overfitting. Correlations between all potential predictors were evaluated to ensure lack of multicollinearity. The other secondary outcomes, related to most frequent pathogen and most frequent antibiotics used, were assessed using descriptive statistics. All patients who met the study criteria were evaluated.
Results
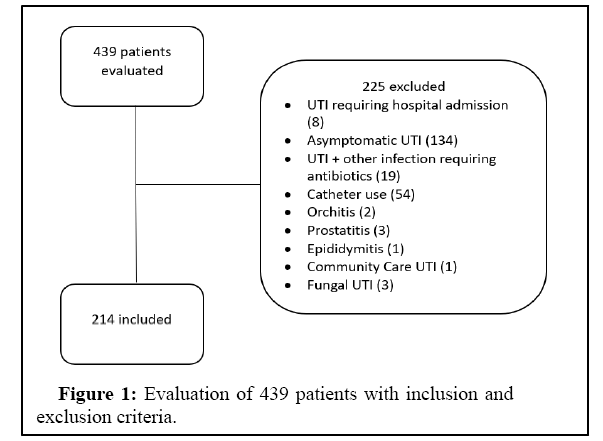
A total of 439 charts were evaluated with 214 meeting the inclusion criteria and 225 meeting exclusion criteria (Figure 1). The main reasons for exclusion were asymptomatic UTI and catheter use. Table 1 demonstrates the baseline characteristics with most patients being white (83.18%) and of advanced age (M=72, SD=12.08). The most common comorbidities seen amongst the study population were BPH (44.39%), diabetes (38.79%) and CKD (26.17%). For preliminary analysis, logistic regression was used to evaluate if antimicrobial selection was associated with early or late UTI recurrence. Through a univariate analysis, we tested beta lactams, sulfamethoxazoletrimethoprim, fluroquinolones and nitrofurantoin to determine if selection of a specific antibiotic class affected recurrence. We planned to include predictors with a P-value<0.25 in the final multivariate analysis model, consistently with common multivariate regression model-building practices [6]. However, all model results were nonsignificant in predicting recurrence. Using the same criteria, we tested the effects of age, BPH, neurogenic bladder, spinal injury, DM, CKD, stroke, dementia and history of UTI to determine if any of these variables had an effect on recurrence. The comorbidities or risk factors that met the P<0.25 threshold for inclusion in the final multivariate analysis model included diabetes on early recurrence (P:0.0286) and history of UTI on late recurrence (P:0.1077). For the primary outcome, duration of treatment on early recurrence (OR 0.660, 95% CI=0.194 to 2.237, P:0.5041) and duration of treatment on late recurrence (OR 0.703, CI=0.251 to 1.969, p 0.5024) were both statistically nonsignificant. Thus, evidence did not support rejecting the null hypothesis. For secondary outcomes, in our final multivariate analysis model, we found diabetes on early recurrence to be statistically significant (OR 0.226, CI=0.058 to 0.882, P: 0.0323). This suggests that patients with diabetes were more likely to experience early UTI recurrence. Our final model also found that history of UTI on late recurrence was statistically nonsignificant (OR 0.346, CI=0.095 to 1.254, P: 0.1061). Patients with a history of UTI prior to the index episode were more likely to have late UTI recurrence. As shown in Table 2, we found the most common index episode pathogen seen was E. coli (43.06%). Post-hoc results are displayed in Table 3 demonstrating that the most common antibiotic used was sulfamethoxazole-trimethoprim (35.51%).
| Race | |
|---|---|
| White | 178 (83.18%) |
| Black | 29 (13.55%) |
| Asian | 1 (0.47%) |
| Unanswered | 6 (2.80%) |
| Age | 72 (SD 12.08) |
| Serum Creatinine | 1.31 (SD 0.84) |
| Height (in) | 70.40 (SD 6.97) |
| Weight (lbs) | 213.03 (SD 52.47) |
| Comorbidities | |
| BPH | 95 (44.39%) |
| Prostate cancer | 5 (2.34%) |
| Neurogenic bladder | 11 (5.14% |
| Spinal cord injury | 5 (2.34%) |
| Multiple sclerosis | 1 (0.47%) |
| Diabetes | 83 (38.79%) |
| Stroke | 16 (7.48%) |
| Dementia | 17 (7.94%) |
| CKD | 56 (26.17%) |
| History of UTI | 132 (61.68%) |
Table 1: Characteristics of the patients.
| Index pathogens | Frequency | Percent |
|---|---|---|
| Actinotignum shaalii | 1 | 0.69% |
| Aerococcus urinae | 4 | 2.78% |
| Alpha hemolytic Streptococcus | 2 | 1.39% |
| Citrobacter koseri | 3 | 2.08% |
| Escherichia coli | 62 | 43.06% |
| Enterobacter | 2 | 1.39% |
| Enterobacter aerogenes | 3 | 2.08% |
| Enterobacter cloacae | 2 | 1.39% |
| Enterococcus faecalis | 14 | 9.72% |
| Gardnerella vaginalis | 1 | 0.69% |
| Klebsiella pnuemoniae | 9 | 6.25% |
| Klebsiella oxytoca | 3 | 2.08% |
| MRSA | 1 | 0.69% |
| Proteus mirabilis | 9 | 6.25% |
| Providencia stuartii | 1 | 0.69% |
| Pseudomonas aeruginosa | 5 | 3.47% |
| Pseudomonas luteola | 1 | 0.69% |
| Serratia marcescens | 1 | 0.69% |
| Staphylococcus aureus | 5 | 3.47% |
| Staphylococcus epidermidis | 11 | 7.64% |
| Streptococcus anginosus | 1 | 0.69% |
| Streptococcus mitis | 1 | 0.69% |
| Streptococcus gallolyticus | 1 | 0.69% |
| Streptococcus agalactiae | 1 | 0.69% |
| Total | 144 |
Table 2: Common index episode of different pathogens.
| ABX | Frequency | Percent |
|---|---|---|
| Beta lactams | 71 | 33.18% |
| Bactrim | 76 | 35.51% |
| Fluroquinolones | 7 | 3.27% |
| Nitrofurantoin | 60 | 28.04% |
Table 3: Demonstration of antibiotics used in patients.
Discussion
In this retrospective study evaluating whether duration (>7 days vs. ≤ 7 days) of antimicrobial treatment affected early and late recurrence, there was no statistically significant difference found. Because these results are nonsignificant, this suggests that it may not be necessary for male patients with UTI to be treated with antimicrobials for duration greater than 7 days. Additional possible benefits of shorter courses of antimicrobial treatment include decreasing adverse drug events, reducing overall cost, preventing antimicrobial resistance, and increasing patient adherence.
Secondary outcomes show that patients with diabetes are at higher risk for early recurrence. This outcome was statistically significant. Urinary tract infections are more prevalent in patients with diabetes for several reasons. Poor metabolic control, impairments in the immune system and incomplete bladder emptying due to autonomic neuropathy may all contribute to the enhanced risk of urinary tract infections in these patients [7]. Clinically, this finding demonstrates the importance of managing and controlling diabetes in patients with recurrent UTI. Additionally, if a patient had a history of UTI, they were more likely to have a late recurrence. If a patient experiences UTI often, for any reason, it is logical that they would have a recurrent infection, even if this finding was not statistically significant. Clinically, it is important to recognize prior UTI history to appropriately identify and treat the underlying cause of recurrent infection. Another finding was the low utilization of fluroquinolones. This is likely because this class of antibiotics are non-formulary; therefore, providers opt for other treatments first.
One strength of this study is that it is real world patient data. Because we are only considering the male population, and the population of military veterans is predominantly male, the use of VA data was considered ideal, producing results about impact of duration of treatment on UTI recurrence in males that are particularly generalizable and have strong external validity. Also, since patient specific information was all collected by chart review, this allowed for consistency within the data collecting process. Additionally, given the sample size achieved through retrospective observational methods, the statistical analyses were adequately powered to test the research questions posed. Lastly, the VA charting system is convenient because all of the patient’s records are in one place meaning we can adequately follow up with them.
One limitation is that this was a geographically limited study and was only completed with VA Eastern Kansas Health Care System patients. Additionally, documentation errors have the potential to limit accuracy and completeness of data for any retrospective chart review study. We also did not assess side effects of the antibiotics to determine whether patients on longer treatment duration experienced increased frequency or severity of adverse drug reactions. Lastly, due to the observational nature of the study design, there may be sources of bias or confounds that weren’t accounted for, and a randomized controlled trial to confirm findings is warranted [8-11].
Conclusion
Longer treatment duration (>7 days) for urinary tract infections in outpatient male veterans is not associated with a difference in early or late recurrence rates compared to shorter antimicrobial treatment duration (≤ 7 days). This finding suggests that male patients should be prescribed shorter courses of antibiotics when treating UTIs. While these results are promising, additional studies, especially prospective randomized controlled trials, are required to confirm these findings.
Please note, this work was supported by VA Eastern Kansas Medical Center and the VA Informatics and Computing Infrastructure (VINCI). The views and opinions of the authors expressed here are not necessarily those of the Veterans Health Administration or the United States Government.
References
- Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ (2015) Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 13:269-284.
[Crossref] [Google Scholar] [PubMed]
- Gupta K, Larissa Grigoryan L, Trautner B (2017) Urinary tract infection. Ann Intern Med 167:ITC49-ITC64.
[Crossref] [Google Scholar] [PubMed]
- Tan CW, Chlebicki MP (2016) Urinary tract infections in adults. Singapore Med J 57:485-490.
- Drekonja DM, Rector TS, Cutting A, Johnson JR (2013) Urinary tract infection in male veterans: Treatment patterns and outcomes. JAMA Intern Med 173:62-68.
[Crossref] [Google Scholar] [PubMed]
- Urinary tract infections: Epidemiology, mechanisms of infection and treatment options
- Zhang Z (2016) Model building strategy for logistic regression: purposeful selection. Ann Transl Med 4:111.
[Crossref] [Google Scholar] [PubMed]
- Nitzan O, Elias M, Chazan B, Saliba W (2015) Urinary tract infections in patients with type 2 diabetes mellitus: Review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes 8:129-136.
- Ahmed H, Farewell D, Francis NA, Paranjothy S, Butler CC (2019) Impact of antibiotic treatment duration on outcomes in older men with suspected urinary tract infection: Retrospective cohort study. Pharmacoepidemiol Drug Saf 28:857-866.
[Crossref] [Google Scholar] [PubMed]
- Ahmed H, Farewell D, Jones HM, Francis NA, Paranjothy S, et al. (2018) Incidence and antibiotic prescribing for clinically diagnosed urinary tract infection in older adults in UK primary care, 2004-2014. PLoS One 13:e0190521.
[Crossref] [Google Scholar] [PubMed]
- Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, et al. (2011) International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 52:e103-e120.
[Crossref] [Google Scholar] [PubMed]
- Trautner BW (2013) New perspectives on urinary tract infection in men comment on “Urinary tract infection in male veterans: Treatment patterns and outcomes” and on “Preoperative urine cultures at a veterans affairs medical center”. JAMA Intern Med 173:68-70.
Citation: Riveland B, Potter E, Gaddy M, Wehrman G (2022) Urinary Tract Infection Duration of Treatment in Male Veterans. J Infect Dis Ther 10:510. DOI: 10.4172/2332-0877.1000510
Copyright: © 2022 Riveland B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2652
- [From(publication date): 0-2022 - Oct 28, 2025]
- Breakdown by view type
- HTML page views: 2204
- PDF downloads: 448