Urinary Incontinence in the Spanish Elderly: Prevalence and Risk Factors
Received: 31-Oct-2017 / Accepted Date: 06-Nov-2017 / Published Date: 07-Nov-2017 DOI: 10.4172/2165-7025.1000371
Abstract
Objective: To define the prevalence of UI in the Spanish elderly population in both sexes, and to identify the possible relationships between physical activity habits, psychosocial variables, and the presence of UI.
Placement: Spain.
Participants: Data were collected from 7,878 people over 60 years of age (age range: 60–89 years). Of these, 57.6% were women and 42.4% were men. The mean age of the sample was 72.2 ± 8.1 years.
Intervention: Personal interviews were conducted to a representative sample of the Spanish population.
Study variables: The presence of UI, the daily physical activity and frequency, psychosocial variables (social class and social and family support), and body mass index.
Results: 12.8% people reported having UI symptoms: with a prevalence of UI of 22.3% for females and 11.2% for males. The data showed the higher age, weight, Body Mass Index, and sedentary lifestyle of the UI patients compared to healthy participants.
Conclusions: A strong relationship was found between elevated BMI, lower socio-familial support, sedentarism and the prevalence of UI. The social class not did not find relevant results.
Keywords: Urinary incontinence; Prevalence; Aged; Risk factors
Introduction
The International Continence Society defines urinary incontinence (UI) as the objectively demonstrable involuntary loss of urine that causes a social or hygienic problem [1]. UI limits autonomy, reduces self-esteem and significantly impairs the quality of life of those who suffer from it [2]. UI affects 25% of the world's population, and this percentage reaches 45% for the female population in some countries [3]. This problem is more frequent in the elderly, especially in women, but it is underestimated and poorly studied [4].
The practice of physical activity (PA) can prevent and treat UI due to its strengthening effect on the abdominal wall and pelvic floor [5]. However, patients with UI are reluctant to practice physical activity (especially in a group) [6], which aggravates and chronicles this problem in a vicious circle.
Studies estimate that the annual expenditure on pharmaceutical treatment of UI in Spain is approximately 210 million euros. Nevertheless, its prevalence is not well established, and patients with this symptomatology request facultative treatment in fewer than 30% of cases [2,7]. These percentages increase even more with age, when UI does not represent a priority in the survival of the elderly [8].
Because prevalence rates are an important factor in the models used to calculate the economic costs associated with UI, this study was designed with the objective of describe the prevalence of UI in the Spanish population and relating it to possible risk factors. To achieve this, as specific objectives were defined: (a) to define the prevalence of UI in the Spanish elderly population in both sexes; and, (b) to identify the possible relationships between PA habits, functional limitations and psychosocial variables, and the presence of UI in the elderly.
Material and Methods
Experimental design
This cross-sectional, observational study was based on data from the European Health Survey of 2014 (EHS14) conducted by the National Institute of Statistics (INE) and the Spanish Ministry of Health, Social Services and Equality. Personal interviews were conducted between January and September 2014 in a representative sample of the Spanish population (n=37,500).
Sample
The EHS14 in Spain included its entire population (46,745,807 people). To obtain a representative sample, the sampling process included all the provinces and was carried out in a stratified manner. Details about the survey can be found on the INE website [9].
Data were collected from 7,878 people over 60 years of age (age range: 60-89 years), resulting in data from a 30-year cohort. Of these, 4,540 (57.6%) were women and 3,338 (42.4%) were men. The mean age of the sample was 72.2 ± 8.1 years: 71.4 ± 7.9 years for the subgroup of men and 72.8 ± 8.2 years for the subgroup of women.
Study variables
Presence of UI: This variable in EHS14 arises through a dichotomous question (yes or no): Do you have urinary incontinence or problems with urine control?
PA habits: Two questions of interest on this subject are asked:
Daily PA: Which of these possibilities best describes your main activity during the day? The response options were (1) sitting most of the day; (2) standing most of the day without major displacement or effort; (3) walking, making frequent trips and (4) performing tasks that require great physical effort.
PA frequency: Which of these options best describes the frequency with which you do PA in your free time? The response options were (1) I do not exercise; (2) I do some PA occasionally; (3) I do PA several times a month; and (4) I train or practice PA several times a week.
Psychosocial variables: In the EHS14, two questions are asked on this topic:
Social class: was based on the occupation of the reference person. This was coded as follows: (1) upper class-directors and managers of companies; (2) middle class-self-employed and qualified technical professionals and (3) low class – unskilled workers.
Social and family support was based on the result obtained through two questions: In your environment, to what extent are you exposed to harassment, discrimination and/or violence? And, if you have a serious personal problem, how many people close to you could you count on? Both had four response options that represented the highest degree of exposure to harassment situations and the number of support people. The answers to both questions were averaged and coded as follows: (1) null or very low support; (2) moderate support; and (3) high social and family support. This coding process is performed by the INE, and the results obtained are already processed in the database provided by that institution.
The independent variables of the study were (a) sex; (b) age (years); (c) weight (kg) and (d) Body Mass Index (BMI). The BMI was calculated based on the participants’ self-reported weight and height. The BMI is divided into four categories: underweight (BMI<18.5 kg/ m2); normal (18.5 kg/m2 ≥ BMI<25 kg/m2); overweight (25 kg/m2 ≥ BMI<30 kg/m2) and obesity (BMI ≥ 30 kg/m2) [10].
Statistical analysis
To characterize the sample, descriptive measures were used (frequency, mean, and standard error). T-tests were used to determine gender differences in continuous variables. The proportionality test was used to test for equality of proportions using statistical measures of large samples. To analyze the association between the dependent and independent variables, a bivariate analysis was performed. The Wilcoxon test was used to compare medians.
A logistic regression model with a dependent variable (presence of UI) and several independent or explanatory variables (BMI, PA habits and psychosocial variables) was applied.
Observations with missing values were automatically discarded by Stata (StataCorp LP, College Station, USA).
All statistical analyses were performed using Stata for Mac, version 12 and a value of p<0.05 was always set as the threshold for statistical significance.
Results
Of the total sample (7,878 people over 60 years of age), 1,012 (12.8%) people reported having UI symptoms. Of these, 638 (63%) were women and 374 (3%) were men. These data imply a prevalence of UI of 22.3% for females and 11.2% for males.
The data highlight the higher age, weight and mean BMI of the UI patients compared to healthy participants (Table 1). These differences between healthy and UI participants were statistically significant for the three variables in the total sample and in a separate analysis of women. However, in men, only age was significantly different.
| Variables | All (n=7.878) | Women (n=4.540) | Men (n=3.338) | |||
|---|---|---|---|---|---|---|
| UI patients | No UI | UI patients | No UI | UI patients | No UI (n=2.964) | |
| (n=1.012) | (n=6.866) | (n=638) | (n=3.902) | (n=374) | ||
| Age (years) | 76.7 ± 7.9 | 71.6 ± 7.9** | 74.8 ± 8 | 72.7 ± 8.2** | 72.3 ± 7.2 | 71.2 ± 7.9* |
| Weight (kg) | 73.2 ± 6.5 | 72.1 ± 6.9* | 70.1 ± 4.5 | 67.3 ± 5.5** | 78.5 ± 7.5 | 78.3 ± 6.9 |
| BMI (kg/m2) | 27.1 ± 2.5 | 26.4 ± 2.7** | 27 ± 3.5 | 26 ± 2.9** | 27.3 ± 3.5 | 26.8 ± 4.5 |
| Physical activity daily [n (%)] | ||||||
| Sedentarism | 690 (68.2) | 2.654 (38.7)* | 468 (73.4) | 1.537 (39.4) | 223 (59.6) | 1.023 (34.5) |
| Walk | 281 (27.7) | 3.262 (47.5) | 153 (24) | 1.925 (49.3) | 108 (28.9) | 1.247 (42.1) |
| Efforts | 41 (4.1) | 950 (13.8) | 17 (2.6) | 440 (11.3) | 43 (11.5) | 694 (23.4) |
| Frequency of physical activity [n (%)] | ||||||
| Never | 630 (62.3) | 2.827 (41.2) | 408 (63.9) | 1.758 (45.1) | 202 (54) | 1.021 (34.4) |
| Occasional | 337 (33.2) | 3.338 (48.6) | 204 (32.1) | 1.784 (45.6) | 150 (40.1) | 1.604 (54.1) |
| Monthly Weekly |
19 (1.9) | 322 (4.7) | 6 (0.9) | 166 (4.3) | 13 (3.5) | 134 (4.5) |
| 26 (2.6) | 379 (5.5) | 20 (3.1) | 194 (5) | 9 (2.4) | 205 (7) | |
*P value<0.05; **P value<0.001
Table 1: Descriptive and comparative analysis between sexes of the independent variables and count of the responses in terms of physical activity habits.
Regarding PA habits, the UI patient group reported a more sedentary lifestyle, especially in women (Table 1). Of the PA habits, the only one that showed statistically significant differences between UI patients and healthy individuals was daily PA in women (p<0.001). No significant differences were found for any of the PA variables neither in men nor in the total sample.
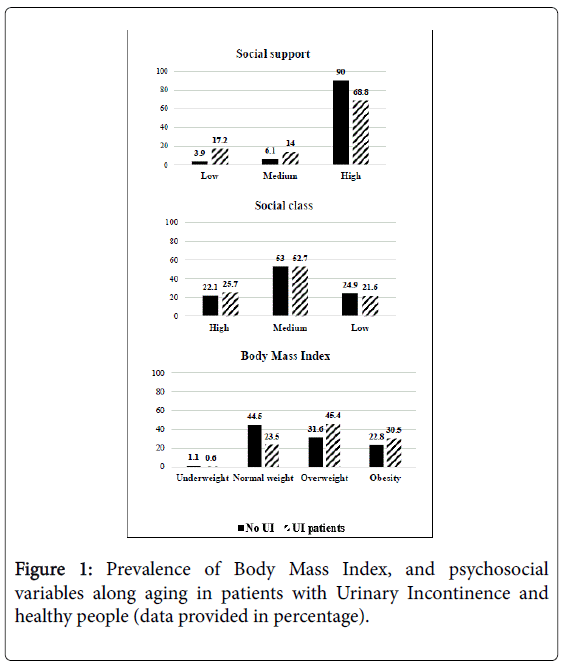
Figure 1 shows the variables of the psychosocial state, social class was very similar for both study groups. However, in perceived social support, differences were found: a UI patient was five times more likely to perceive low socio-family support around them. In parallel, of all asymptomatic individuals, less than 4% did not perceive a good level of socio-family support in their environment. Finally, BMI also showed differences between the two study groups: more than 75% of individuals with UI showed excessive BMI.
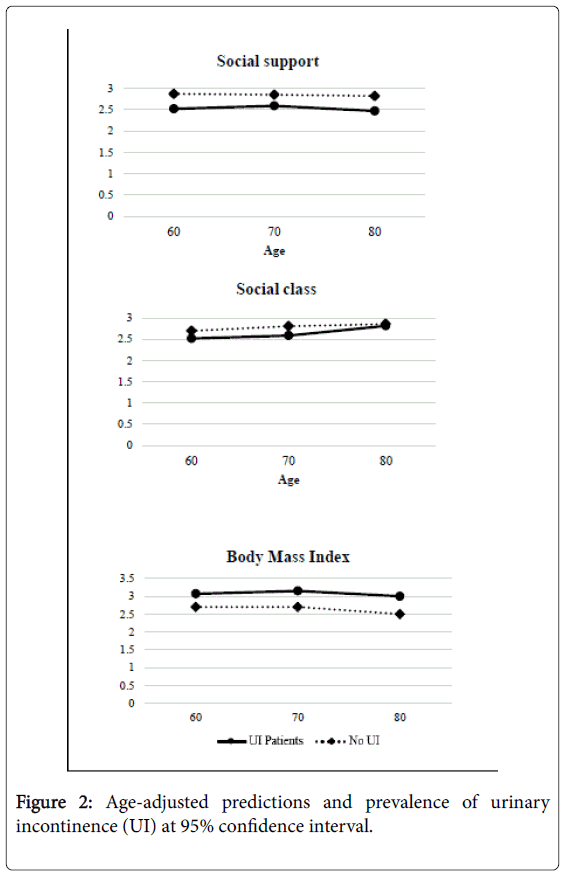
Figure 2 shows the adjusted predictive models for the variable age and prevalence of UI for each study variable. These graphs show that the protective effect of PA is more intense when it is part of the participants' daily lives. Social support was higher in the healthy group and practically constant throughout the aging. However, in the UI group, this was lower and tended to decrease, especially after age 70. It is also observed that the study variable with the worst was social class, which showed very small differences between the two study groups.
Discussion
The objectives of this study were to define the prevalence of UI in the Spanish elderly population in both sexes and to identify the possible relationship between physical activity habits, psychosocial variables, and the presence of UI in the elderly. UI limits autonomy, reduces self-esteem and significantly impairs the quality of life of 25% of the world's population [2,3]. Our results indicate a difference in the prevalence of UI between the sexes, despite their commonalities, such as sedentarism, and perceived lower social support, compared to the elderly incontinent.
Prevalence of UI in the Spanish elderly population
The prevalence rates of UI obtained in this study (12.8% in people older than 60 years) are lower than those reported by previous studies. Among them, Milsom et al. [11] carried out a population study in several European countries, obtaining a total prevalence of 16.6% (ranging from 12% in France and Italy to 18%–19% in Germany, England and Sweden, reaching a maximum of 22% in Spain). Along the same lines, in the United States, was observed an overall prevalence of 16.5% [12]. It should be noted that the published studies on the prevalence of UI in large population groups are outdated (more than 10 years old in most cases). Nevertheless, we can observe a reduction in the incidence of this pathology in general and in the elderly in particular. In contrast, what remains a constant in the prevalence of UI is the higher incidence in women than in men.
In this population, weight and BMI were significantly different between healthy women and those with UI, but the same was not true for males. In addition, the influence of BMI on UI development was identified. This aspect agrees with previous studies, which also detected this association and explored the hypothesis that the physiological basis of the same lies in a chronic increase in the intra-abdominal pressure, which alters the motor control of the pelvic floor and renders it inefficient, allowing the urine to escape [13,14].
Relationships between PA habits, functional limitations and psychosocial variables, and the presence of UI
Regarding PA habits, of the two variables used to asses this behavior, the most important was the activity level during the day (daily PA): it was the only variable that differentiated the group of women with healthy UI and had the greatest negative influence on the development of UI in both sexes in logistic regression analysis. In addition, those who undertook at least occasional PA and walked more than 120 minutes a day also showed a lower incidence of UI. According to data from the last Eurobarometer, the usual practice of PA is much less common in Spain than in central and northern Europe, justifying that between 30% and 40% of the population 65 years of age and older (especially women) present obesity, which justifies and supports our results [15].
In order to understand the origin of these differences between the sexes, beyond the biological conditions that predispose women to the development of UI (mainly previous vaginal births and physiological changes due to the effect of menopause), it is necessary to take into account the social differences between men and women. In this way, at the socio-family level, the female role as the one responsible for family care, coupled with the greater difficulty accessing and controlling economic resources and the inadequate cultural assimilation of aging, make older women a vulnerable group in terms of health [16]. Therefore, it is important to design a specific approach for the detection and treatment of UI in women, such as the development of specific questionnaires that include the evaluation of the level of PA and sexual function, which is often altered as a consequence of pelvic floor dysfunction [17,18]. This is supported by the results obtained regarding psychosocial variables. The perception of social support by the elderly has been one of the most significant variables of this study: showing significant differences between the two study groups and a strong protective effect against the development of symptoms associated with UI throughout aging. However, the social class of the individual did not show any significant effects. That is, independent of social class, the socio-familiar environment of the elderly is a determinant of healthy aging in general and especially of maintaining urinary continence.
A singularity of this study was that the identification of subjects with UI was carried out through personal interviews and in private (to eliminate problems with recognition of the problem on the part of the patient). In addition, the survey question asked whether the respondents had any UI-related symptoms. That is, there was no need for a confirmatory medical diagnosis. This was an important aspect, because it is a problem that many patients do not seek a medical consultation.
However, we also bear in mind the limitations of this work, such as the absence of longitudinal data to observe the medium-and long-term relationship between BMI variation and UI symptoms. Another limitation is the great variability of criteria that can be adopted to define and diagnose UI. This problem was identified by Stewart et al [19] in a literature review that identified 17 studies on the incidence of UI, from which was extracted their methodological characteristics and detailed data on 109 specific incidence rates described by age. Age and definition of IU accounted for 60% of the variation in incidence rates between studies.
The lack of homogeneity in the diagnostic criteria of UI explains the great variability in the incidence estimates. The development of norms for the reporting of prevalence and revision is a premise for the creation of a solid body of evidence on the aetiology and policies of action on UI. A premise on which these standards should be based is to communicate the quantitative criteria of frequency of symptoms (twice or more per month, for example) against indefinite thresholds (never, sometimes, often or always).
Conclusions
In this study of a representative sample of the Spanish population, a strong relationship was found between elevated BMI, lower sociofamilial support and the prevalence of UI. It was also related to attitudinal aspects such as sedentarism, a behavior that predisposes older people to develop UI.
It should be noted that this is the first study to report a reduction in the prevalence of UI in comparison with other studies on the prevalence of this disease. Regardless of these encouraging results, in order to further reduce the number of people affected by UI, it is essential to involve all health professionals in the prevention and identification of all patients.
References
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, et al. (2002) The standardisation of terminology of lower urinary tract function: Report from the standardisation sub-committee of the international continence society. Am J Obstet Gynecol 1: 116-126.
- Freire MM, Cougil MS, Diz PG, Paternain MV, Ramos MB, et al. (2004) Estudio de prevalencia de incontinencia urinaria en mujeres de 18 a 65 años y su influencia en la calidad de vida. At Prim 34: 134-139.
- Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen C, et al. (2014) Global prevalence and economic burden of urgency urinary incontinence: A systematic review. Eur Urol 65: 79-95.
- Norton P, Brubaker L (2006) Urinary incontinence in women. Lancet 367: 57-67.
- Bø K (2004) Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int Urogynecol J Pelvic Floor Dysfunct 15: 76-84.
- Bø K (2004) Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Med 34: 451-464.
- Kirkland VL, Palmer MH, Fitzgerald ST (2001) Incontinence in a manufacturing setting: Women's perceptions and responses. Public Health Nursing 18: 312-317.
- Troko J, Bach F, Toozs-Hobson P (2016) Predicting urinary incontinence in women in later life: A systematic review. Maturitas 94: 110-116.
- Instituto Nacional de EstadÃstica (2014) Encuesta europea de salud en españa: EESE-2014.
- Campillo J, Carmena R, Casanueva F (2000) Consenso SEEDO’2000 para la evaluación del sobrepeso y la obesidad y el establecimiento de criterios de intervención terapéutica. Med Clin 115: 587-597.
- Milsom I, Abrams P, Cardozo L, Roberts R, Thüroff J, et al. (2001) How widespread are the symptoms of an overactive bladder and how are they managed? A population?based prevalence study. BJU Int 87: 760-766.
- Stewart W, Van Rooyen J, Cundiff G, Abrams P, Herzog AR, et al. (2003) Prevalence and burden of overactive bladder in the united states. World J Urol 20: 327-336.
- Hannestad YS, Rortveit G, Sandvik H, Hunskaar S (2000) A community-based epidemiological survey of female urinary incontinence: The norwegian EPINCONT study. J Clin Epidemiol 53: 1150-1157.
- Pavón AG, Chao CW, RodrÃguez NR, Iglesias FJG (2014) Prevalencia y factores de riesgo de incontinencia urinaria en mujeres que consultan por dolor lumbopélvico: Estudio multicéntrico. At Prim 46: 100-108.
- European Comission (2014) Special Eurobarometer 412: Sports and physical activity. European Comission.
- MartÃnez-Torres, JC, Delgado JÃG (2015) Urinary incontinence like health problem in the medium age women. Invest Medicoquir 6: 267-278.
- Mestre M, Lleberia J, Pubill J, Espuña-Pons M (2015) Los cuestionarios en la evaluación de la actividad y función sexual en mujeres con incontinencia urinaria y prolapso de órganos pélvicos. Act Urol Esp 39: 175-212.
- Sánchez BG, Mansilla JR, GarcÃa ADT, López-Arza MG (2014) Eficacia del entrenamiento de la musculatura del suelo pélvico en incontinencia urinaria femenina. Anales Sis San Navarra 37: 381-400.
- Stewart WF, Hirsh AG, Kirchner HL, Clarke DN, Litchtenfeld MJ, et al. (2014) Urinary incontinence incidence: Quantitative meta-analysis of factors that explain variation. J Urol 191: 996-1002.
Citation: Leirós-Rodríguez R, Romo-Pérez V, García-Soidán JL (2017) Urinary Incontinence in the Spanish Elderly: Prevalence and Risk Factors. J Nov Physiother 7:371. DOI: 10.4172/2165-7025.1000371
Copyright: © 2017 Leirós-Rodríguez R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3676
- [From(publication date): 0-2017 - Apr 29, 2025]
- Breakdown by view type
- HTML page views: 2845
- PDF downloads: 831