Pilot Study Open Access
Urban Patient Navigator Program Associated with Decreased Emergency Department Use, and Increased Primary Care Use, among Vulnerable Patients
Garbers S1, Peretz P2*, Greca E2, Steel P3, Foster J4, Nieto A2 and Arkipoff M5
1Heilbrunn Department of Population and Family Health, Mailman School of Public Health, Columbia University, New York, USA
2Ambulatory Care Network, New York-Presbyterian Hospital, New York, USA
3Weill Cornell Medical Center, New York- Presbyterian Hospital, New York, USA
4Columbia University Medical Center, New York -Presbyterian Hospital, New York, USA
5Hospital for Special Surgery, New York, USA
- *Corresponding Author:
- Patricia Peretz
MPH, Manager
Community Health and Evaluation New York-Presbyterian Hospital
622 W. 168th St., New York
VC4-412, USA
Tel: 212-305-4065
E-mail: pap9046@nyp.org
Received date: April 21, 2016; Accepted date: June 07, 2016; Published date: June 15, 2016
Citation: Garbers S, Peretz P, Greca E, Steel P, Foster J, et al (2016) Urban Patient Navigator Program Associated with Decreased Emergency Department Use, and Increased Primary Care Use, among Vulnerable Patients. J Community Med Health Educ 6: 440. doi: 10.4172/2161-0711.1000440
Copyright: © 2016 Garbers S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Receiving non-emergent care in the Emergency Department (ED) setting may disrupt continuity of care, may lead to less effective preventive care, and often contributes to overcrowding. Community Health Worker (CHW)-driven patient navigator programs that connect patients to primary care are a promising approach to enhance quality of care for patients and to reduce preventable ED utilization.
Methods: Between July 2010 and June 2011, CHWs delivered services to 5,154 predominantly Spanishspeaking patients within 3 large, urban EDs. An evaluation was conducted to determine whether patient navigation services were associated with decreased ED visits or increased primary care visits. Clinical and administrative data were used to compare the mean number of visits 12 months before and 12 months after navigation.
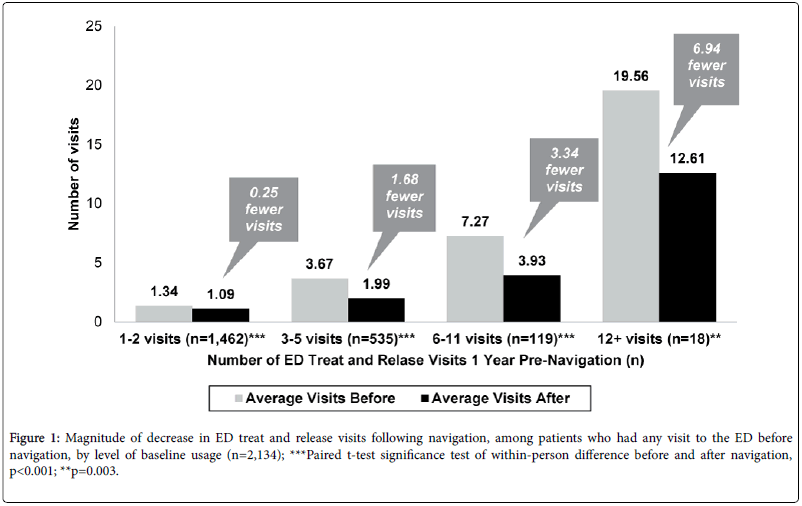
Results: Eighty-six percent of patients who presented without a primary care provider had a primary care appointment scheduled upon discharge. Among patients with 6-11 ED visits prior to navigation (n=119), the mean number of visits dropped from 7.27 to 3.93 (paired t-test p<0.001). These findings persisted after adjustment for potential confounders including insurance type and age group. Increased use of primary care was concurrent with the observed decreased ED use, although a statistical test of the association between these trends was of borderline significance.
Conclusions: In this population of vulnerable patients who received CHW-driven patient navigation, ED utilization decreased after navigation, particularly among those with highest ED usage. Further research is warranted to determine whether connecting patients to primary care is the driving force behind observed reduced ED utilization and to assess whether there is a concurrent effect on hospital admissions.
Keywords
Emergency department; Public health; Community health workers; Patient navigation; Health education; System navigation
Introduction
Receiving non-emergent care in the emergency department (ED) setting may disrupt continuity of care and lead to less effective preventive care and chronic disease management for patients [1]. It also contributes to overcrowding. From 1997 to 2007, annual ED visits increased from an estimated 94.9 million to an estimated 116.8 million, an increase that is almost double what would be expected given population growth [2]; by 2011, visits increased to 136.3 million visits [3]. Since the economic downturn in 2008, much of this increase was driven by visits funded by Medicaid [4]. The resultant crowding, which affects most emergency departments (ED) but particularly those in metropolitan areas [5,6], compromises the quality of care [5,7], increases costs [8,9], delays treatment initiation [10,11], increases length of stay [10] and contributes to lengthening wait times [12].
Several factors contribute to crowding, including a lack of efficient patient movement through the process of care [13], extensive use of ED services by frequent users [8,9,14], and reliance on the ED for nonurgent or ambulatory care sensitive conditions that could be treated in primary care settings [15-17]. Because such lack of timely and effective access to primary care is a key factor in ED usage [16,18-22], numerous policymakers have called for stronger linkage between community-based health care providers and EDs [6,15].
The Patient Protection Act and Affordable Care Act have focused on care coordination with the goal of reducing avoidable ED use and hospital readmissions [10]. In a recent review of ED care coordination literature, 4 out of 7 randomized studies focused on developing a post- ED treatment plan and obtaining appropriate post-ED care were effective in improving follow-up care and reducing repeat ED visits [11-15]. To date care coordination programs have often used intensive case management or relied upon specialized, highly-paid, clinical staff, such as social workers, nurses and physicians [21-24]. There is evidence in the literature that ED-based navigator programs may be effective in increasing usage of primary care services; however, these programs do not always observe a corresponding decrease in ED usage [25].
Community Health Workers (CHWs), who are frontline workers with a strong understanding of the communities that they serve, have been shown to bridge gaps in care by helping patients address specific barriers to health care access leading to reduced disruptions in care and, ultimately, improved health outcomes [26,27]. CHWs in primary care settings have been effective in increasing access to care for underserved populations, leading to reduced ED visits and hospitalizations [25,28]. However, the heterogeneity of outcomes has been cited as a limitation of this evidence base [29,30]. There are few ED-based patient navigator programs led by CHWs; and even fewer have demonstrated effectiveness [31]. To address this gap in the literature, an evaluation of a CHW-driven ED patient navigator program in New York City was conducted to determine whether providing lay patient navigator services in the ED setting led to a decrease in ED utilization or an increase in outpatient primary care utilization (with an affiliated patient-centered medical home program [32]). To provide needed explanatory support for overall findings, the evaluation also examined whether these changes were concurrent.
Methods
Design
This evaluation employed a pre/post design to compare the number of ED treat and release (T&R) visits in the 12 months pre-navigation to the number of T&R visits 12 months post-navigation, for all program participants served between July 2010 and June 2011.
Setting
The Patient Navigator program, established in 2009, was based in 3 (2 adult, 1 pediatric) Northern Manhattan EDs of New York- Presbyterian Hospital (NYP), and was affiliated with 6 Patient Centered Medical Homes (PCMHs) that were formally recognized by the National Committee for Quality Assurance for meeting specific standards around team-based, coordinated, patient-centered care. The community district in which NYP is located (Washington Heights, Inwood, and Marble Hill) is predominantly Hispanic and low-income: in 2013, 72% of residents were Hispanic (of any race) and 14.5% were black, 24.2% of families had income below the Federal Poverty Level, and 38.2% were receiving Supplemental Nutrition Assistance Program benefits [33].
Participants
Patients without a primary care provider, without insurance, or who visited the ED more than 1 time in the preceding 12 months were identified in any one of three ways: via a patient status board, health care team referral or event monitoring software. CHWs working as Patient Navigators (PNs) monitored the ED status board to identify patients who were not commercially insured and who had more than 1 ED visit in the preceding 12 months. Any ED staff member could refer a patient who lacked health insurance or who was in need of a primary care physician. To supplement these referral sources, event monitoring software transmitted an email to the PNs identifying any ED patient discharged from the ED who presented to the ED more than once in the past 12 months or who did not have health insurance.
After patients were identified, the PN contacted the patient to describe the program, to obtain oral consent to receive PN services, and to screen for eligibility. During the study period, there were 80,919 patients who met the criteria to receive PN services, and these patients accounted for 112,825 visits. The 5,154 unique patients who received PN services accounted for 10,116 visits, and the 75,765 patients who did not receive PN services, and who served as a comparison group, accounted for 102,709 visits. The comparison group included individuals who were either not screened by the program or refused PN services. Table 1 presents the characteristics of the navigated patients compared to the characteristics of the non-navigated comparison group. The 5,154 patients who received PN services were given appointments in both the affiliated PCMH network (the PCMH subset, n=1,625) and outside the PCMH network (n=3,529). Analyses of post-navigation visits to a primary care provider outside the PCMH network were not studied as part of this evaluation.
| Characteristic | NavigatedPatients withinPCMH Network (n=1,625) | NavigatedPatients notinPCMHNetwork (n=3,529) | DidnotreceivePN Services (Comparison)1 (n=75,765) | Total (n=80,919) | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | |
| Age group*** | |||||||
| <1 year | 95 | 6 | 101 | 3 | 6,468 | 9 | 6,664 |
| 1-4 years | 93 | 6 | 114 | 3 | 5,852 | 8 | 6,059 |
| 5-14 years | 136 | 8 | 202 | 6 | 9,973 | 13 | 10,311 |
| 15-17 years | 34 | 2 | 81 | 2 | 2,999 | 4 | 3,114 |
| 18-24 years | 165 | 10 | 658 | 19 | 9,585 | 13 | 10,408 |
| 25-34 years | 269 | 17 | 697 | 20 | 11,169 | 15 | 12,135 |
| 35-64 years | 634 | 39 | 1,365 | 39 | 22,517 | 30 | 24,516 |
| 65 years and older | 194 | 12 | 304 | 8 | 7,202 | 10 | 7,700 |
| Hospital*** | |||||||
| Allen Hospital ED | 361 | 22 | 1,174 | 33 | 20,055 | 26 | 21,590 |
| Morgan Stanley Children’s Hospital ED | 364 | 22 | 583 | 17 | 25,153 | 33 | 26,100 |
| NYP Columbia Campus ED | 900 | 55 | 1,772 | 50 | 30,557 | 40 | 33,229 |
| Gender | |||||||
| Female | 904 | 56 | 1,898 | 54 | 41,898 | 55 | 44,700 |
| Male | 714 | 44 | 1,598 | 46 | 33,866 | 45 | 36,178 |
| Primary language** | |||||||
| English | 439 | 27 | 1,003 | 28 | 38,736 | 51 | 40,178 |
| Spanish | 955 | 59 | 1,921 | 54 | 35,342 | 47 | 38,218 |
| Others | 231 | 14 | 605 | 17 | 1,687 | 2 | 2,523 |
| Pay or status*** | |||||||
| Commercial | 114 | 7 | 414 | 12 | 17,092 | 23 | 17,620 |
| Medicaid Fee for Service | 331 | 20 | 597 | 17 | 6,501 | 9 | 7,429 |
| Medicaid Managed Care, Contracted | 538 | 33 | 824 | 23 | 24,078 | 32 | 25,440 |
| Medicaid Managed Care, Non-Contracted | 58 | 4 | 329 | 9 | 5,976 | 8 | 6,363 |
| Medicare Fee for Service | 144 | 9 | 159 | 5 | 5,219 | 7 | 5,522 |
| Medicare Managed Care, Contracted | 51 | 3 | 88 | 2 | 2,164 | 3 | 2,303 |
| Medicare Managed Care, Non-Contracted | 9 | <1 | 31 | <1 | 438 | <1 | 478 |
| Other | 9 | <1 | 27 | <1 | 1,405 | 2 | 1,441 |
| Self-Pay | 371 | 23 | 1,060 | 30 | 12,892 | 17 | 14,323 |
| Missing data not presented 1The comparison group excludes patients with a presenting diagnosis and/or chief complaint of psychiatric and/or substance use conditions; with missing data on presenting diagnosis; or with missing data on discharge disposition information. The comparison group includes patients with psychiatric and/or substance use histories or conditions or that are not the chief complaint or presenting diagnosis, patients with no telephone, and patients who refused PN services; *** Chi-square test p<0.001 for all group comparisons tested (Navigated PCMH vs. Navigated non-PCMH and each navigated group to the comparison group); ** Chi-square test p<0.01 for all group comparisons tested (Navigated PCMH vs. Navigated non-PCMH and each navigated group to the comparison group) |
|||||||
Table 1: Characteristics of Emergency department T&R patients, comparing navigated patients to those who did not receive navigation services.
Intervention
The mission of the PN program was to work alongside the health care team, including providers, nurses, social workers, and care managers, to support patients to best understand, access, and utilize the health care system and to empower patients and their families to achieve optimal care plans. During the study period (July 2010-June 2011), 10 PNs provided an average of 385 hours of service per week, at a total program cost (salary & non- salary) of $950,000.
PN services included culturally sensitive, customized education about how best to access and utilize the health care system, the scheduling of appointments with a primary care provider (for a consultation or follow-up) or specialist; and follow-up to ensure that the patient understood the next steps and that he/she attended the scheduled appointments. Patients received a minimum of 4 contacts by the PN program: initial screening contact, subsequent contact to schedule the required outpatient appointment, a reminder phone call before the appointment, and a follow up phone call after the date of the appointment to determine adherence and, if necessary reschedule a missed appointment.
Patients with health insurance were referred to the primary care provider listed on the patient’s insurance card, unless the patient requested a new primary care provider, or to the required specialist accepting the patient’s insurance plan. Patients without insurance were referred to an internal insurance enrollment program.
Data collection
Data associated with the study group, during the study period, was extracted from the Patient Navigator service program data, patient electronic medical records, and the hospital registration and billing database. PNs collected basic health care data from participating patients, including sociodemographic characteristics (age, gender, primary language); health care access (primary care provider, insurance carrier); the type of navigation services provided, and the associated outcome.
For each patient who received PN services, T&R visit data were exported from the hospital’s clinical-administrative database, including: date, ED location, chief complaint, primary presenting diagnosis, current insurance carrier, and discharge status. In addition, primary care data were exported from the ACN-PCMH database, including date, provider, and current insurance carrier.
For the comparison group, the following variables were exported from the hospital’s clinical-administrative database for all patients with a ED T&R visit during the study period: ED location; age group; gender; primary language; current insurance carrier, primary presenting diagnosis of diabetes, congestive heart failure, or asthma, and discharge status. Only aggregate data associated with comparison group characteristics were used; individually identifying patient information were not provided to the investigators.
The protocol for data collection and analysis was reviewed and approved by the Institutional Review Boards at both Columbia University Medical Center and Public Health Solutions.
Primary outcome
The outcome for the primary study aim was a continuous variable, the mean difference between the number of T&R ED visits in the 12 months prior to the index visit and the number of T&R ED visits in the 12 months after the index visit. This outcome was also operationalized as a dichotomous variable, reduction in ED T&R visits after navigation (yes/no); patients with a mean difference of <0.0 were coded as having the outcome.
Secondary outcome
To support the primary study aim a secondary outcome was calculated: the mean difference between the number of primary care visits within the PCMH network in the 12 months prior to the index visit and the number of primary care visits in the 12 months after the index visit. This outcome was also operationalized as a dichotomous variable, increase in visits within the PCMH network after navigation (yes/no); patients with a mean difference of >0.0 were coded as having the outcome.
Statistical analysis
Data analyses were conducted using STATA 10.1 (StataCorp, College Station, TX). First, tabular analyses were conducted to describe the intervention sample. Then, the characteristics of the comparison sample were tabulated and compared to the intervention sample, with Chi-square (for categorical variables) and ANOVA (for continuous variables) tests of differences between the two groups.
The primary outcome, mean difference in ED visits before and after navigation was calculated, along with standard deviations. Analyses were repeated stratifying by characteristics at the index visit, as operationalized in Table 2, including ED location (CHONY; Milstein; Allen); age group (age <18, age 18 or older); gender; payor status; primary language; access to primary care; and frequency of ED use in the baseline period [34] Finally, the secondary outcome, mean difference with standard deviation in primary care visits before and after navigation was calculated, and stratified by the same subgroups.
To assess independence between changes in ED visits and visits within the PCMH network before and after navigation, the primary and secondary outcomes, using the dichotomous operationalization, were cross-tabulated, and tested for significance using McNemar tests, with alpha set at 0.05. These analyses were restricted to those patients in the PCMH subset with any visits to the ED in the baseline period (n=781); analyses were repeated separating adults (n=543) from children (n=238) [data not shown].
To take into account the possibility that characteristics associated with ED usage may not be independent, binary logistic regression was used to model the dichotomous primary outcome, reduction in treat and release ED visits after navigation, among patients who had any ED treat and release visit prior to navigation (n=2,134). A regression model was run, adjusting for payor status; language; age group; and baseline ED usage. The regression model was repeated among the PCMH subset with any ED visit in the baseline period (n=781 total), adjusting for the same covariates as well as any increase in visits within the PCMH network post-navigation (yes, no [ref.]) [data not shown].
Results
Characteristics of study group
The 5,154 patients who received PN services were predominantly Spanish-speaking adults who were uninsured or insured by contracted Medicaid managed care plans (Table 2). Compared to patients seen in the ED during the same time period who were not in the PN program, navigated patients were statistically significantly older, more likely to have a primary language other than English, and less likely to have commercial insurance.
| Characteristic | N | ED T&R visits before navigation (Mean n) |
ED T&R visits after navigation (Mean n) |
Reduction in visits (Mean n) | |
|---|---|---|---|---|---|
| Overall | 5.154 | 100 | 096 | 004 | |
| Hospital | Allen Hospital ED | 1.535 | 084 | 089 | -006 |
| Morgan Stanley Children’s Hospital ED | 947 | 178 | 135 | 0.42** | |
| NYP Columbia Hospital ED | 2.672 | 082 | 086 | -005 | |
| Gender | Female | 2.802 | 106 | 103 | 003 |
| Male | 2.312 | 093 | 089 | 005 | |
| Age group | Child (age <18 years) | 868 | 174 | 132 | 0.42** |
| Adult (age 18 and older) | 4.286 | 085 | 089 | -004 | |
| Language | English | 1.442 | 109 | 102 | 007 |
| Spanish | 2.876 | 092 | 09 | 002 | |
| Spanish/English equally | 795 | 116 | 108 | 008 | |
| Others | 41 | 027 | 071 | -044 | |
| Payor Status | Commercial | 528 | 069 | 055 | 014 |
| Medicaid Fee for Service | 928 | 086 | 114 | -0.28** | |
| Medicaid Managed Care, Contracted | 1.362 | 146 | 118 | 0.27** | |
| Medicaid Managed Care, Non-Contracted | 387 | 098 | 088 | 011 | |
| Medicare Fee for Service | 303 | 099 | 108 | -010 | |
| Medicare Managed Care, Contracted | 139 | 135 | 132 | 003 | |
| Medicare Managed Care, Non-Contracted | 40 | 053 | 093 | -040 | |
| Other | 36 | 025 | 039 | -014 | |
| Self-Pay | 1.431 | 077 | 076 | 001 | |
| Access to Care | No PCP | 2.416 | 066 | 082 | -0.15** |
| Yes, has PCP, but needs new PCP | 458 | 108 | 087 | 021 | |
| Yes, has PCP, no changes required | 2.258 | 135 | 114 | 0.21** | |
| ED usage at index visit | New user | 3.020 | 0 | 053 | -0.53** |
| 1-2 visits in baseline period | 1.462 | 134 | 109 | 0.25** | |
| 3-5 visits in baseline period | 535 | 367 | 199 | 1.68** | |
| 6-11 visits in baseline period | 119 | 727 | 393 | 3.34** | |
| 12+ visits in baseline period | 18 | 1,956 | 1,261 | 6.94** | |
| Note: Characteristics at index visit (visit at which Navigation services were initiated); PCP=Primary Care Provider; **Paired t-test p<0.001; *p<0.01 | |||||
Table 2: Mean number of treat and release visits to emergency department in 12 month pre-navigation period and 12-month post-navigation period, for all eligible navigated patients, by subgroup characteristics (n=5,154).
Impact on ED utilization
Overall baseline ED utilization was low but there was significant variation in the number of pre-navigation visits by subgroup (Table 3). The majority of adults (n=4,286), (62%) had no ED T&R visits in the year preceding the index visit, but there were some patients who had high usage before navigation: 10% of adult patients (n=430) had 3 or more ED T&R visits before navigation, including 1.4% (n=63) with 6-11 visits in the year before navigation, and a small subset (<1%, or n=13) with 12 or more visits (average of 21.62 visits) in the baseline period [age-group specific data not shown in Table 3].
| Characteristic | N | All patients (N=2,134) | ||
|---|---|---|---|---|
| (N=2,134) | AOR (95%CI) | p-value | ||
| Age group | Age 18 and over (adult) | 1638 | Ref. | --- |
| Age <18 (child) | 496 | 1.07(0.84,1.35) | 0.5927 | |
| Language | English | 604 | Ref. | --- |
| Others | 8 | 1.13(0.26,4.81) | 0.8713 | |
| Spanish | 1132 | 0.94(0.76,1.16) | 0.5597 | |
| Spanish/English equally | 390 | 0.75(0.57,0.99) | 0.0415 | |
| Payor Status | Commercial/Other | 191 | Ref. | --- |
| Medicaid Fee for Service | 337 | 0.64(0.44,0.94) | 0.0241 | |
| Medicaid Managed Care, Contracted | 754 | 0.69(0.49,0.98) | 0.0365 | |
| Medicaid Managed Care, Non- Contracted |
179 | 0.87(0.56,1.35) | 0.5235 | |
| Medicare Fee for Service | 132 | 0.63(0.39,1.02) | 0.0592 | |
| Medicare Managed Care, Contracted | 70 | 1.09(0.59,2.03) | 0.7855 | |
| Medicare Managed Care, Non- Contracted |
12 | 1.02(0.29,3.6) | 0.9728 | |
| Self-Pay | 459 | 0.94(0.65,1.37) | 0.7518 | |
| Baseline ED usage | 1-2 visits in baseline period | 1462 | Ref. | --- |
| 3-5 visits in baseline period | 535 | 2.92(2.3,3.7) | <.0001 | |
| 6-11 visits in baseline period | 119 | 3.10(1.93,4.98) | <.0001 | |
| 12+ visits in baseline period | 18 | 4.21(1.21,14.71) | 0.0243 | |
Table 3: Logistic regression model of a decrease in ED T&R visits from before navigation to after navigation, among eligible navigated patients who had any visit in the ED during the baseline period, total and by age group (n=2,134).
Children (age <18, n=868) had a higher average number of visits in the pre-navigation period than adults (1.74 vs. 0.85 visits), with some subgroups having high average number of visits pre-navigation: infants (age <1 year, 1.94 visits), children age 1-4 (2.29 visits) and children whose index visit was covered by Medicaid managed care (2.14 visits) – the payer source for the index visits of 45% of the children in the sample. More than a quarter of the navigated children had 3 or more ED T&R visits in the year pre-navigation: 21% (n=181) made 3-5 visits, 6% (n=56) made 6-11 visits, and <1% (n=5) children had 12 or more visits [age-specific data not shown in Table 3].
A statistically significant decrease in the average number of ED T&R visits was observed among patients whose index visit was covered by a contracted Medicaid Managed Care plan (1.46 to 1.18 visits, p <0.001) and among children (1.74 to 1.32 visits, p <0.001). Significant decreases were observed for nearly all subgroups of children, particularly subgroups with higher baseline ED visits: children whose index visits were covered by contracted Medicaid managed care (2.14 to 1.52 visits, p<0.001; data not shown in table). Notably, no decreases in ED visits were observed for infants (age <1 year) after navigation (1.94 vs. 1.96 visits, p=0.91; data not shown), but significant decreases were observed for children age 1-4 years (2.29 to 1.55 visits, p <0.001; data not shown).
Substantial, statistically significant decreases were observed among the more frequent users of the ED in the pre-navigation period (Figure 1). Among patients who had any visit to the ED before navigation (n=2,134), the largest reductions in ED visits after navigation were observed among the most frequent baseline users of the ED. Patients who had 3-5 ED T&R visits in the year before navigation (n=535) had, on average, 1.68 fewer visits in the year after navigation; for those with 6-11 visits before navigation (n=119), the average number of visits declined by 3.34 visits in the year after navigation.
Because reductions in ED usage after navigation were observed for some subgroups, including among children, frequent users, and among patients with specific insurance coverage, adjusted analyses were conducted to control for the overlap among these factors (that is, that children had higher levels of baseline usage of the ED, and were more likely to be covered by specific insurance carriers). A logistic regression model was conducted (among all patients who had any visit to the ED before navigation [n=2,134]) to control for these overlapping factors. In the adjusted analyses (Table 3), baseline ED usage remained as the strongest predictor of a decline in ED usage after navigation. In these adjusted analyses, age group was no longer a significant predictor of reduced ED treat and release visits.
Linkage to primary care
Almost all (94%) navigated patients had at least one appointment scheduled by the PN upon discharge (Table 1). Among patients who had no primary care provider (n=2,419), 86% patients had an appointment scheduled with a primary care provider upon discharge and 53% were referred to an internal insurance enrollment resource.
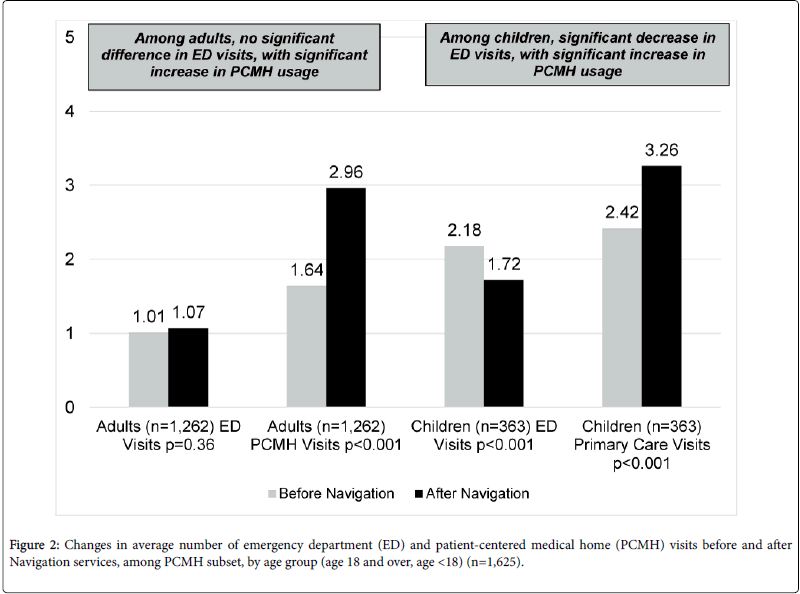
In the subset of patients who were associated with the ACN PCMH network, decreases in ED usage were concurrent with increases in primary care usage in the post-navigation period. As shown in Figure 2, among adults in the PCMH subset (n=1,262), while there was no significant change in ED usage after navigation, the average number of visits in the PCMH network increased (1.64 visits to 2.96 visits, p<0.001). Among children associated with the ACN PCMH (n=363), a statistically significant decrease in average ED T&R visits (from 2.18 visits to 1.72) was concurrent with an increase in primary care visits (from 2.42 visits to 3.26). The independence of these two trends was tested for patients in the ACN PCMH subset who had at least one ED visit in the baseline period (n=781 of the 1,625): In total, 32.9% of the 781 patients had both an increase in primary care visits and a decrease in ED visits; McNemar test, a within-person test of independence, was of borderline statistical significance (p=0.0506).
Discussion
The purpose of this study was to examine the impact of a CHWdriven, ED-based patient navigation program on patient ED utilization. Findings demonstrate that patients who had frequent ED T&R visits before navigation had significantly fewer visits in the year after navigation. Among the 535 navigated patients who had 3-5 ED visits in the year pre-navigation, on average, the number of visits decreased by 1.68 visits in the year after navigation – a difference of 898 visits within this subset alone.
In a subgroup analysis of patients with low access to care, postnavigation decreases in ED T&R visits were not observed. Underinsured patients were not heavy users of the ED before navigation, consistent with findings from other studies [35]. The findings in this evaluation are similar: among both adults and children, those whose index visits were self-pay (not insured), and those who had no primary medical provider all had, on average, less than 1 ED T&R visit in the year before navigation. The navigated patients were linked to primary care, an essential step in addressing gaps in care. Overall, 73% of patients had a visit scheduled with a primary care provider. This is higher than the 51% of patients who were linked to care observed in an ED-based intensive case management program [27].
The observed ED usage decreases were concurrent with increases in usage of primary care within the PCMH, and tests of independence for these two changes were of borderline statistical significance.
Limitations
Despite the promising outcomes associated with the evaluation, and potential for further study, there are some limitations that warrant consideration. First, patients who received PN services are, by definition of the eligibility criteria for the program, systematically different from patients using the ED who do not meet eligibility criteria. By design, the sample (as shown in Table 1 and corresponding technical notes), includes more patients who are uninsured or underinsured, and excludes those patients with certain presenting conditions (including mental illness and substance use diagnoses). In the absence of a randomized control group or a comparison group for whom outcome data were available, the pre/post study design did not mitigate against internal selection bias and subsequent associated patterns such as regression to mean. This analysis relied upon exported clinical and administrative data, and medical data captured in use of administrative databases has been shown to have low reliability [36].
The available data in this study included only the primary presenting complaint diagnosis, not the prevalence of underlying ambulatory care-sensitive medical conditions (such as asthma or diabetes), conditions that, while not representing a large proportion of ED patients, may be most responsive to linkage with a PCMH [37]. The prevalence of PCMH priority presenting primary diagnosis [32] was low: 1% of the sample overall presented with a primary diagnosis of diabetes, <1% for congestive heart failure, and 2-3% for asthma, and there were no significant difference in these presenting diagnoses between those who did and did not receive PN services (data not shown in table). Further investigation is needed to elucidate which subgroups, as defined by health status and morbidity status, can most effectively be served with patient navigation by CHWs and to identify patients who may need more intensive case management.
Despite these limitations, however, the analysis has significant strengths including a large sample size of more than 5,000 patients and broad time period – a full two years of observation for each person in the dataset at three inter-related emergency departments. With the availability of numerous covariates, the analysis was also able to conduct analyses with sufficient statistical power to control for confounding factors such as insurance status, primary language, and age. Most importantly, the present study was able to examine, at the individual level, changes in utilization of both ED and primary care.
Conclusions
The healthcare system can be challenging to navigate for all patient but especially those who are uninsured, living in poverty or have limited English proficiency or limited health literacy [38-42]. CHWs working as PNs in the ED can help bridge gaps in care by working as part of the health care team to provide culturally sensitive support, education, and connections to clinical and social resources for patients who are not well established with primary and specialty care, potentially addressing health care disparities [43-45]. A recent systematic review of interventions to reduce ED utilization found that patient education interventions showed the largest magnitude of effect [46]. The strong effect observed among the patients with highest use of ED care before navigation, an indicator of poor access to care, suggests that programs to link patients who have high ED utilization (regardless of insurance status) show the greatest promise for improving access to care[47].
While the present study found concurrent decreased ED usage and increased usage of primary and specialty care through the affiliated ACN, and statistical testing suggested these two trends may be related, the lack of data on care utilization outside the affiliated network limits the present study’s ability to quantify the extent to which linking patients with primary care was the driving force. Despite this limitation, this study provides promising findings that suggest that a CHW -driven patient navigator program can impact the way that patients utilize the health care system. Given the decreases in ED utilization (particularly among the highest baseline users) observed in a program that deployed lay CHWs and given the dearth of evidence on the cost effectiveness of community health worker interventions future research should quantify the cost effectiveness of such interventions [48].
Funding
This work was supported by funding from The Carson Family Charitable Trust. The authors wish to thank Yuan (Vivian) Zhang, Jimmy Duong, and Ying Wei,PhD at BRIDGE (Biostatistics Resource in Design, Grants, and Evaluation) Program at Columbia University; Dziwe Ntaba, MD; Allison Piazza, MLIS, Weill Cornell Medical College.
References
- Durand AC, Gentile S, Devictor B, Palazzolo S, Vignally P, et al. (2011) ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med 29: 333-345.
- Niska R, Bhuiya F, Xu J (2010) National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. PsycEXTRA Dataset: American Psychological Association (APA).
- Mortensen K (2010) Copayments did not reduce medicaid enrollees' nonemergency use of emergency departments. Health Aff (Millwood) 29: 1643-1650.
- Kamali MF, Jain A, Jain M, Schneider SM (2011) Why Do Patients With Minor Complaints Prefer Emergency Departments Over Primary Care Physicians? Ann Emerg Med 58: S235.
- Gill JM, Riley AW (1996) Nonurgent use of hospital emergency departments: Urgency from the patient's perspective. J Fam Pract 42: 491-496.
- Koziol-McLain J, Price DW, Weiss B, Quinn AA, Honigman B (2000) Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. J EmergNurs 26: 554-563.
- Lowe RA, Localio AR, Schwarz DF, Williams S, Tuton LW, et al. (2005) Association between primary care practice characteristics and emergency department use in a medicaid managed care organization. Med Care 43: 792-800.
- Beal AC, Doty MM, Hernandez SE, Shea KK, Davis K (2007) Closing the Divide: How Medical Homes Promote Equity in Health Care—Results from the Commonwealth Fund 2006 Health Care Quality Survey. The Commonwealth Fund.
- Rhodes KV, Bisgaier J, Lawson CC, Soglin D, Krug S, et al. (2013) Patients who can't get an appointment go to the ER": access to specialty care for publicly insured children. Ann Emerg Med 61: 394-403.
- Thorpe KE, Ogden LL (2010) Analysis & commentary. The foundation that health reform lays for improved payment, care coordination, and prevention. Health Aff (Millwood) 29: 1183-1187.
- Zorc JJ, Scarfone RJ, Li Y, Hong T, Harmelin M, et al. (2003) Scheduled follow-up after a pediatric emergency department visit for asthma: a randomized trial. Pediatrics 111: 493-502.
- Baren JM, Shofer FS, Ivey B, Reinhard S, DeGeus J, et al. (2001) A randomized, controlled trial of a simple emergency department intervention to improve the rate of primary care follow-up for patients with acute asthma exacerbations. Ann Emerg Med 38: 115-122.
- Horwitz SM, Busch SH, Balestracci KM, Ellingson KD, Rawlings J (2005) Intensive intervention improves primary care follow-up for uninsured emergency department patients. AcadEmerg Med 12: 647-652.
- Smith SR, Jaffe DM, Fisher EB Jr., Trinkaus KM, Highstein G, et al. (2004) Improving follow-up for children with asthma after an acute Emergency Department visit. J Pediatr 145: 772-777.
- Katz EB, Carrier ER, Umscheid CA, Pines JM (2012) Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med 60: 12-23.
- Jones JS, Young MS, LaFleur RA, Brown MD (1997) Effectiveness of an organized follow-up system for elder patients released from the emergency department. AcadEmerg Med 4: 1147-1152.
- Shesser R, Smith M, Adams S, Walls R, Paxton M (1986) The effectiveness of an organized emergency department follow-up system. Ann Emerg Med 15: 911-915.
- Francis V, Korsch BM, Morris MJ (1969) Gaps in doctor-patient communication. Patients' response to medical advice. N Engl J Med 280: 535-540.
- Waggoner DM, Jackson EB, Kern DE (1981) Physician influence on patient compliance: a clinical trial. Ann Emerg Med 10: 348-352.
- Fletcher SW, Appel FA, Bourgois M (1974) Improving emergency-room patient follow-up in a metropolitan teaching hospital. Effect of a follow-up check. N Engl J Med 291: 385-388.
- Okin RL, Boccellari A, Azocar F, Shumway M, O'Brien K, et al. (2000) The effects of clinical case management on hospital service use among ED frequent users. Am J Emerg Med 18: 603-608.
- Pope D, Fernandes CM, Bouthillette F, Etherington J (2000) Frequent users of the emergency department: a program to improve care and reduce visits. CMAJ 162: 1017-1020.
- Ferrante JM, Cohen DJ, Crosson JC (2010) Translating the patient navigator approach to meet the needs of primary care. J Am Board Fam Med 23: 736-744.
- Gary TL, Batts-Turner M, Yeh HC, Hill-Briggs F, Bone LR, et al. (2009) The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med 169: 1788-1794.
- Peretz PJ, Matiz LA, Findley S, Lizardo M, Evans D, McCord M (2012) Community health workers as drivers of a successful community-based disease management initiative. Am J Public Health 102: 1443-1446.
- Freeman HP, Rodriguez RL (2011) History and principles of patient navigation. Cancer 117: 3539-3542.
- Carroll JK, Humiston SG, Meldrum SC, Salamone CM, Jean-Pierre P, et al. (2010) Patients' experiences with navigation for cancer care. Patient EducCouns 80: 241-247.
- Thyne SM, Rising JP, Legion V, Love MB (2006) The Yes We Can Urban Asthma Partnership: a medical/social model for childhood asthma management. J Asthma 43: 667-673.
- Swider SM (2002) Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs 19: 11-20.
- Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, et al. (2005) Lay health workers in primary and community health care. Cochrane Database Syst Rev 1: CD004015.
- Enard KR, Ganelin DM (2013) Reducing Preventable Emergency Department Utilization and Costs by Using Community Health Workers as Patient Navigators. J HealthcManag 58: 412-427.
- Carrillo JE, Shekhani NS, Deland EL, Fleck EM, Mucaria J, et al. (2011) A regional health collaborative formed By NewYork-Presbyterian aims to improve the health of a largely Hispanic community. Health Aff (Millwood) 30: 1955-1964.
- Matteoni CA, Wang N, Goldblum JR, Brzezinski A, Achkar E, et al. (2000) Flexible sigmoidoscopy for the detection of microscopic colitis. Am J Med 108: 416-418.
- Byrne M, Murphy AW, Plunkett PK, McGee HM, Murray A, et al. (2003) Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med 41: 309-318.
- Fuda KK, Immekus R (2006) Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med 48: 9-16.
- Grimes DA (2010) Epidemiologic research using administrative databases. ObstetGynecol 116: 1018-1019.
- Adams JG (2013) Emergency department overuse: perceptions and solutions. JAMA 309: 1173-1174.
- Zuckerman S, Shen YC (2004) Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care 42: 176-182.
- Baker DW (2006) The meaning and the measure of health literacy. J Gen Intern Med 21: 878-883.
- Hoffman C, Paradise J (2008) Health insurance and access to health care in the United States. Ann N Y AcadSci 1136: 149-160.
- Morrison AK, Myrvik MP, Brousseau DC, Hoffmann RG, Stanley RM (2013) The relationship between parent health literacy and pediatric emergency department utilization: a systematic review. AcadPediatr 13: 421-429.
- Phelps K, Taylor C, Kimmel S, Nagel R, Klein W, et al. (2000) Factors associated with emergency department utilization for nonurgent pediatric problems. Arch Fam Med 9: 1086-1092.
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J, et al. (2003) Culturally competent healthcare systems: a systematic review. Am J Prev Med 24: 68-79.
- Lowe RA, Fu R, Ong ET, McGinnis PB, Fagnan LJ, et al. (2009) Community characteristics affecting emergency department use by Medicaid enrollees. Med Care 47: 15-22.
- Natale Pereira A, Enard KR, Nevarez L, Jones LA (2011) The role of patient navigators in eliminating health disparities. Cancer 117: 3543-3552.
- Morgan SR, Chang AM, Alqatari M, Pines JM (2013) Non-emergency department interventions to reduce ED utilization: a systematic review. AcadEmerg Med 20: 969-985.
- Gindi RM, Cohen RA, Kirzinger WK (2012) Emergency room use among adults aged 18–64: early release of estimates from the National Health Interview Survey, January–June 2011. National Center for Health Statistics.
- Viswanathan M, Kraschnewski JL, Nishikawa B, Morgan LC, Honeycutt AA, et al. (2010) Outcomes and costs of community health worker interventions: a systematic review. Med Care 48: 792-808.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12963
- [From(publication date):
June-2016 - Apr 10, 2025] - Breakdown by view type
- HTML page views : 11994
- PDF downloads : 969