Review Article Open Access
Updates in Drug Development Strategies against Peptic ulcer
BB Subudhi1*, SP Sahoo2 and PK Sahu1
1School of pharmaceutical Science, Siksha O Anusandhan University, Bhubaneswar, Orissa, 751003, India
2Research Center-II, Aurobindo Pharma Limited, Hyderabad, India
- Corresponding Author:
- BB Subudhi
Associate Professor, Siksha O Anusandhan University School of Pharmaceutical Sciences
School of Pharmaceutical Sciences, Ghatikia, Kalinganagar, Bhubaneswar, 751003, India
Tel: 919853945363
E-mail: bharatbhusans@gmail.com
Received Date: September 16, 2015 Accepted Date: February 26, 2016 Published Date: March 4, 2016
Citation: Subudhi BB, Sahoo SP, Sahu PK (2016) Updates in Drug Development Strategies against Peptic ulcer. J Gastrointest Dig Syst 6:398. doi:10.4172/2161-069X.1000398
Copyright: © 2016 Subudhi BB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Traditional use of antacids and use of histamine inhibitors have become ineffective in the management of peptic ulcer. Irreversible inhibition of proton pump although reduces ulceration, in the long run leads to adverse issues. It has not been possible to develop an ideal proton pump inhibitor. In this scenario, search for alternatives by capitalizing on the multifactorial etiology of ulceration holds promise.
Keywords
Peptic ulcer; Drug development; Therapeutic; Proton pump
Introduction
An ulcer occurring in the lower end of oesophagus, in the stomach usually along the less curvature and in duodenum is known as peptic ulcer or duodenal ulcer. It is associated with symptoms including epigastric gnawing, heart burn, acid eructations, nausea, vomiting, belching, bloating, anorexia, haemorrhage and anaemia.
Peptic ulcer occurs due to an imbalance between mucosal damaging (acid, pepsin) and protecting (mucus, bicarbonate, Prostaglandin E2 and I2) mechanisms. Acid secretion is a physiologically important process of the stomach as gastric acid induces pepsinogen activation to initiate digestive process and kills bacteria and other microbes ensuring a stable intragastric environment [1]. There are three endogenous secretagogues called positive regulators of acid secretion. They are acetyl choline, histamine and gastrin [2-5]. Prostaglandins (PG E2 and I2) act as negative regulators of acid secretion. An imbalance in these regulators leads to peptic ulcer [6]. Another cause of Peptic ulcer is the Helicobacter pylori infection. This infection has no direct role but can induce the immune system which results in superficial gastritis and when it becomes chronic it gradually results in peptic ulcer [7]. The secretion of gastric acid occurs at the level of parietal cells of oxyntic glands in the gastric mucosa, producing 2-3 liters of gastric juice per day (HCl of pH 1). Based on the involvement of multiple factors in peptic ulcer [8], several therapeutic strategies have been adopted against it.
These, include suppression of the aggressive factors with use of antacids, specific antagonists of muscarinic -M1 receptors, gastrin receptors, histamine-H2 receptors, proton pump inhibitors (PPIs), mucoprotective agents, eradication of H. pylori and analogues of prostaglandins. Research for development of antiulcer agent, aims to address one or the other of these issues.
Drugs Reducing Gastric Parietal Cell Stimulation in the Primary Level of Acid Secretion Process
Therapeutic strategy for treating ulcer at the molecular level generally involves reducing acid secretion by inhibiting receptors/ mediators at the initial level, intermediate level and final level of acid secretion. In the initial level, the strategy aims to reduce secretion by preventing stimulation to transmitters including histamine, acetylcholine and gastrin. The intermediate level mainly involves interference on the role of carbonic anhydrase in promoting acid secretion. In the final stage it is the proton pump (H+ K+ ATPase) which has been the target for inhibition to reduce acid secretion.
Acetylcholine inhibitors: Pfeiffer [9] suggested that secretion of acid, mucus and pepsinogen in the gastric mucosal is stimulated via muscarinic receptors. Over expression of M3 receptors in duodenal ulcer patients is proved by autoradiographic techniques; thus blockade of this receptor subtype will reduce the pain by decreasing the duodenal motility and provide an effective anti-secretory therapy. Based on the high affinity to block the muscarinic receptors on the intramural ganglia of stomach wall, pirenzepine was developed as an anti-secretory drug, which was followed by telenzepine, a more potent derivative with improved healing rates [10]. Parasympathetic side effects [11] of these agents include dry mouth, blurred vision and constipation. These side effects along with their incomplete inhibition of gastric acid secretion limit their clinical utility.
Histamine inhibitors: H2 receptor antagonists competitively inhibit the interaction of histamine with H2 receptors, thereby reducing both volume and H+ ion concentration of the gastric juice. They are selective and have little or no effect on H1 receptors. They also inhibit acid secretion elicited by gastrin, muscarinic agonists, food, sham feeding, fundic distension, as well as, other pharmacological agents. They also inhibit basal and nocturnal acid secretion. This effect contributes in a major way to their clinical efficacy. Black et al. [12] identified H2-receptor and prototype H2-receptor antagonist, burimamide. The potency of burimamide at inhibiting gastric acids secretion far exceeded than that produced by anticholinergic drugs and was devoid of side effects. However, it had poor bioavailability which was subsequently replaced by metiamide [13] which also because of its side effects like agranulocytosis, was withdrawn from the clinical trials. Price [14] reported cimetidine as the third H2 receptor antagonist to be tested in humans and was similar to metiamide in its pharmacological profile, but did not cause agranulocytosis. Discovery of this molecule reduced the necessity of surgical procedures for peptic acid diseases. Further, ranitidine [15] was introduced as more potent drug in 1981 with a much superior safety profile. Third and most potent antagonist was famotidine available for clinical use, being 20-50 times more potent than cimetidine and 6-10 times more potent than ranitidine [16]. It was also used once daily. Roxatidine reported by Pioch [17] and Nizatidine reported by Berardi [18] followed famotidine. Each of these drugs are rapidly absorbed and eliminated after oral administration.
H2 receptor antagonists are generally extremely safe drugs with incidence of adverse effect of cimetidine less than 3%. Adverse effects include dizziness, nausea, skin-rashes, somnolence, confusion, impotence, gynecomastia, hematological effects and altered function of immune system. Rarely may they cause bone marrow depression, hepatitis, and anaphylaxis. However in chronic as well as acute cases of ulceration, their effectiveness is far from satisfactory. Because of this they are increasingly replaced by proton pump inhibitors.
Gastrin inhibitors: Gastrin is a peptide hormone that stimulates secretion of gastric acid (HCl) by the parietal cells of the stomach and aids in gastric motility. It is released by G cells in the pyloric antrum of the stomach, duodenum, and the pancreas. Gastrin binds to cholecystokinin B receptors to stimulate the release of histamines in enterochromaffin-like cells, and it induces the insertion of K+/H+ ATPase pumps into the apical membrane of parietal cells and releases acid into the stomach [19]. Gastrin stimulated acid secretion is inhibited by gastric inhibitory peptide (GIP), secretin, somatostatin, glucagon, calcitonin. Somatostatin is a potent inhibitor of gastrinstimulated acid secretion by activation of somatostatin receptor type 2 (sst2) in vivo, probably in part by blocking gastrin-stimulated histamine release from enterochromaffin-like cells expressing sst2 [20]. Cholecystokinin (CCK) inhibits gastrin secretion independently of paracrine somatostatin secretion [21].
Drugs Reducing Carbonic Anhydrase (CA) Activity in the Intermediate Level of Acid Secretion
The involvement of CA I and CA IV in gastric acid secretion, effect of CA inhibitors in reducing HCl secretion and their healing effect on gastric and duodenal ulcers is well documented [22]. In vivo results, performed in humans, show that omeprazole inhibits not only H+/K+ ATPase, but also CA II and CA IV, isozymes present in large quantities in the cytosol, in the walls of the secretory canaliculi, and in the parietal cell membrane. Further, gastric acid secretion is inhibited in humans after oral administration of acetazolamide in therapeutic doses of 25 mg/kg of body weight [23]. Acetazolamide exhibit antiulcer action in acute experiments because of inhibition of CA-II, but its effect on Gastric ATPase is not clear.
Sulfonamides with the general formula RSO2NH2 constitute a wide class of inhibitors of the zinc enzyme carbonic anhydrase (CA). Acetazolamide, a classic sulfonamide drug has also been reported to reduce gastric acid secretion commensurate with gastric carbonic anhydrase inhibition [23]. Correlating in vivo results with the data obtained in vitro suggests that gastric mucosa CA I, II, and IV inhibition is induced by sulfenamide, the active form of omeprazole. Thus this class of compound can be interesting leads for further exploration of anti ulcer action.
Drugs Inhibiting Gastric ATPase in the Final Level of Acid Secretion
Proton pump is the ultimate mediator of gastric acid secretion by parietal cells [24]. With the identification of H+/K+-ATPase as the primary gastric proton pump, it was proposed that activation of H+ secretion occurred by incorporation of H+/K+-.
ATPase rich tubulovesicles into the apical plasma membrane and the pumps were re-sequestered back into the cytoplasmic compartment on return to the resting state. Currently this is achieved by blocking the irreversible H+/K+-ATPase inhibitors, popularly referred as Proton Pump Inhibitors (PPIs). They bind to the gastric proton pump on the parietal cell membrane, inhibiting the release of hydrogen ions from the parietal cells into the lumen of the gastric glands and hence stomach.
Inhibition of H+/K+-ATPase as a means of controlling gastric pH has attracted considerable attention in recent years with the discovery of benzimidazole sulfoxide class of antisecretory agents. Timoprazole, as one of the first well-defined inhibitor of gastric proton pump [25], which was followed by more potent picoprazole and omeprazole [26]. Chemically, the basic structure consists of substituted benzimidazole ring and a substituted pyridine ring connected to each other by a methylsulfinyl chain. Clinically used PPIs include Omeprazole, Lansoprazole, Rabeprazole, Pantoprazole and Esomeprazole. Irreversible inhibition of H+/K+-ATPase occurs following acid activation of these compounds within the acidic compartments in the parietal cells and covalent binding, with C813 residue of gastric H+/K +-ATPase [27]. The draw backs relating to use of irreversible proton pump inhibitors includes extreme acid suppression sometimes leads to achlorohydria at recommended doses and that may produce enteric infections like typhoid, cholera, and dysentery [28]. Significant drug interactions can lead to decreased absorption of some drugs like griseofulvin, ketoconazole, vit.B12, iron salts. Other side effect includes abdominal pain, diarrhea, nausea, and headache. Acute interstitial nephritis progressing to acute renal failure has also been reported to be associated with the use of PPIs. Prolonged inhibition of gastric acid secretion has been associated with the formation of precancerous changes in human gastric mucosa and gastric carcinoids in long term animal studies.
So the research efforts are currently targeting to obtain reversible proton pump antagonists. Imidazopyridine based compound SCH28080 was the prototype of this class and the anti-secretory effect of this compound is mediated through gastric proton pump [29]. SCH 28080 is a protonable weak base (pKa -5.6); hence like omeprazole it accumulates in the acidic compartments of the parietal cells in its protonated form. SCH 28080 is chemically stable even after protonation, is itself active and does not need an acid-induced transformation, as required by omeprazole and its congeners [30,31]. SCH28080 binds non- covalently with gastric H+/K+-ATPase but was withdrawn due to serious hepatotoxicity.
Drugs with other Mode of Action
Antacids: Naturally occurring carbonates, potash, bismuth were used as antacids more than century ago [32]. Since then, they have been developed and are currently widely used. Antacids neutralize HCl to form water and carbon dioxide. Hydroxides of aluminum and magnesium are the most common constituents of antacid preparations. Sodium bicarbonate, calcium carbonate are also used with silicates and phosphates. Simethicone, a surfactant that may decrease foaming and thus, esophageal reflux, is part of many antacid preparations. However, use of antacid is limited to acid neutralization only and does not affect hyper acid secretion. Besides they suffer from other limitations. Sodium bicarbonate, which is used as a systemic antacid causes alkalosis. Magnesium, aluminum and calcium salts act locally and are less likely to develop alkalosis, but magnesium salts cause diarrhea, whereas aluminum and calcium salts cause constipation
Anti H. pylori drugs: H. pylori are a gram-negative rod shaped bacilli that colonizes in the mucus on the luminal surface of gastric epithelium H. pylori infection causes inflammatory gastritis and is a putative contributor to peptic ulcer disease, gastric lymphoma and adenocarcinoma. Infection may not always be causative as ulcers may recur in patients who have undergone successful eradication treatment. Double or triple antimicrobial therapies, in combination with antisecretory drugs, are useful against H. pylori infection and associated peptic ulcers. Bismuth compounds are also been included in regimen probably due to their cytoprotective action. Triple therapy with metronidazole, a bismuth compound and either tetracycline or amoxicillin for two weeks is recommended to treat H. pylori infections. However, the therapeutic limitations of this triple therapy include complex regimen and related nausea, diarrhea and dizziness [33].
Prostaglandin analogues: There are a number of prostaglandin analogues like arbaprostil, enprostil, misoprostol, rioprostil and trimoprostil. They are inferior to H2-receptor antagonists as regards their effects on ulcer healing, pain relief, and relapse prevention and less effective than expected from their acid inhibitory action. They also possess cytoprotective property. They may prove useful as replacement therapy in patients requiring nonsteroidal antiinflammatory drugs [34].
Mucoprotectives: Sucralfate, a basic aluminum salt of sucrose, was the first successful drug with a major cytoprotective mechanism of action. It binds bile acids and pepsin and adheres to both ulcerated and nonulcerated mucosa. Sucralfate stimulates the synthesis and release of gastric mucosal prostaglandins as well as bicarbonate and the epidermal growth factor which stimulates healing. Sucralfate is the safest drug available today in the treatment of dyspeptic symptoms [35]. Bismuth therapy has shown efficacy against two major gastrointestinal disorders: peptic ulcer disease and diarrhea. In peptic ulcer disease it is as effective as the H2-receptor antagonists, costs considerably less, and offers a lower rate of relapse. When Helicobacter pylori are implicated, bismuth acts as an antimicrobial agent, suppressing the organism but not eliminating it. In recent studies, bismuth compounds have been used with conventional antibiotics, producing elimination of the organism, histological improvement, and amelioration of symptoms for periods longer than one year [36].
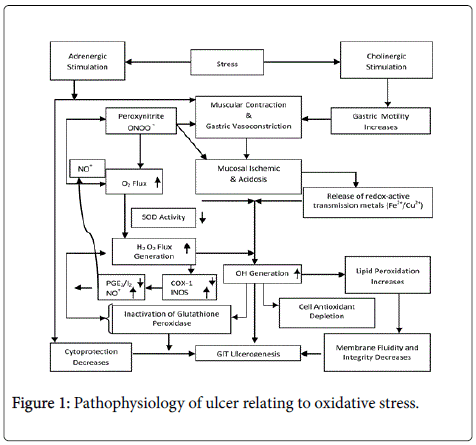
Stress modulators: Stress causes both sympathetic and parasympathetic stimulation of stomach leading to local hypoxia (near or actual “ischemia”). The ischemic condition caused an increase in the levels H2O2 which in conjugation with O2 generates OH–ions which oxidized various cellular constituents such as proteins, membrane lipids and depletes glutathione. Lipid peroxidation causes loss of membrane fluidity and loss of cellular function [37]. Present studies have implicated the role of free radicals on lipid peroxidation in the development of ulcer [38].
Natural products: Wide research has been undertaken in order to establish natural product as stress modulators against ulceration. Treatment with ethanolic extract of seeds of E. jambolana significantly decreased the LPO levels of gastric mucosa against CRS-induced changes in LPO in rats [39]. The phenolic compound rosmarinic acid from Rosmarinus officinalis Linn has shown therapeutic potential in treatment of peptic ulcer disease [40]. The protective effect of liquorice and its derivatives including deglycyrrhized form was reported by Dehpour et al. [41]. The preventive effect of natural xanthanolides on ulcer formation in rats was confirmed by Favier et al. [42]. Solon, a synthetic isoprenyl flavonoid derived from sophoradin from the root of an ancient Chinese plant Sophora tonkinensis, administered orally to rats prevented dose-dependently the formation of acute gastric lesions [43]. Aparisthman from Aparisthmium cordatum reduced significantly the formation of gastric lesions as well as volume of gastric juice as compared with control in the pylorus-ligature model [44]. Although the mechanism underlying this anti ulcerogenic effect of antioxidants remains unknown, it seems to be related to an increase of the defensive mechanisms of the stomach and acting as scavengers against free radicals and prevention of lipid peroxidation.
Free radicals, especially reactive oxygen species in living cells leads to pathogenecity of various diseases including hepatic diseases, cardiovascular diseases, atherosclerosis, diabetes, cancer and ulcers in gastrointestinal tract. Figure 1 explains the pathogenesis of ulcer stimulation due to activation of free radicals. Due to increased lipid peroxidation mucosal cell integrity decreases leading to ulcerogenesis in GI tract. Several works have been reported where natural products with good antioxidant action have shown strong antiulcer activity. Although these reports do not elucidate the mechanism, a holistic approach is believed to explain those findings.
Amino acids: Amino acids (AAs) make up 75% of the human body which are essential to nearly every bodily function. Every chemical reaction that takes place in a human body depends on AAs and the proteins that they build and these are typically found as components in human peptides and proteins. In addition to combining to form the body's proteins, some amino acids act as neurotransmitters or as precursors of neurotransmitters, the chemicals that carry information from one nerve cell to another. Certain amino acids are thus necessary for the brain to receive and send messages. Amino acids also enable vitamins and minerals to perform their jobs properly.
L-serine inhibits gastric secretion and protects the gastric mucosa against stress and chemically induced ulcers [45]. Pretreatment with serine attenuated the formation of stress, indomethacin and necrotizing agents-induced gastric lesions. Glycine, a neutral amino acid has been reported to inhibit gastric secretion and to protect the gastric mucosa against chemically and stress-induced ulcers in rats [45]. L-glutamic acid (0.1 M) administered to the blood also produces marked inhibition of gastric secretion. Pretreatment with L-arginine markedly reduces the degree of gastric injury. It elevates NO bioavailability in the gastric mucosa, which is a gastric mucosal protective factor that contributes significantly to maintaining normal gastric mucosal integrity [46]. The effectiveness of simple and mixed copper (II) complexes of L-tryptophan and L-phenylalanine on the gastric acid secretion was reported in Shay rats by Alberghina [47]. The gastric inhibitory effect of melatonin and L-tryptophan on ulcer healing was accompanied by a significant rise in the gastric blood flow at ulcer margin and an increase of plasma melatonin, luminal NO2–/NO3– and plasma gastrin levels [48]. Gastric acid and pepsin outputs were significantly inhibited during the ulcer healing in melatonin-treated gastric mucosa.
Intraduodenal administration of mixed AA solution resulted in significant inhibition of gastric acid secretion and gastrin release stimulated by intragastric perfusion of peptone [49]. L-tryptophan has a positive effect on gastric mucosal damage in ischemia-reperfusion injury by inhibition of free oxygen radicals [50]. Intestinal infusion of leucine augments the maximal gastric-acid secretory response to pentagastrin and serves as a bioassay for intestinal-phase acid secretion [51]. The mechanism of leucine-stimulated acid secretion involves its ability to alter tyrosine absorption. Intravenous tyrosine infusion also decrease acid secretion in response to intestinal leucine but required much higher dose. Tyrosine exerts a specific inhibitory effect on leucine-stimulated acid secretion, which is mediated intraluminally. The mechanism of leucine-stimulated acid secretion may involve modulation of the sympathetic nervous system, thereby affecting acid secretion as it is a regulator of adrenergic nervous system.
Calcium channel blockers: Hypercalcaemia is associated with increased gastric acid secretion and calcium appears to be critical for stimulus secretion coupling in gut [52].The release of Histamine, acetyl choline, gastrin and hydrochloric acid are all calcium dependent [53]. Histamine release dependent upon both extracellular and intracellular calcium indicates development of gastric ulcer is calcium dependent process. Calcium channel blockers verapamil and its analogues verapamil (desmethoxyverapamil) and gallopamil (methoxyverapamil) prevented ulcer genesis induced by cold-restraint stress and promoted spontaneous ulcer healing [54]. Nitrendipine, diltiazem and verapamil, three chemically-distinct calcium channel blockers, all reduce coldrestraint stress gastric lesions [52]. Nitrendipine significantly decreased stress-induced gastric lesions, but was far less efficacious against 100% ethanol-induced lesions [52]. The anti-ulcer effects of nitrendipine were not reversible with indomethacin, sodium meclofenamate or Nethylmaleimide. Nitrendipine also significantly reduced basal gastric acid output. Verapamil significantly reduced stress lesions in an indomethacin and meclofenamate-reversible manner. Verapamil also decreased basal acid secretion.
Gastric stimulation results in increased calcium influx which can be blocked by calcium antagonist not by Histamine (H2) blockers [55]. Verapamil inhibited acid secretion from isolated parietal cells under basal, histamine and dibutyryl cyclic AMP stimulated condition [56]. Calcium channel antagonists also block the acid secretion by inhibiting parietal cell H+-K+-ATPase. The influence of verapamil on stress and bethanechol induced gastric effects in rats, showed a dose dependent decrease in gastric glandular secretion and also increased gastric wall contraction [57].
The prevention of transmembrane calcium influx which results in inhibition of smooth muscle contraction appears to block histamine and 5-hydroxytryptamine release from stomach wall mast cells. Stress ulcer antagonism by verapamil is associated with inhibition of gastric glandular mucosal mast cell degranulation and reduced stomach contractions. The Combined Cholinergic, gastrinergic and histaminergic influence results on M1 (neuronal) and M2 (Parietal), gastrin and histaminic H2 receptors respectively leading to reduced stimulation of H+/K+ ATPase exchange pump which involved in the terminal step of hydrochloric acid secretion [58].
The effect of nifedipine and cimetidine on cold or stress-induced gastric ulcers and glandular wall mast cell count were studied in rats [59]. Nifedipine in three doses (1, 5 and 10 mg/kg) administered intra peritonealy prevented gastric ulceration and mast cell degranulation. This was attributed to inhibition of histamine stimulated acid secretion and ability to reduce acetyl choline induced gastric secretion in which calcium is the most likely final common denominator.
Considering the multiple etiology involved in peptic ulcer, we have earlier reported molecular hybrids of calcium channel blockers and carbonic anhydrase inhibitors with amino acids [60-64]. These molecules showed significant antiulcer action. Although their exact mode of action is yet to be elucidated multiple mechanisms including proton pump inhibition was demonstrated.
In spite of the progress in understanding the etiology of ulcer, the attempts at developing ideal antiulcer agents are far from successful. Ideally, antiulcer agents should reversibly reduce acid secretion without any adverse effect. Additionally, it may have capacity to neutralize hyperacidity and attenuate infection due to H.Pylori . Besides, it should be safe for long-term use without any risk of developing drugdependency. There are many issues that need to be addressed based on the basic pathophysiology of ulceration. Although the agents discussed have shown potential, none of them has till date matched the effectiveness of omeprazole and its analogues. However omeprazole and its analogues bind covalently and irreversibly inhibit gastric ATPase up to 16-18 hrs following a single dose. Normalization usually takes about 96 hours. This makes them unsuitable for long term use. Besides long term use is associated with risk of drug-dependency. Attempts at finding suitable alternative are far from over. Thus considering, ever increasing incidences of ulcer and ulcer leading to cancer, there is an urgent need to attempt to develop alternative agents to them.
Conclusions
The growth of peptic ulcer disease with time is complex and interesting. Although its incidences were rare before 1800 century, with time and change in life style its incidences have increased significantly. Several therapeutic strategies have evolved over time for its management. However, considering the involvement of multiple factor in its etiology, it has not been possible to provide an ideal solution to completely cure its occurrence. Traditional use of antacids and use of histamine inhibitors have become insufficient in the management of peptic ulcer. Irreversible inhibition of proton pump although reduces ulceration, in the long run leads to adverse issues. It has not been possible to develop an ideal proton pump inhibitor. In this scenario, search for alternatives by capitalizing on the multifactorial etiology of ulceration holds promise. However, these searches are far from over and require further investigations to develop ideal antiulcer agents.
References
- Herling AW, Weidmann K (1996) Burger’s Medicinal Chemistry & Drug Discovery. Vol2. (5th edn) John Wiley and Sons Inc., New Jersey.
- Code CF (1956) Histamine and gastric secretion. Little Brown & Co, New York.
- Uvnas B (1942) The part played by the pyloric region in the cephalic phase of gastric secretion. ActaPhysiolScand 4: 13-18.
- Sandvik AK, Waldum HL (1991) Aspects of the regulation of gastric histamine release. Scand J GastroenterolSuppl 180: 108-112.
- Welsh NJ, Shankley NP, Black JW (1994) Comparative analysis of the vagal stimulation of gastric acid secretion in rodent isolated stomach preparations. Br J Pharmacol 112: 93-96.
- Nelson WL (2005) In Foye’s Principles of Medicinal Chemistry, (5th edn), Lippincott Williams Wilkins: Batlimore.
- Wang AY, Peura DA (2011). The prevalence and incidence of Helicobacter pylori-associated peptic ulcer disease and upper gastrointestinal bleeding throughout the world. Gastrointestinal endoscopy clinics of North America 21: 613–35
- Brunton LL (2001) Goodman &Gilmann’s The Pharmacological Basis of Therapeutics. (10th edn), McGraw-Hill, New York.
- Pfeiffer A, Krömer W, Friemann J, Ruge M, Herawi M, et al. (1995) Muscarinic receptors in gastric mucosa are increased in peptic ulcer disease. Gut 36: 813-818.
- Dammann HG, Dreyer M, Wolf N, Muller P, Merk-Hartlet B,et al. (1989) Single evening administration of a new antimuscarinic agent telenzepine in therapy of acute duodenal ulcer, Results of a randomized double-blind comparative study versus pirenzepine. Zeitschrift fur Gastroenterologie 27: 203-206.
- Lazzaroni M, Sangaletti O, Parente F, Imbimbo BP, Bianchi Porro G (1986) Inhibition of food stimulated acid secretion by association of pirenzepine and ranitidine in duodenal ulcer patients. Int J ClinPharmacolTherToxicol 24: 685-688.
- Black JW, Duncan WA, Durant CJ, Ganellin CR, Parsons EM (1972) Definition and antagonism of histamine H 2 -receptors. Nature 236: 385-390.
- Wyllie JH, Hesselbo T, Black JW (1972) Effects in man of histamine H 2 -receptor blockade by burimamide. Lancet 2: 1117-1120.
- Price BJ, Clitherow JW, Bradshaw J (1978) US Patent 4128658, ChemAbstr 88, 190580.
- Roberts S, McDonald IM (2003) Burger’s Medicinal Chemistry & Drug Discovery. Vol 4 (6th edn), John Wiley and Sons Inc., New Jersey.
- Hirata YO, Yanagisawa I, Ishii YO, TsukS, Noriki T, et al. (1981) MUS 4283408, ChemAbstr 94: 139794.
- Pioch RP EP 49: 618-1985.
- Berardi RR, Tankanow RM, Nostrant TT (1988) Comparison of famotidine with cimetidine and ranitidine. Clin Pharm 7: 271-284.
- Dockray GJ (2004) Clinical endocrinology and metabolism. Gastrin. Best Pract Res ClinEndocrinolMetab 18: 555-568.
- Lloyd KC, Amirmoazzami S, Friedik F, Chew P, Walsh JH (1997) Somatostatin inhibits gastrin release and acid secretion by activating sst2 in dogs. Am J Physiol 272: G1481-1488.
- Schmidt PT, Hansen L, Hilsted L, Holst JJ (2004) Cholecystokinin inhibits gastrin secretion independently of paracrine somatostatin secretion in the pig. Scand J Gastroenterol 39: 217-221.
- Puscas I, Coltau M, Baican M, Domuta G (1999) Omeprazole has a dual mechanism of action: it inhibits both H+K+ATPase and gastric mucosa carbonic anhydrase enzyme in humans (in vitro and in vivo experiments). The Journal of Pharmacology and Experimental Therapeutics 290: 530–534.
- Puscas I, Coltau M, Baican M, Domuta G (1999) A new concept regarding the mechanism of action of omeprazole. Int J ClinPharmacolTher 37: 286-293.
- Okamoto CT, Forte JG (2001) Vesicular trafficking machinery, the actin cytoskeleton, and H+-K+-ATPase recycling in the gastric parietal cell. J Physiol 532: 287-296.
- Ruwart MJ, Nezamis JE, Rush BD, Lancaster C, Davis JP, et al. (1984) Timoprazole is a unique cytoprotective agent in the rat. Digestion 30: 33-40.
- Lindberg P1, Brändström A, Wallmark B, Mattsson H, Rikner L, et al. (1990) Omeprazole: the first proton pump inhibitor. Med Res Rev 10: 1-54.
- Ife RJ, Dyke CA, Keeling DJ, Meenan E, Meeson ML, Person ME, Price CA, Theobald CJ, Underwood AH (1989) 2-[[(4-Amino-2-pyridyl)methyl]sulfinyl] benzimidazole H+/K+-ATPase inhibitors. The relationship between pyridine basicity, stability, and activity. J Med Chem 32:1970-1977.
- Jain KS1, Shah AK, Bariwal J, Shelke SM, Kale AP, et al. (2007) Recent advances in proton pump inhibitors and management of acid-peptic disorders. Bioorg Med Chem 15: 1181-1205.
- Chiu PJ, Casciano C, Tetzloff G, Long JF, Barnett A (1983) Studies on the mechanisms of the antisecretory and cytoprotective actions of SCH 28080. J PharmacolExpTher 226: 121-125.
- Keeling DJ, Laing SM, Senn-Bilfinger J (1988) SCH 28080 is a lumenally acting, K+-site inhibitor of the gastric (H+ + K+)-ATPase. BiochemPharmacol 37: 2231-2236.
- Wallmark B, Briving C, Fryklund J, Munson K, Jackson R, et al. (1987) Inhibition of gastric H+,K+-ATPase and acid secretion by SCH 28080, a substituted pyridyl(1,2a)imidazole. J BiolChem 262: 2077-2084.
- Kromer W, Positus S, Kruger U (2000) PharamceuticalsVol 2 Wiley- VCH, Weinhim.
- Labenz J1 (2000) Consequences of Helicobacter pylori cure in ulcer patients. Baillieres Best Pract Res ClinGastroenterol 14: 133-145.
- Laursen LS, Havelund T, Lauritsen K, Madsen JR (1989) [Prostaglandin analogues in the treatment of peptic ulcer disease]. UgeskrLaeger 151: 74-78.
- Jensen SL, Funch Jensen P (1992) Role of sucralfate in peptic disease. Dig Dis 10: 153-161.
- Gorbach SL (1990) Bismuth therapy in gastrointestinal diseases. Gastroenterology 99: 863-875.
- Tandon R, Khanna HD, Dorababu M, Goel RK (2004) Oxidative stress and antioxidants status in peptic ulcer and gastric carcinoma. Indian J PhysiolPharmacol 48: 115-118.
- Gutteridge JM (1995) Lipid peroxidation and antioxidants as biomarkers of tissue damage. ClinChem 41: 1819-1828.
- Chaturvedi A, Kumar MM, Bhawani G, Chaturvedi H, Kumar M, et al. (2007) Effect of ethanolic extract of Eugenia jambolana seeds on gastric ulceration and secretion in rats. Indian J PhysiolPharmacol 51: 131-140.
- al-Sereiti MR, Abu-Amer KM, Sen P (1999) Pharmacology of rosemary (Rosmarinusofficinalis Linn.) and its therapeutic potentials. Indian J ExpBiol 37: 124-130.
- Dehpour AR, Zolfaghari ME, Samadian T, Vahedi Y(1994) The protective effect of liquorice components and their derivatives against gastric ulcer induced by aspirin in rats. J Pharm Pharmacol 46: 148-149.
- Favier LS, María AO, Wendel GH, Borkowski EJ, Giordano OS, et al. (2005) Anti-ulcerogenic activity of xanthanolidesesquiterpenes from Xanthium cavanillesii in rats. J Ethnopharmacol 100: 260-267.
- Konturek SJ, Mrzozowski T, Drozdowicz D, Pawlik W, Sendur R (1987) Gastroprotective and ulcer healing effects of solon, a synthetic flavonoid derivative of sophoradin. Hepatogastroenterology 34: 164-170.
- Hiruma-Lima CA, Gracioso JS, Toma W, Almeida AB, Paula AC, et al. (2001) Gastroprotective effect of aparisthman, a diterpene isolated from Aparisthmiumcordatum, on experimental gastric ulcer models in rats and mice. Phytomedicine 8: 94-100.
- Tariq M, Al Moutaery AR (1997) Gastric anti-ulcer and cytoprotective effect of l-serine in rats. Res CommunMolPatholPharmacol 97: 171-184.
- Zhang Z, Zou YY, Li FJ, Hu CP (2011) Asymmetric dimethylarginine: a novel biomarker of gastric mucosal injury? World J Gastroenterol 17: 2178-2180.
- Alberghina M, Brogna A, Mangiameli A, Marletta F, Rizzarelli E, et al. (1982) Copper (II) complexes of aminoacids: gastric acid antisecretory activity in rats. FarmacoSci 37: 805-814.
- Brzozowska I, Konturek PC, Brzozowski T, Konturek SJ, Kwiecien S, et al. (2002) Role of prostaglandins, nitric oxide, sensory nerves and gastrin in acceleration of ulcer healing by melatonin and its precursor, L-tryptophan. J Pineal Res 32: 149-162.
- Ikeda M, Shiratori K, Shimizu K, Watanabe S, Hayashi N (1997) [The mechanisms of the inhibition of gastric acid secretion induced by intraduodenal amino acids in rats]. Nihon ShokakibyoGakkaiZasshi 94: 12-20.
- Blbller N, AkkuŸ MA, Ilhan YS, Baysal F, Ozercan I, et al. (2003) The effects of L-tryptophan and pentoxiphylline on stress ulcer. UlusTravmaAcilCerrahiDerg 9: 90-95.
- Yang EY, Nahrwold DL (1993) Tyrosine inhibits intestinal-phase gastric-acid secretion. Surgery 114: 915-920.
- Glavin GB (1989) Calcium channel modulators: effects on gastric function. Eur J Pharmacol 160: 323-330.
- McColl KE, Buchanan NM, Laferla G, Hearns J, Buchanan K, et al. (1987) Effects of nifedipine on gastric acid secretion and gastrin release in man. Gut 28: 455-459.
- Alican I, Toker F, Arbak S, Yegen BC, Yalçin AS, et al. (1994). Gastric lipid peroxidation, glutathione and calcium channel blockers in the stress-induced ulcer model in rats. Pharmacol Res 30: 123-35.
- Szelenyi I (1980) Calcium, histamine, and pentagastrin: speculations about the regulation of gastric acid secretion at cellular level. Agents Actions 10: 187-190.
- Sewing KF, Hannemann H (1983) Calcium channel antagonists verapamil and gallopamil are powerful inhibitors of acid secretion in isolated and enriched guinea pig parietal cells. Pharmacology 27: 9-14.
- Clive WO, Chi HC, Man CT, Marcel WLK (1985) The Influence of Verapamil on the Gastric Effects of Stress in Rats. European Journal of Pharmacology 112: 399-404.
- Wong WS, Rahwan RG (1990) Antiulcer activity of the calcium antagonist propyl-methylenedioxyindene--I. Effect on cold/restraint stress-induced ulcers in rats. Gen Pharmacol 21: 321-325.
- al-Mashhadani WM, Karim KH, al-Taie RI, al-Zahawi HM (1991) Nifedipine versus cimetidine in prevention of stress-induced gastric ulcers in rats. Eur J Pharmacol 192: 117-121.
- Subudhi BB, Sahoo SP (2013) Development of amino acid conjugated sulfonamides as potent antiulcer agent. Medicinal Chemistry Research.
- Subudhi BB, Panda SK, Ghosh G, Panda PK (2012) Synthesis and antiulcer activity study of disubstituted alkyl 4-(substituted)-2,6-dimethyl-1-((4-oxo-3-(4-sulfamoylphenyl)-2-thioxo-3,4-dihydroquinazolin-1(2H)-yl) methyl)-1,4-dihydropyridine-3,5 dicarboxylate. Ind J Chem (Sec B) 51: 899-903.
- Subudhi BB, Sahoo SP (2011) Synthesis and evaluation of antioxidant, anti-inflammatory and antiulcer activity of conjugates of amino acids with nifedipine. Chem Pharm Bull (Tokyo) 59: 1153-1156.
- Subudhi BB, Sahoo SP (2011) Synthesis and antiulcer activity evaluation of conjugates of amino acids with N-aroyl- N, N'-dicyclohexyl urea. Chem Cent J 5: 86.
- Subudhi BB, Panda PK, Bhatta D (2009) Synthesis and antiulcer activity study of 1, 4-dihydropyridines and their mannich bases with sulfanilamide. Ind J Chem (Sec B) 48: 725-728.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13701
- [From(publication date):
April-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 12567
- PDF downloads : 1134