Editorial Open Access
Unveiling the Undiscovered: Etiology of Acute Encephalitis Syndrome in North India
Amita Jain*, Parul Jain and Bhawana Jain
Department of Microbiology, King George’s Medical University, Lucknow, India
- *Corresponding Author:
- Amita Jain
Department of Microbiology
King George’s Medical University
Lucknow, UP, India, 226003
Tel: 091-9415023928
E-mail: amita602002@yahoo.com
Received date: March 27, 2015; Accepted date: April 28, 2015; Published date: April 30, 2015
Citation: Jain A, Jain P, Jain B (2015) Unveiling the Undiscovered: Etiology of Acute Encephalitis Syndrome in North India. J Neuroinfect Dis 6:e101. doi:10.4172/2314-7326.1000e101
Copyright: © 2015 Jain A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Acute Encephalitis Syndrome (AES) poses a great public health problem in India, occurring both in epidemics and sporadically. The magnitude of the problem has been estimated to be around 50,000 cases and 10,000 deaths annually. Traditionally Japanese encephalitis (JE) has been considered to be the most important cause of AES in our country. The overemphasis on JE is so much so that AES surveillance is paralleled to JE surveillance for all practical purposes. In 2014, the total numbers of AES cases and deaths reported from India were 10,853 and 1717 respectively and the corresponding values for JE were 1657 (~15%) and 293 (~17%) respectively. This implies that other undiscovered or neglected etiology of AES, which accounts for about 85%, also exists and should also be looked for.
Introduction
Acute Encephalitis Syndrome (AES) poses a great public health problem in India, occurring both in epidemics and sporadically. The magnitude of the problem has been estimated to be around 50,000 cases and 10,000 deaths annually [1]. Traditionally Japanese encephalitis (JE) has been considered to be the most important cause of AES in our country. The overemphasis on JE is so much so that AES surveillance is paralleled to JE surveillance for all practical purposes. In 2014, the total numbers of AES cases and deaths reported from India were 10,853 and 1717 respectively and the corresponding values for JE were 1657 (~15%) and 293 (~17%) respectively [2]. This implies that other undiscovered or neglected etiology of AES, which accounts for about 85%, also exists and should also be looked for.
AES in India, especially Northern India, as per definition of WHO [3] encompasses several other illnesses; it has malaria, enteric encephalopathy, tubercular meningitis, dengue with neurological manifestations, scrub typhus, bacterial meningitis, etc. It surely is a mixed pot.
Scientific literature discusses about several other infectious agents; only few of them are treatable. Bacterial meningoencephalitis, most commonly caused by Streptococcus pneumoniae, Neisseria meningitides, and Haemophilus influenzae type B, is amenable to specific antibiotic treatment and can be prevented by the available vaccines. Tuberculosis also requires specific treatment. Scrub typhus caused by Orientia tsutsugamushi causes encephalitis that is difficult to diagnose, but can be treated easily. Enteric encephalopathy is not rare and needs different management. Malaria is endemic and cerebral malaria is common. However, sufficient data is not available from India on these easily treatable causes of AES [4].
Today, world is more concerned about the untreatable and not known causes. When AES cases from Uttar Pradesh, India, were investigated for the etiological diagnosis, viral etiology could be determined for approximately 58% cases, which included Japanese encephalitis virus 16%, Dengue virus 11%, Herpes simplex virus, Mumps virus and measles virus 9% each, and Varicella Zoster virus 4%. Total 42% cases were AES cases with unknown etiology, which still need to be determined [5]. Dengue encephalitis and neurological manifestations are commonly seen [6]. Viruses that have been implicated in outbreaks of AES, but have not been studied countrywide include Chandipura virus, West Nile virus, Nipah virus, Kyasanur Forest Disease Virus, Enteroviruses and Adenoviruses [7]. Case reports are available on human Parvovirus B19V as a potential cause of encephalitis and encephalopathy in immunocompetent cases. Human Parvovirus 4 can be an emerging cause of encephalitis in patients with acute encephalitis syndrome. We detected human parvovirus 4, from CSF of two patients presenting as acute encephalitis syndrome in northern India, though causative association is yet to be proved [8]. Consideration should be given to detection of these non-JE AES etiologies, as it will directly impact the formulation of health policies of AES in India. This includes identifying targets for immunization, chart preventive strategies and implement appropriate control measures, especially in outbreak situations and formulating other public health interventions.
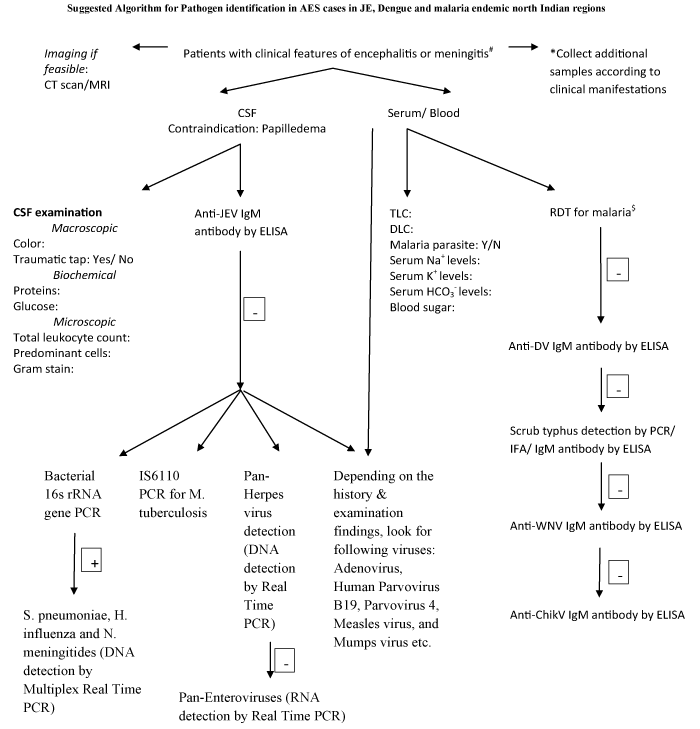
In a resource limited country like India, testing all the AES samples for all the possible pathogens is a remote possible. Moreover, the volume of cerebrospinal fluid available for laboratory testing is often small. Therefore, an algorithmic approach for the diagnosis of encephalitis is advocated which may serve many purposes, including patient management, research, and facilitating public health disease surveillance. An algorithm should be designed for each region, based on the local prevalence of the disease organisms and this will help to diagnose most cases of AES, using minimum resources within a reasonable period of time. An attempt was made to design an algorithm for Uttar Pradesh (Figure 1), a region endemic for both JEV and DV, which can be used as an example.
*eg lesion scraping if rash is present, saliva in presence of mandibular swelling/orchitis.
$Rapid Diagnostic Tests for malaria Note: Detailed clinical history to be collected as per preformed format
Figure 1: Case definition of AES as per WHO: A person of any age, at any time of year with the acute onset of fever and a change in mental status (including symptoms such as confusion, disorientation, comatose, or inability to talk) and/or new onset of seizures (excluding simple febrile seizures).
References
- Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, et al. (2011) Estimated global incidence of Japanese encephalitis: a systematic review. Bull World Health Organ 89: 766-774, 774A-774E.
- Sharma SN, Shukla RP, Raghavendra K, Subbarao SK (2005) Impact of DDT spraying on malaria transmission in Bareilly District, Uttar Pradesh, India. J Vector Borne Dis 42: 54-60.
- Japanese encephalitis surveillance standards. From WHO-recommended standards for surveillance of selected vaccine-preventable diseases.
- Ravi V, Mani R, Govekar S, Desai A, Lakshman L, et al. (2014) Aetiology and Laboratory Diagnosis of Acute Encephalitis Syndrome with Special Reference to India. J Commun Dis 46: 12- 23.
- Jain P, Jain A, Kumar A, Prakash S, Khan DN, et al. (2014) Epidemiology and etiology of acute encephalitis syndrome in North India. Jpn J Infect Dis 67:197-203.
- Murthy JM (2010) Neurological complication of dengue infection. Neurol India 58: 581-584.
- Joshi R, Kalantri SP, Reingold A, Colford JM Jr (2012) Changing landscape of acute encephalitis syndrome in India: a systematic review. Natl Med J India 25: 212-220.
- Prakash S, Jain A, Seth A, Singh AK, Jain B (2015) Complete genome sequences of two isolates of human parvovirus 4 from patients with acute encephalitis syndrome. Genome Announc 3.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 15394
- [From(publication date):
May-2015 - Nov 25, 2024] - Breakdown by view type
- HTML page views : 10913
- PDF downloads : 4481