Unvaccinated Convalescent Person with Previous Covid-19 Infection had Low Immunity Response: An Important Clinical Information
Received: 13-Jan-2022 / Manuscript No. JIDT-22-51617 / Editor assigned: 17-Jan-2022 / PreQC No. JIDT-22-51617 (PQ) / Reviewed: 27-Jan-2022 / QC No. JIDT-22-51617 / Revised: 31-Jan-2022 / Manuscript No. JIDT-22-51617 (A) / Published Date: 07-Feb-2022 DOI: 10.4172/2332-0877.1000490
Abstract
When the worldwide population enters the period of vaccination against SARS-CoV-2 infection, the more information on immune response, the better for the prevention strategy against COVID-19. We reported herein the results of SARS-CoV-2 antibodies in a cross-sectional study 75 Vietnamese participants divided into 3 groups: Auninfected person with 2 doses vaccination (“Vac” group; n=32); B: convalescent person who received first dose vaccine then having COVID-19 infection (“Vac-F0” group; n=12); and C: unvaccinated convalescent person with previous COVID-19 infection (“F0” group; n=31). The “F0” group had 26% (8/31) with antibodies higher than 250 U/mL, significantly lower than those from “Vac” group (84.4%, 27/32) and “Vac-F0” group (83.3%, 10/12), p=0.000. There were 3 cases in “F0” group with “no immune response” (<0.4 U/mL, 9.7%). No difference in antibodies between “Vac” and “Vac-F0” group. Among “F0” group, “non-severe infection” person had immune response lower than that from whom with severe infection (p=0.04). Unvaccinated convalescent person with previous infection had low immunity against SARS-CoV-2 virus. The antibody measurement is essential to identify this at-risk population and an additional dose of vaccine is needed for them.
Keywords: COVID-19; Unvaccinated covalescent person; Anti -SARSCoV-2;Spike antibody
Introduction
The SARS-CoFV-2 virus belongs to the sarbecovirus group of coronaviruses, using spike proteins to bind to ACE2 receptors in the membranes of host cells and enter them [1]. A survey in Texas in Sep 2021 on 8,846 individuals found 1420 cases with low immunity response in person with infected COVID-19 history (16%) [2]. Low antibody titers recorded in individuals with asymptomatic or mild disease [3]. The COVID-19 pandemic in Vietnam is part of the ongoing worldwide pandemic. Starting in April 2021, Vietnam experienced its largest outbreak to date, with over 83,000 infections. Vaccinations commenced on 8th March 2021 with a total of 51,968,108 administered vaccination doses reported by 8th October 2021 [4]. The immune response to COVID-19 has not been well confirmed up to the present time. The aim of our research was to contribute some information from data of Vietnamese person.
Tam Tri Saigon Hospital is a private hospital in district 12, Ho Chi Minh City, Viet Nam. The Hospital received patients for treatment during the endemic crisis in Ho Chi Minh, from June to October 2021. The incidence rates per day of positive COVID-19 cases were high in Jul -Aug, as 5.56%-16.28% then reduced to 1%-2% in early October.
There were 75 Vietnamese individuals participated into the study, divided into three groups: A-healthy person with full 2 doses of vaccine (“Vac” group), n=32; B-convalescent persons from previous COVID-19 infection having a first vaccine dose (“Vac-F0” group), n=12; and C- unvaccinated convalescent person from previous COVID-19 infection (“F0” group), n=31 [5]. Clinical characteristics of participants were presented (Table 1). The severity of infection was not different between “Vac-F0” and “F0” groups.
| Variables | Participant groups | p value | |||||
|---|---|---|---|---|---|---|---|
| Vac (n=32) | Vac-F0 (n=12) | F0 (n=31) | |||||
| Gender | Male | 17 | 7 | 15 | 0.6* | ||
| Female | 15 | 5 | 16 | ||||
| Age (yrs.) | Mean ± SD | 44.1 ± 2.17 | 33.18 ± 1.19 | 31.3 ± 2.24 | 0.001** | ||
| Min-max | 22-67 | 22-46 | 5-54 | ||||
| Time from date received the second dose of vaccine (days) | Mean ± SD | 52.9 ± 4.01 | |||||
| Min - max | 15-110 | ||||||
| Time from recovery date of previous SARS-CoV-2 infection (days) | Mean ± SD | 29 ± 4.5 | 47.74 ± 2.4 | ||||
| Min-max | 8-54 | 0-80 | |||||
| Severity of previous SARS-CoV-2 infection | Severe (n) | 5 | 9 | 0.32* | |||
| Non-severe (n) | 7 | 22 | |||||
*:Chi-square test; **:KrusKal-Wallis test
Table 1: Clinical characteristics of groups of participants.
There was a significant difference in anti-SARS-CoV-2 spike antibodies between 3 groups (p=0.000). The paired comparison showed the strong difference between “F0” group versus other 2 groups, “Vac” and “Vac-F0”, no difference between “Vac” and “Vac- F0” group. There were 3 cases in “F0” group with antibodies <0.4 U/mL (9.7%). In “F0” group, 5 out of 8 (63%) with severe COVID-19 infection had high antibodies >250 U/mL, different from 3 out of 22 non-severe cases (13%), p=0.04 (Table 2).
| Groups | Anti-SARS-CoV-2 Spike Antibodies (U/mL) | Total | Comparison (Pearson Chi-Square statistics) | |||||
|---|---|---|---|---|---|---|---|---|
| >250 | 0.8–250 | <0.8 | Between 3 groups | “Vac” versus “F0” | “Vac-F0” versus “F0” | “Vac” versus “Vac-F0” | ||
| “Vac” (n) | 27 | 5 | 0 | 32 | 0.000* | 0.000* | 0.001* | 0.87 |
| “Vac-F0” (n) | 10 | 2 | 0 | 12 | ||||
| “F0” (n) | 8 | 20 | 3 (<0.4 U/mL) | 31 | ||||
*:Significantly different
Table 2: The concentration of Anti-SARS-CoV-2 Spike antibodies (U/ml) of 3 participant groups and the comparison between each paired group.
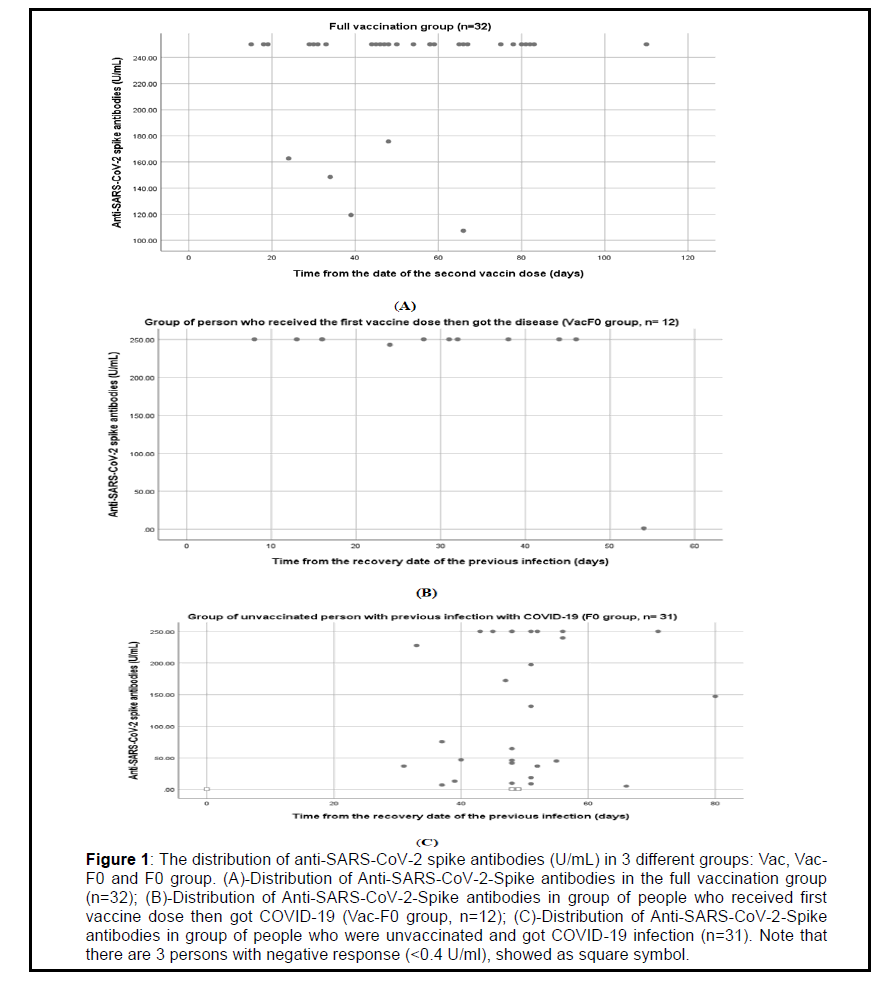
The distribution of anti-SARS-CoV 2 spike antibodies (U/mL) of the 3 groups showed (Figure 1). Among “Vac” group, 27(84.4%) are with antibodies higher than 250 U/mL. Among “Vac-F0” group, 10(83.3%) are with antibodies higher than 250 U/mL, 2 cases with 242.8 and 1.34 U/mL. Among “F0” group, only 8 cases are with antibodies higher than 250 U/ml (26%), especially 3 cases with negative response (<0.4 U/mL) (9.7%).
Figure 1: The distribution of anti-SARS-CoV-2 spike antibodies (U/mL) in 3 different groups: Vac, Vac- F0 and F0 group. (A)-Distribution of Anti-SARS-CoV-2-Spike antibodies in the full vaccination group (n=32); (B)-Distribution of Anti-SARS-CoV-2-Spike antibodies in group of people who received first vaccine dose then got COVID-19 (Vac-F0 group, n=12); (C)-Distribution of Anti-SARS-CoV-2-Spike antibodies in group of people who were unvaccinated and got COVID-19 infection (n=31). Note that there are 3 persons with negative response (<0.4 U/ml), showed as square symbol.
The first important result of our study was the low immunity response in unvaccinated persons with SARS-CoV-2 infection compared to those having full vaccination or partial vaccination (reveived first dose of vaccine). A survey in Texas in Sep 2021 on 8,846 individuals found 1420 with infected history having low immunity response (16%) [2]. Low anti-SARS-CoV-2 IgG in unvaccinated convalescent person with asymptomatic or symptomatic previous COVID-19 infection compared to convalescent person having first vaccine dose and to uninfected person with full vaccination [6]. The finding in our study revealed that natural infection does not elicit the full immune response and just be equal to that from first dose of vaccination. The unvaccinated convalescent persons should be taken care more than believed that they are being full protection after getting out from disease. The strategy on permitting or using all these persons to go to anywhere or to work at any places may be needed to review.
The second finding in our study was the combination of first dose vaccine and SARS-CoV-2 infection, “Vac-F0”, eliciting a good immunity response, equivalent or higher than that seen in full vaccination group. The antibody after SARS-CoV-2 vaccination was extremely vivacious in subjects with previous infection [6-8]. The report in Singapore announced decades-old SARS infection triggers potent response to COVIC-19 vaccines [9]. After one dose of mRNA vaccine, individuals previously with COVID-19 infection had high anti-RBD IgG [10]. It means that combination of one dose of vaccination with a natural infection, regardless infection occurring before or after vaccination, all elicit the good synergistic immune response. This should be considered as a hybrid combination of action. Higher levels of neutralizing antibodies in previously infected participants compared to those from normal participants [11]. Because of the natural immunity is incompleted, patients with ESKD should be prioritized for SARS-CoV-2 vaccination, independent of their COVID-19 disease history [12].
The last point in our study was the relationship between low immunity response and non-severe COVID-19 infection [6]. The measurement of SARS-CoV-2 antibodies is essential to detect previous infections in people who were asymptomatic or had mild Covid-19 disease, according to FDA recommendation [13]. Therefore, the measurement of antibodies in a wide range of different kind of people is necessary to have good data for a sustainable prevention strategy against COVID-19 infection.
Conclusion
For conclusion, the study revealed that the unvaccinated convalescent person had low immunity response compared to the normal person with 2 vaccine doses, as well as to convalescent person with 1 vaccine dose, thus these unvaccinated convalescent persons need to have the close follow-up and to have as soon as possible at least one dose of vaccine right way.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Author Contributions
Le Ngoc Hung is the person who takes responsibility for the intergrity of the wok as a whole, from inception to published article; study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript. Nguyen Huu Tung, Cao Hung Phu, Nguyen Van Bac, and Nguyen Manh Hoa contributed to critical revision of the manuscript for important intellectual content.
Acknowledgements
We would like to thank the support of the Director Board of Tam Tri Hospital as well as the staff of Laboratory Department for the study.
References
- Kuba K, Imai Y, Penninger JM (2006) Angiotensin-converting enzyme 2 in lung diseases. Curr Opin Pharmacol 6:271-276.
[CrossRef] [Google Scholar] [PubMed]
- Impact of prior SARS-CoV-2 infection and vaccine on antibody levels: Texas survey, News Medical Life Sciences, 2021.
- Immune responses and immunity to SARS-CoV-2, European Centre for Disease Prevention and Control, 2021.
- COVID-19 pandemic in Vietnam, Wikipedia, 2021.
- Hardy A, Shum M, Quyên VN. The ‘F-system’ of targeted isolation: A key method in Vietnam’s suppression of covid-19, HAL Open Science, 2020.
- Tretyn A, Szczepanek J, Skorupa M, Jarkiewicz-Tretyn J, Sandomierz D, et al. (2021) Differences in the concentration of anti-SARS-CoV-2 IgG antibodies post-covid-19 recovery or post-vaccination. Cells 10:1952.
[CrossRef] [Google Scholar] [PubMed]
- Callegaro A, Borleri D, Farina C, Napolitano G, Valenti D, et al. (2021) Antibody response to SARS-CoV-2 vaccination is extremely vivacious in subjects with previous SARS-CoV-2 infection. J Med Virol 93:4612-4615.
[CrossRef] [Google Scholar] [PubMed]
- Steensels D, Pierlet N, Penders J, Mesotten D, Heylen L (2021) Comparison of SARS-CoV-2 antibody response following vaccination with BNT162b2 and mRNA-1273. JAMA 326:1533-1535.
[CrossRef] [Google Scholar] [PubMed]
- Mallapaty S (2021) Decades-old SARS virus infection triggers potent response to COVID vaccines. Nature 596:471-472.
[CrossRef] [Google Scholar] [PubMed]
- Demonbreun AR, Sancilio A, Velez MP, Ryan DT, Saber R, et al. (2021) Comparison of IgG and neutralizing antibody responses after one or two doses of COVID-19 mRNA vaccine in previously infected and uninfected individuals. EClinicalMedicine 38:101018.
[CrossRef] [Google Scholar] [PubMed]
- Anichini G, Terrosi C, Gandolfo C, Savellini GG, Fabrizi S, et al. (2021) SARS-CoV-2 antibody response in persons with past natural infection. N Engl J Med 385:90-92.
[CrossRef] [Google Scholar] [PubMed]
- Cohen DE, Sibbel S, Marlowe G, Bludorn K, Miller D, et al. (2021) Antibody status, disease history, and incidence of SARS-CoV-2 infection among patients on chronic dialysis. J Am Soc Nephrol 32:1880-1886.
[CrossRef] [Google Scholar] [PubMed]
- FDA in brief: FDA advises against use of SARS-CoV-2 antibody test results to evaluate immunity or protection from COVID-19, including after vaccination, US Food & Drug Administration, 2021.
Citation: Hung LN, Tung NH, Phu CH, Bac NV, Hoa NM (2022) Unvaccinated Convalescent Person with Previous Covid-19 Infection had Low Immunity Response: An Important Clinical Information. J Infect Dis Ther 10:490. DOI: 10.4172/2332-0877.1000490
Copyright: © 2022 Hung LN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2288
- [From(publication date): 0-2022 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 1761
- PDF downloads: 527