Unusual Series of Streptococcus milleri Group Infections
Received: 24-Jan-2018 / Accepted Date: 14-Feb-2018 / Published Date: 16-Feb-2018 DOI: 10.4172/2476-213X.1000123
Abstract
Background: Streptococcus milleri group (SMG) are a potential cause for variable pyogenic infections. Few studies described the epidemiology and clinical presentation of these infections.
Methods/results: We describe five cases of streptococcus milleri infections in a single internal medicine ward, which represents higher incidence than expected. All patients survived while one infected with S. Intemedius, needed intensive care hospitalization and prolonged mechanical ventilation.
Conclusion: As the clinical presentation of patients with SMG infections may vary, and some may even present afebrile and with normal inflammatory markers, a careful clinical estimation and accurate diagnosis is required. When SMG infection is diagnosed, early drainage of the pyogenic foci and empiric antimicrobial treatment is indicated.
Keywords: Case series; Streptococcus milleri; pyogenic infections; thoracic
Introduction
Streptococcus Milleri Group (SMG) is a subgroup of the Streptococcus Viridans and consists of three sub-species (anginosus, intermedius and constellatus). SMG is part of the normal flora of human mucous membranes [1], but may cause pyogenic infections. The incidence of these infections is not clear, one series found the incidence of clinically significant SMG infection in tertiary hospital to be 8.8 cases per 10,000 admissions [2]. In this paper we present five cases of SMG infection in a single internal medicine ward in Rambam Health care Campus (Haifa, Israel) during six months period in 2015, which reflects an incidence of 29 cases per 10,000 admissions. These cases demonstrate the variable clinical presentation of SMG infections.
Cases Presentation
Patient 1
A 56 years old man was admitted due to fever, confusion and general deterioration. His past medical history included schizophrenia, ischemic heart disease, hypertension and hyperlipidemia. He had also suffered a cerebro vascular accident and a traumatic subarachnoid hemorrhage in the past. A week prior to his admission he was discharged from a peripheral hospital where he was treated due to seizures, probably related to sub-therapeutic level of valproic acid. During his admission there, he developed fever and streptococcal bacteremia, underwent total body Computed Tomography (CT) and trans esophagial echo that did not reveal any bacterial focus and was treated with a course of intravenous wide-spectrum antibiotics. On admission he was afebrile but slightly confused. His vital signs, physical examination and initial laboratory evaluation were non remarkable. Chest X-ray revealed a shadowing in the left lower lobe. He was admitted and treated under the working diagnosis of hospital acquired pneumonia. In the first days of his admission he had recurrent fever peaks. His blood cultures were sterile. Due to an impression of acute confusion he underwent a brain CT scan (w/o contrast) that did not reveal gross pathology.
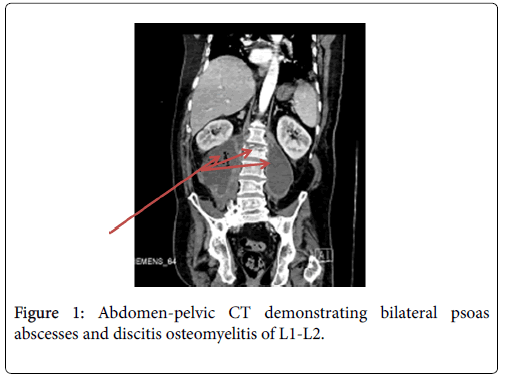
Due to recurrent febrile episodes in spite of wide spectrum antimicrobial treatment, and as a formal blood culture result (from his previous admission) of S. Anginosus was received he underwent a repeated total body CT with contrast. The scan revealed massive bilateral psoas abscesses (10 cm × 10 cm × 22 cm on the right and 6 cm × 6 cm × 15 cm left), discitis osteomyelitis of L1-L2 (Figure 1) and an intracranial lesion suspected for brain empyema. The patient underwent US guided drainage of the psoas abscesses. He was presented to the neurosurgeons who were not convinced that the intracranial lesion was an empyema; therefore no neurosurgical intervention was performed.
The pus cultures were sterile as well as the repeated blood cultures and he was treated with IV penicillin according to the susceptibility of the S. Anginosus previous positive culture. He underwent serial scans both for the intracranial lesion and for the psoas abscesses with resolution of the findings. During the course of treatment he was afebrile and clinically improved. After a total of 12 weeks of treatment and a full draining of the abscesses, he was discharge for rehabilitation.
Patients 2
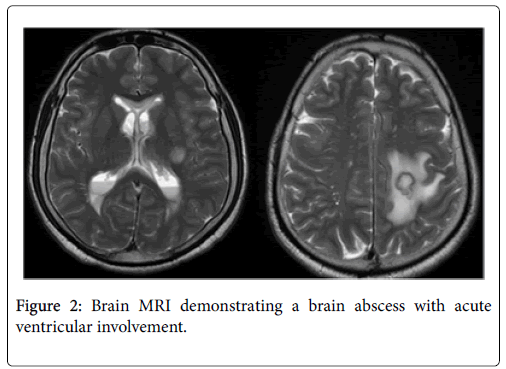
A 45 years old man, with history of intravenous drug abuse, was admitted due to three episodes of seizures and right hemiparesis in the week prior to his admission. In Emergency room he underwent a brain CT which demonstrated a rounded, 1.5 cm diameter lesion suspected for brain malignancy. He was admitted for further investigation. On admission he was started on steroids and anti-epileptics. He underwent a chest-abdomen-pelvic CT which showed no other suspected malignancy. During the first days of his hospitalization he deteriorated, complaining on worsening headache, fever, nausea and vomiting. Serial brain CT revealed no new acute finding. He was planned for lumbar puncture. Prior to the lumbar puncture he underwent a brain MRI which demonstrated a brain abscess with acute ventricular involvement (Figure 2). He was urged to operating room and underwent external ventricular drainage of large amount of pus in high pressure. The pus cultures grew a poly-microbial growth including S. Intermedius . Following surgery, he was treated with a long course of intravenous antibiotic. Due to the need for long term mechanical ventilation he later underwent tracheostomy and was treated at the neurosurgical intensive care unit. As his clinical condition improved he was discharge for respiratory rehabilitation with recommendation to complete 8 weeks of intravenous antibiotics.
Patients 3
A 69 years old man who was under investigation for a portal vein thrombosis and a space occupying lesion of the pancreas, was admitted due to abdominal discomfort. On admission, his vital signs, physical examination and laboratory evaluation were normal. He underwent abdominal ultrasound scan which did not reveal clear etiology for his symptoms. Later he underwent an abdominal CT which demonstrated two liver lesions suspected for metastasis. Due to this finding he was transferred to a surgical ward for further investigation. On the day of his transfer, due to a peak of fever blood cultures were obtained.
During his hospitalization in the surgical ward he underwent a biopsy from the pancreatic lesion which was non-diagnostic. An alpha hemolytic strep was detected in the blood cultures that were taken prior to his transfer during the fever peak. As he had no recurrent episodes of fever it was suspected to be a contamination. He was discharged with an appointment for an elective biopsy from the liver lesions. Two days following his discharge he was re-admitted due to fever and acute confusion. He was treated with broad spectrum antibiotics and underwent a fine needle biopsy of the liver lesion with pus aspirated from the lesion. The pus cultures demonstrated alphahemolytic S. Anginosus . Following a further short course of antibiotics he was discharge for outpatient follow-up.
Patient 4
A 77 years old man, with a history of non-small-cell-carcinoma of lungs, previously underwent radiotherapy and chemotherapy, was admitted due to fever, right upper quadrant abdominal pain and jaundice. On arrival he was hemo-dynamically stable and had increased inflammatory markers. An ultrasound-scan of his abdomen demonstrated a wide common bile duct, and he underwent urgent endoscopic retrograde cholangiopancreatography (ERCP) with pus and multiple bile stones drained. Later his blood culture grew polymicrobial growth including S. Anginosus . He was treated with a course of intravenous antibiotics with good clinical response and was later discharged.
Patient 5
A 79 years old man, with progressive dementia and known ischemic heart disease was admitted due to fever and dyspnea. On admission he was febrile, physical examination revealed bilateral reduced air entry in lungs with moist crackles over the lung bases. His white blood cell count was raised and chest X-ray demonstrated bilateral pleural effusions and a left lower lobe shadowing suspected for consolidation. Blood cultures were taken and empiric antibiotic was started. As only mild clinical improvement was achieved with the treatment, and as S. Constelatus grew in the blood cultures empyema was suspected. He underwent a chest Ultrasound-Scan, followed by chest CT in order to estimate the amount of effusion. As only small amount of fluid was demonstrated, he was presented to the thoracic surgeons who reviewed the scans and were impressed it was unlikely to be an empyema. Due to his progressive dementia, his lack of cooperation, the risk of complication and as he slowly clinically improved, it was decided not to preform further invasive investigations at that point. After a course of intravenous antibiotics he was discharged for outpatient repeated chest X-ray and follow-up.
Conclusions
SMG infections are related to various clinical manifestations. Our series, as the previously published data [2,3], present a wide clinical spectrum, male predominance and high rates of significant comorbidities among patients with SMG infection. All the five cases we presented survived, in concordance with the known overall excellent prognosis of SMG infection. The clinical relevance of the SMG subspecies is yet to be determined [4] but S. intermedius is generally related to worse prognosis and longer hospital stay [5]. The one case we presented here with S. intermedius infection did have the most complicated course of hospitalization, and required intensive care hospitalization.
The clinical presentation of patients with SMG infections may vary, and as reported herein, some may even present afebrile with normal inflammatory markers. Therefore, a careful clinical evaluation and accurate diagnosis is required. Blood cultures should be taken from any patient with suspected infectious disease prior to administration of antibiotics; when SMG infection is diagnosed, one must look for a focus of the infection. Drainage of the pyogenic foci and empiric antimicrobial treatment is indicated.
References
- Gossling J (1988) Occurrence and pathogenicity of the Streptococcus milleri group. Rev Infect Dis 10: 257-285.
- Siegman-Igra Y, Azmon Y, Schwartz D (2012) Milleri group streptococcus-a stepchild in the viridans family. Eur J Clin Microbiol Infect Dis 31: 2453-2459.
- Laupland KB, Ross T, Church DL, Gregson DB (2006) Population-based surveillance of invasive pyogenic streptococcal infection in a large Canadian region. Clin Microbiol Infect 12: 224-230.
- Claridge JE 3rd, Attorri S, Musher DM, Hebert J, Dunbar S (2001) Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus ("Streptococcus milleri group") are of different clinical importance and are not equally associated with abscess. Clin Infect Dis 32: 1511-1515.
- Junckerstorff RK, Robinson JO, Murray RJ (2014) Invasive Streptococcus anginosus group infection-does the species predict the outcome? Int infect Dis 18: 38-40.
Citation: Kobo O, Vainer-Evgrafov E, Frisch A, Karban A, Tzoran I (2018) Unusual Series of Streptococcus milleri Group Infections. J Clin Infect Dis Pract 3:123. DOI: 10.4172/2476-213X.1000123
Copyright: © 2018 Kobo O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 6113
- [From(publication date): 0-2018 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 5283
- PDF downloads: 830