Case Report Open Access
Unusual Pyogenic Meningitis Masquerading as Leukodystrophy
Rajul Rastogi1*, Prabhat Kumar Bhagat1, Anshuman Srivastava2, Yuktika Gupta1, Pawan Joon1, Asif Majid Wani1 and Vijai Pratap1
1Teerthanker Mahaveer Medical College and Research Center, Moradabad, UP, India
2School of Medical Science and Research, Sharda University, Greater Noida, UP, India
- *Corresponding Author:
- Rajul Rastogi
Teerthanker Mahaveer Medical College and Research Center
Moradabad, UP, India
E-mail: eesharastogi@gmail.com
Received date: August 02, 2016; Accepted date: August 31, 2016; Published date: September 02, 2016
Citation: Rastogi R, Bhagat PK, Srivastava A, Gupta Y, Joon P, Wani AM, et al. (2016) Unusual Pyogenic Meningitis Masquerading as Leukodystrophy. J Neuroinfect Dis 7:225. doi: 10.4172/2314-7326.1000225
Copyright: ©2016 Rastogi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Meningitis is a frequent cause of morbidity and mortality in pediatric age-group with pyogenic cases outnumbering other etiologies especially in the Indian subcontinent. Though the diagnosis of meningitis is usually made on clinical and CSF examination yet imaging is often required to rule out focal lesions, hydrocephalus and other complications or when clinical examination is equivocal. Rarely, initial imaging may be normal or may suggest another diagnosis leading to clinicoradiological discordance making further detailed evaluation imperative. Hence, in this article, we present a rare case of pyogenic meningitis that mimicked leukodystrophy on initial imaging with unusual presentation on detailed imaging.
Keywords
Meningitis; Pyogenic; Leukodystrophy; Imaging
Introduction
Meningitis is a frequent neurological cause of morbidity and mortality worldwide including Indian subcontinent [1]. Among the various etiologies, pyogenic type is the most predominant. Despite clinical diagnosis, imaging is often required to rule out coexisting focal lesions; detection and extent of other complications or when clinical diagnosis is in doubt [1]. In majority of cases, plain or non-contrast computed tomography (NCCT) or contrast-enhanced computed tomography (CECT) brain is the initial and only imaging studies required with latter involving intravenous contrast injection allowing detection of areas with breach in blood brain barrier. However, in difficult cases magnetic resonance imaging (MRI) brain or contrastenhanced MRI (CEMRI) is preferred as a problem solving tool with latter involving intravenous contrast injection and delineates area of breach in blood brain barrier. This article describes unusual form of pyogenic meningitis associated with septic vasculitis and infarcts where NCCT brain mimicked leukodystrophy and contrast-enhanced MRI (CEMRI) revealed signs of unusual meningitis. In usual form, there may be leptomeningeal enhancement or basilar exudate enhancement but in unusual form which is more severe, meningitis leads to septic vasculitis leading to necrosis of vessel wall and luminal thrombus formation and subsequent infarction.
Case Report
A five-year old female child presented with history of high-grade fever accompanied with chills and rigors for 4-5 days. Altered sensorium along with inconsolable cry and excessive lower limb movement were present since 2-3 days. Clinical examination revealed extensor plantar reflex and exaggerated knee reflex without obvious signs of neck rigidity. No evidence of any obvious papilledema was noted. Laboratory examination revealed raised blood total leukocyte count (12100 cells/ml) associated with raised neutrophil count; raised protein level; decreased glucose level; normal ADA values and positive culture for streptococcus pyogenes in cerebrospinal fluid (CSF). Chest radiograph and abdominal ultrasonography of the patient was unremarkable. Patient was then advised NCCT brain.
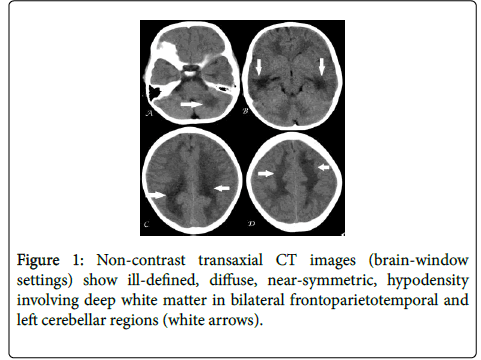
NCCT brain revealed ill-defined, near-symmetric, diffuse, hypodensity predominantly involving deep white matter of bilateral frontoparietotemporal and left cerebellar regions with slight extension in to cerebral subcortical white matter but without significant mass effect/midline shift or obvious focal lesion (Figure 1). Possibility of white matter disease probably leukodystrophy was suggested and CEMRI brain was then advised for further evaluation.
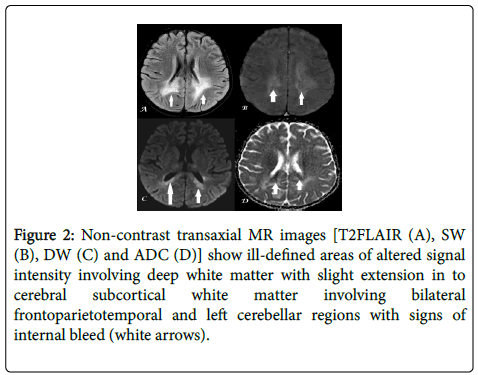
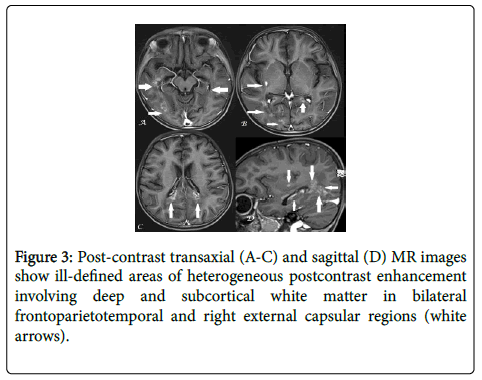
Non-contrast MRI brain revealed ill-defined, near-symmetric areas of altered signal intensity involving deep periventricular white matter of bilateral frontoparieto-temporal and bilateral cerebellar regions with variable extension in to cerebral subcortical white matter. The areas were variably hyperintense on T2-weighted (T2W) and T2-weighted fluid attenuated inversion recovery (T2FLAIR) images showing patchy internal areas of hyperintensity on diffusion-weighted (DW) images with corresponding hypointensity on apparent diffusion coefficient (ADC) images and subtle hypointensity on SW images (Figure 2). Post-contrast MRI revealed heterogeneous, coalescent, rim-enhancement in the above-described areas with a small enhancing focus in right external capsular region (Figure 3). No evidence of any obvious abnormal meningeal enhancement/meningeal thickening; basilar exudates or hydrocephalus was noted. Based on the radiological findings, the diagnosis of septic-vasculitis induced infarcts was made.
Figure 2: Non-contrast transaxial MR images [T2FLAIR (A), SW (B), DW (C) and ADC (D)] show ill-defined areas of altered signal intensity involving deep white matter with slight extension in to cerebral subcortical white matter involving bilateral frontoparietotemporal and left cerebellar regions with signs of internal bleed (white arrows).
Based on the clinicoradiological findings, intensive intravenous antibiotic therapy with 100 mg/kg body wt/day of ceftriaxone was initiated for 14 days and a good clinical response was achieved. The patient was then discharged on oral antibiotics (cefixime 8 mg/kg body wt) for 07 days and was found to be clinically normal on 4 and 8 weeks follow-up.
Discussion
Pyogenic meningitis is one of the severe causes of neurological impairment during infancy and childhood. The diagnosis is mainly based on clinical findings and CSF analysis. However, imaging is indicated for evaluation of severe complications including hydrocephalus; cerebritis or abscess formation; cranial nerve inflammation/palsy; arterial or venous thrombosis/vasculitis causing infarcts; ventriculitis/ependymitis and subdural collections requiring urgent attention and treatment [1]. Imaging is also indicated when the clinical diagnosis and CSF findings are equivocal. Septic vasculitis which leads to small cortical gray and deep white matter infarcts may lead to permanent tissue damage resulting in increased morbidity and mortality making early diagnosis and treatment imperative [2].
CEMRI brain is superior to CECT brain in detecting and monitoring complications of pyogenic meningitis [1]. Diffusionweighted images (DWI) along with magnetic resonance spectroscopy (MRS) are especially helpful in differentiating pyogenic abscess from other etiologies [1]. DWI images are very useful in detecting and monitoring infarcts secondary to septic vasculitis which are difficult to detect on CECT images as subtle hypodensity secondary to acute ischemia is difficult to detect in normal-appearing hypodense white matter [2]. When these septic-vasculitis induced infarcts show diffuse and near-symmetric involvement of white matter, they mimic leukodystrophy as seen in our case creating a diagnostic dilemma.
Septic-vasculitis and induced-infarcts usually show rim or heterogeneous enhancement secondary to vessel wall and adjacent meningeal enhancement but their recognition is equally important in the unusual cases of only white matter involvement with lack of meningeal enhancement as seen in our case [3,4]. When septic vasculitis involves the ventricular lining, it may lead to ventriculitis/ ependymitis with presence of fluid-fluid level in ventricular lumen being a specific sign [5].
Though contrast enhancement is useful in establishing infectious etiology yet it is not useful in determining the duration of treatment as persistent or even increased contrast enhancement of meninges, subdural spaces and basal cisterns may be seen during recovery phase [6].
Conclusion
Septic-vasculitis induced cerebral infarcts are a significant cause of morbidity and mortality in cases of pyogenic meningitis with CECT brain being initial while CEMRI being gold-standard imaging investigation. CT brain findings may rarely mimic leukodystrophy in cases of diffuse, near-symmetric, cerebral and cerebellar white matter infarcts. CEMRI should be considered as first imaging investigation whenever, clinical and CSF findings are discordant.
References
- Hughes DC, Raghavan A, Mordekar SR, Griffiths PD, Connolly DJ (2010) Role of imaging in the diagnosis of acute bacterial meningitis and its complications. Postgrad Med J 86: 478-85.
- Jan W, Zimmerman RA, Bilaniuk LT, Hunter JV, Simon EM, et al. (2003) Diffusion-weighted imaging in acute bacterial meningitis in infancy. Neuroradiology 45: 634-639.
- Küker W (2007) Cerebral vasculitis: imaging signs revisited. Neuroradiology 49: 471-479.
- Berlit P (2010) Diagnosis and treatment of cerebral vasculitis. Ther Adv NeurolDisord 3: 29-42.
- Fukui MB, William RL, Mudigonda S (2001) CT and MR Imaging Features of Pyogenic Ventriculitis. AJNR 22: 1510-1516.
- Harada S, Tsuji M, Yoshida T (2012)Contrast-enhanced MR imaging in bacterial meningitis in children-temporal profile and correlation with the prognosis. No To Hattatsu44: 315-319.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 12147
- [From(publication date):
September-2016 - Apr 27, 2025] - Breakdown by view type
- HTML page views : 11221
- PDF downloads : 926