Unsafe Phyllodes Tumor of the Breast and Pregnancy
Received: 01-Aug-2022 / Manuscript No. bccr-22-72152 / Editor assigned: 03-Aug-2022 / PreQC No. bccr-22-72152 / Reviewed: 17-Aug-2022 / QC No. bccr-22-72152 / Revised: 22-Aug-2022 / Manuscript No. bccr-22-72152 / Accepted Date: 27-Aug-2022 / Published Date: 29-Aug-2022 DOI: 10.4172/2572-4118.1000169
Abstract
Phyllodes Tumor (PT) is an intriguing fibroepithelial bosom growth that can act in an unexpected way contingent upon its biologic highlights. Customarily, PTs are characterized by their histologic highlights into harmless, fringe, and dangerous. As a rule that were accounted for, all PTs might repeat, yet entirely as it were the fringe and dangerous PT can metastasize. PT typically happens as a bosom protuberance or incidental tracking down on ultrasound (US) assessment. The clinical highlights incorporate a clear cut bosom mass, customary or lobulated. The analysis depends on the mix of morphology highlights; however remains testing, especially in the qualification from fibroadenomas. We report an instance of a 36-year-old patient who introduced for a voluminous bosom mass, quickly filling in the beyond 3-4 months. At show, the patient was 19 weeks pregnant. The bosom growth had the clinical and US part of PT. A center needle biopsy was gotten, affirming a harmless PT, and nearby extraction was performed with no postoperative intricacies. The last pathology report showed a marginal PT with close resection edges of 1 mm.
Keywords
Phyllodes tumor; Breast; Borderline; Malignant; Pregnancy
Introduction
Phyllodes cancer (PT) is an intriguing bosom growth with heterogenous way of behaving relying upon the pathology highlights. Harmless PTs can mirror bosom fibroadenoma yet can repeat in the event that they are not extracted with significant spaces. In addition, a few PTs can give marginal science or can act as dangerous sarcomatous bosom growths that effectively metastasize remotely. Customarily, PTs are ordered by their histologic elements into harmless, fringe, and harmful [1]. As per cases that have been accounted for, all PTs might repeat, yet all at once just the fringe and harmful PT can metastasize. PT was initially portrayed by Johannes Muller in 1838 as “cystosarcoma phyllodes”, yet these days the World Health Organization (WHO) has embraced the term PT, after in excess of 60 names that were utilized to portray these cancers. The typical frequency each year in the U.S.A. is around 2.1 per million ladies. Latina white ladies appears to have a higher pace of PTs contrasted and non-Latina white, Asian, and African American ladies. PTs are related with Li Fraumeni condition, an intriguing disorder [2] described by the improvement of numerous sarcomatous cancers.
PTs generally happen as a bosom bump or inadvertent tracking down on a ultrasound (US) assessment. Clinical highlights incorporate an obvious bosom mass, standard or lobulated. Ordinarily, the bosom knot is firm, portable, and effortless, with a cancer size going from 1 cm to more than 10 cm. Different changes, similar to areola withdrawal, ulceration, areola release, or growth obsession with chest wall are normal. Nonetheless, axillary metastases are unprecedented, and the majority of the obvious axillary lymph hubs [3] are receptive, non-metastatic. Around 20% of PTs are analyzed by screening mammograms as lobulated masses, very like fibroadenomas on imaging. Pathology assessment stays the highest quality level for the analysis of PT. A center biopsy or excisional biopsy [4] are utilized for conclusion. Fine needle yearning isn’t suggested for PT since it is less exact and may not be demonstrative. The finding of PT depends on the combination of morphology highlights, however stays testing, especially in the qualification from fibroadenomas.
Case presentation
A 32-year-old female, primigravida, at 38 weeks of growth, gave a huge expanding of the left bosom developing for the last eight months. The mass was little in size when she originally took note eight months back and quickly expanded in size during the course of pregnancy (Figure 1). The mass was related with serious inconvenience due to its size and weight and was excruciating [5]. There was no history of injury, past bosom infection or family background of bosom disease. Actual assessment of the left bosom uncovered a huge enlarging possessing every one of the quadrants of the bosom, especially immense in the average upper and lower quadrants and extending the overlying skin furthermore, uprooting the areola complex [6] towards the left sidelong side. The skin was pigmented; expanded veins were seen with peaude-orange appearance. There was nearby warmth. The expanding was nodular with extending and hyper pigmentation of the overlying skin. The expanding was 10 x 20 cm in size, nodular surface and firm in consistency with areas of delicate quality. It was portable and was not fixed to the fundamental tissues [7]. Bosom was lactating and milk discharge through the left areola was noticed.
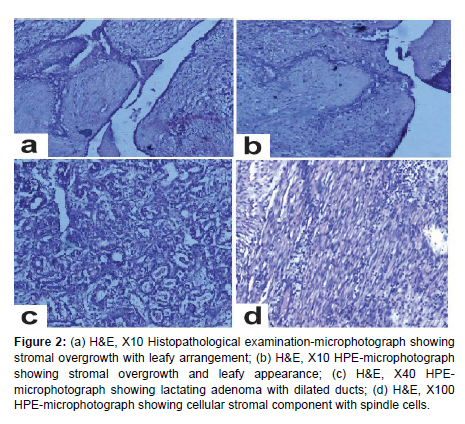
There was no huge extension of axillary lymph hubs. The contralateral bosom assessment showed a little (1 x1 cm) firm, portable mass in the lower external quadrant of the bosom. Right axilla was typical. Ultrasonographic assessment showed huge clear cut strong, heterogenous, transcendently hypoechoic lobulated sore [8] with inner vascularity in the left bosom and a little hypoechoic injury in the right bosom conceivably fibroadenoma. Ultrasound directed Trucut Biopsy (Figure 2) was performed and the cytological study uncovered a fibroepithelial injury reminiscent of harmless phyllodes cancer.
Figure 1: (a) H&E, X10 Histopathological examination-microphotograph showing stromal overgrowth with leafy arrangement; (b) H&E, X10 HPE-microphotograph showing stromal overgrowth and leafy appearance; (c) H&E, X40 HPEmicrophotograph showing lactating adenoma with dilated ducts; (d) H&E, X100 HPE-microphotograph showing cellular stromal component with spindle cells.
Differential finding of a harmless phyllodes growth, goliath fibroadenoma and lactating adenoma were thought of and due to the clinical elements a temporary determination of harmless phyllodes growth was considered and anticipated straightforward mastectomy. She conveyed a live solid child by elective cesarean segment [9]. Later that lactation was started, the side effects deteriorated with expanded weight and delicacy over the left bosom.
The treatment choices and timing of the activity were examined and in view of the diffuse idea of the injury and enormous size, straightforward mastectomy was chosen and was finished in no less than multi week after conveyance under general sedation, through cross over circular cut. The areola complex that was sans sickness, was collected as full thickness unite and was relocated at the devoted site while doing the injury conclusion. This is finished for mental purposes behind the patient and stylish contemplations. Wound was shut with 4/0 PDS subcuticular stitch.
Discussion
Phyllodes growths are uncommon fibroepithelial bosom cancers that are equipped for a different scope of natural way of behaving. These growths were initially called “Cystosarcoma Phyllodes” by Johannes Muller in 1838. They could act like harmless fibroadenomas or indeed, even can metastasize indirectly. Nonetheless, the term is wrong, since it is seldom cystic and sarcomatous with metastases. The term ‘Phyllodes’ signifies the histological appearance of leaf-like papillary projections [10] that signifies stromal multiplication. Phyllodes growths represent under 0.5% of all bosom neoplasms. Not very many cases are accounted for in pregnancy. Goliath growths are those a bigger number of than 10 cm in measurement and in excess of 500 gm in weight. They represent almost 20% of all phyllodes growths. Phyllodes growth generally gives a clinically harmless expanding that might develop quickly. Relationship of these growths in pregnancy and lactation is strange and a not many cases are accounted for in the writing. Overlying skin is extended, pale blue staining and expanded veins are seen clinically. Axillary lymphadenopathy is generally not present even in enormous cancers. Such growths are not detailed somewhere else in the body. Not many cases are accounted for with comparable histopathology in vulvar area most conceivably from the ectopic mammary tissue. Depending upon the level of stromal development, stromal cellularity, cell atypia furthermore, the idea of cancer borders, phyllodes growths are delegated harmless, fringe and threatening. Wide extraction with 1 cm edge is generally suggested. Straightforward mastectomy is demonstrated in huge sores including the vast majority of the bosom tissue.
Conclusion
It was truly challenging for histopathologists to separate harmless phyllodes growth from monster fibroadenoma due to related pregnancy and lactational changes in the mammary tissue, so cautious review is required while making a finding.
Acknowledgement
The authors are grateful to the Mahidol University, for providing the resources to do the research on breast cancer.
Conflicts of Interest
The authors declared no potential conflicts of interest for the research, authorship, and/or publication of this article.
References
- Lenhard MS, Kahlert S, Himsl I, Ditsch N, Untch M, et al. (2008) Phyllodes tumour of the breast: clinical follow-up of 33 cases of this rare disease. Eur J Obstet Gynecol Reprod Biol 138: 217-221.
- Blaker KM, Sahoo S, Schweichler MR, Chagpar AB (2010) Malignant phylloides tumor in pregnancy. Am Surg 76: 302-305.
- Way JC, Culham BA (1998) Phyllodes tumour in pregnancy: a case report. Can J Surg 41: 407409.
- Sharma JB, Wadhwa L, Malhotra M, Arora R, Singh S (2004) A case of huge enlargement of cystosarcoma phylloides of breast in pregnancy. Eur J Obstet Gynecol Reprod Biol 115: 237-239.
- Nejc D, Pasz-walczak G, Piekarski J, Pluta P, Bilski A, et al. (2008) Astonishingly rapid growth of malignant cystosarcoma phyllodes tumor in a pregnant woman-a case report. Int J of Gynecol Cancer 18: 856-859.
- Mrad K, Driss M, Maalej M, Romdhane KB (2000) Bilateral cystosarcoma phyllodes of the breast: A case report of malignant form with contralateral benign form. Ann Diagn Pathol 4: 370-372.
- Vorherr H, Vorherr UF, Kutvirt DM, Key CR (1985) Cystosarcoma phyllodes: Epidemiology, pathohistology, pathobiology, diagnosis, therapy, and survival. Arch Gynecol 236: 173-1781.
- Karim RZ, Gerega SK, Yang YH, Spillane A, Carmalt H, et al. (2009) Phyllodes tumours of the breast: a clinicopathological analysis of 65 cases from a single institution. Breast 18: 165-170.
- Sugie T, Takeuchi E, Kunishima F, Yotsumoto F, Kono Y (2007) A case of ductal carcinoma with squamous differentiation in malignant phyllodes tumor. Breast Cancer 14: 327-332.
- Soumarová R, Seneklová Z, Horová H, Vojkovská H, Horová I, et al. (2004) Retrospective analysis of 25 women with malignant cystosarcoma phyllodes-treatment results. Arch Gynecol Obstet 269: 278-281.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Miliou T (2022) Unsafe Phyllodes Tumor of the Breast and Pregnancy. Breast Can Curr Res 7: 169. DOI: 10.4172/2572-4118.1000169
Copyright: © 2022 Miliou T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.