Unruptured Removal of Giant Intracranial Hydatid Cyst in a 6 Year Old Child
Received: 29-Jul-2018 / Accepted Date: 14-Aug-2018 / Published Date: 23-Aug-2018 DOI: 10.4172/2572-4983.1000162
Keywords: Hydatid disease; Giant intracranial hydatid cyst
Case Report
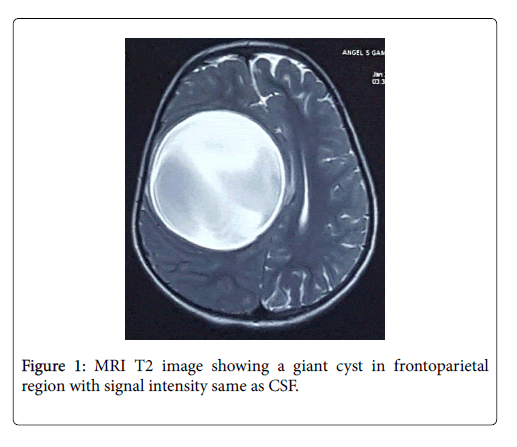
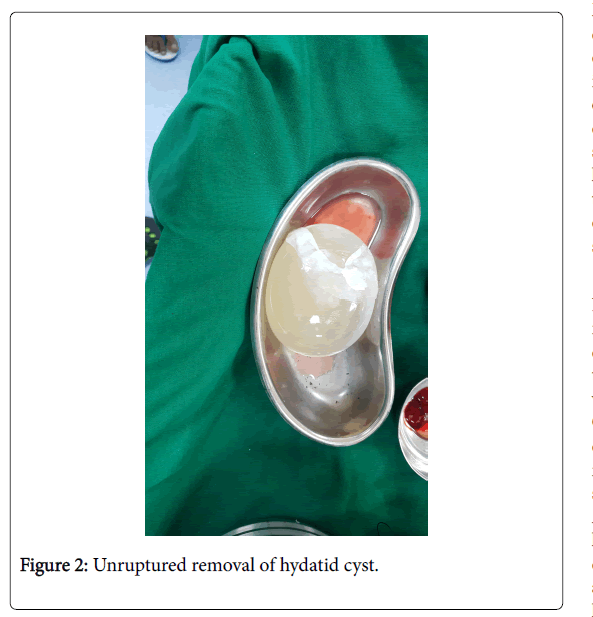
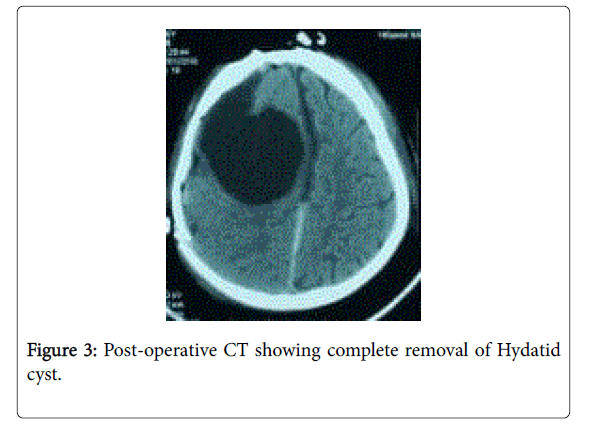
A 6 year old girl presented with history of holocranial headache since 3 months. Since 2 months she complained of intermittent nausea and vomiting. She developed left sided weakness before 1 month. Before 1 week of presentation she developed left focal seizures with secondary generalization. On clinical examination she was conscious alert and following commands. Her higher mental functions were normal and she had no cranial nerve deficits. Tone was normal in all 4 limbs with reduced power of 3/5 in left upper limb and lower limb. She had no sensory deficits and her plantar were flexors in both limbs. Fundoscopy revealed bilateral papilloedema. Laboratory investigations were normal. Chest x-ray and abdominal ultrasonography were normal. Magnetic Resonance Imaging showed a 10 x 8 cm lesion in the right frontoparietal region. Lesion was hypointense on T1, hyperintense on T2 with no enhancement on contrast (Figure 1). The lesion caused displacement of midline structures towards left side, compressing left lateral ventricles leading to hydrocephalus with subfalcine and transtentorial herniation. She underwent right frontotempero- parietal craniotomy with osteoplastic bony flap. On opening dura brain was tense and bulging. Dowlings technique of hydrodissection was used to remove the hydatid cyst intact without the spillage of its contents. After the removal of cyst brain was lax and pulsatile. Watertight dural closure was done, bone flap was replaced and skin was closed in layers. Pathological examination confirmed hydatid cyst (Figure 2). Antibiotics and anti-epileptics were given in the post-operative period. Her post-operative stay in the hospital was uneventful and was discharged after 7 days. Post operatively she was started on albendazole 15 mg/kg/day for 4 weeks. At 3 months follow up she has no complaints and no neurological deficits (Figure 3).
Discussion
Hydatid cyst is an anthropozoonotic disease caused by Echinococcus Granulosis. Humans are intermediate hosts caused by the larval stage of echinococcus tapeworm. This parasite is incidentally ingested through contaminated food or beverages from faeces of infected animals. The eggs hatch inside the intestines, penetrate the walls; enter the hepatic capillaries via portal and mesenteric venous system. It reaches the liver to form cysts or progress further towards the lungs. Once in systemic circulation it can penetrate the pulmonary filter and end up forming cysts in any part of body including brain, heart, orbit or bones. It is endemic to many regions worldwide like Australia, New Zealand, South America, Middle East, Central and South Europe.
Brain cysts are uncommon and accounts for 1-2% of all hydatid cysts infection [1]. Primary brain cysts are solitary while secondary cyst due to rupture of cardiac cysts or iatrogenic rupture in brain; are multiple. 90% of intracranial cysts are solitary mainly localised to middle cerebral artery territory in supratentorial region although it can be seen in intraventricular or infratentorial region. Hydatid cyst mainly affects children but is presented in adulthood. The growth rate of cyst is believed to be 1.5 to 10 cms per year [2].
Serological tests like enzyme-linked immunosorbent assay or indirect hemagglunition can be used to diagnose Hydatid Cyst. False negative rates are higher in these serological tests due to minimal tissue response by brain parenchyma. Computed Tomography (CT) and Magnetic resonance imaging (MRI) are preferred diagnostic tools for detection of intracranial Hydatid cyst. CT and MRI imaging demonstrate a thin walled well defined oval or cystic mass with signal intensity or attenuation similar to that of cerebrospinal fluid. Wall enhancement is absent after IV administration of contrast and calcification is rare. The cyst may cause compression of the ventricular system leading to hydrocephalus and cerebral herniation. Hydatid cyst lacks surrounding oedema seen particularly with abscesses and cystic tumors [3]. Differential diagnosis includes arachnoid cysts, epidermoid cyst, porencephalic cysts, neurological cysts and expanded perivascular spaces [4].
Main treatment consists of entire removal of cyst without rupture. Hydrodissection technique by Dowling Orlando is used for cyst removal in which head of the operating table is lowered and cyst is delivered by passing saline between the cyst and surrounding brain tissue [5]. Modified Dowling technique by Arana-Iniguez involves valsalva maneover and counter pressure to surrounding brain tissue. Complications associated with this surgery are due to rupture of cysts causing anaphylactic reactions, meningitis or possible recurrences of multiple cysts due to spillage. 1 ml of hydatid sand contains 400,000 scolises hence even minimal spillage can lead to catastrophic events. Adhesions to brain parenchyma, thin cyst wall and periventricular locations can be real challenges to the operating surgeon. When large cysts are removed it can lead to subdural collections, cortical collapse and porencephalic cysts. Mass effects from these lesions may require a low pressure shunt.
Albendazole alone or in combination wtih agents like Praziquantal for 4 weeks or more is the preferred adjuvant therapy or in certain circumstances primary mode of treatment for hydatid cyst. Some authors also recommend these agents for longer periods however its benefit over 4 weeks yet remains to be established.
Conclusion
Treatment of hydatid cyst depends upon the location, number of cysts, size of cyst and neurological deficits due to mass effect of cysts. Unruptured removal of cyst and adjuvant therapy with albendazole holds the key for elimination of Hydatid cyst.
References
- Erashin Y, Mutluer S, Guzelbag E (1993) Intracranial hydatid cysts in children. Neurosurgery 33: 219-225.
- Seirra J, Oriedo J, Berthier M, Leiguarda R (1985) Growth rate of secondary hydatid cyst of the brain. J Neurosurgery 62: 781-782.
- Andronikou S, Welman C, Kader E (2002) Classic and unusual appearances of hydatid diseases in children. Pediatr Radiol 32: 817-828.
- Waziri TM, Bollineni V, Kadi R, De Mey J (2017) A giant intracranial hydatid cyst in an eleven-year-old boy. J Belg Soc Radiol 101: 6.
- Carrea R, Dowling E Jr, Guevara JA (1975) Surgical treatment of hydatid cysts of the central nervous system in pediatric age (Dowling's technique). Child’s Brain 1: 4-21.
Citation: Modi MN, Shah R, Vaidya J, Vyas P, Choraria N (2018) Unruptured Removal of Giant Intracranial Hydatid Cyst in a 6 Year Old Child. Neonat Pediatr Med 4: 162. DOI: 10.4172/2572-4983.1000162
Copyright: © 2018 Modi MN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4501
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 3721
- PDF downloads: 780