Unilateral Absence of Left Pulmonary Artery with Absent Pulmonary Valve Syndrome: Surgical Perspective on Primary Repair
Received: 08-Jun-2021 / Accepted Date: 22-Jun-2021 / Published Date: 29-Jun-2021 DOI: 10.4172/jcpr.1000144
Abstract
Tetralogy of Fallot (TOF) with absent pulmonary valve and unilateral absence of pulmonary artery is an extremely rare congenital cardiac anomaly. Historically, the outcome of surgery in this subset has been very dismal. We believe valveless reconstruction for Right Ventricular Outflow Tract (RVOT) as a part of primary repair should never be opted for in this variant. Only a fully competent and durable valve in RVOT can provide meaningful early and time related survival in this variant. We report our experience with a bi-leaflet pulmonary valve constructed from 0.1 mm PTFE membrane in this substrate.
Keywords: Tetralogy of Fallot (TOF); Absent left pulmonary artery; Absent Pulmonary Valve (APV); Congenital heart surgery
Introduction
Tetralogy of Fallot (TOF) with Absent Pulmonary Valve (APV) and Unilateral Absence of Pulmonary Artery (UAPA) is a rare congenital cardiac anomaly. Till now only 17 cases have been reported in the literature [1-3]. Surgical correction carries a very high mortality, with sudden cardiac deaths reported in almost all of the patients [2]. Right Ventricle (RV) is destined to acute failure or sub-acute failure after surgery with valveless reconstruction of Right Ventricular Outflow Tract (RVOT). We believe valveless reconstruction of RVOT as a part of primary repair should never be opted for, in this variant. We present 4 year follow up of a patient with this variant, who underwent total correction with construction of bi-leaflet Pulmonary Valve (PV) using a 0.1 mm Polytetrafluorethylene (PTFE) membrane.
Case Study
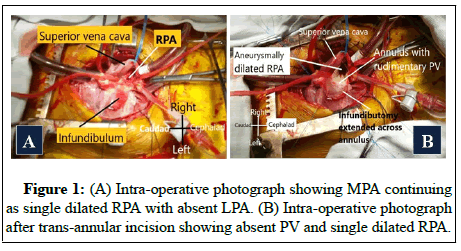
Informed written consent was taken from the guardian for publication. A two year old male child was brought with the history of dyspnea and cyanosis on mild exertion since 3 months of age. Patient had cyanosis and a to and fro murmur was present at the left upper sternal border. Chest X-ray revealed mild cardiomegaly, hypoplastic left lung and prominent right hilar shadow. Echocardiography revealed TOF morphology, large subaortic Ventricular Septal Defect (VSD) with severe Pulmonary Stenosis (PS). Also dilated Main Pulmonary Artery (MPA) was seen with continuation only as a dilated Right Pulmonary Artery (RPA), suggestive of absent Left Pulmonary Artery (LPA). Neither PDA nor any major collateral supplying the left lung could be appreciated on aortography. Pulmonary vein wedge injection also confirmed its absence. No obvious compression of airway on the right side could be appreciated on CT scan. Child underwent successful total correction. Intra-operatively, pulmonary annulus was mildly stenotic, RPA was aneurysmally dilated and PV was rudimentary (Figures 1A and 1B).
After minimal infundibular resection, VSD was closed with 5/0 polypropylene, TF needle, using continuous suture technique. As the annulus was small, the infundibular incision was extended onto MPA to a limited extent.
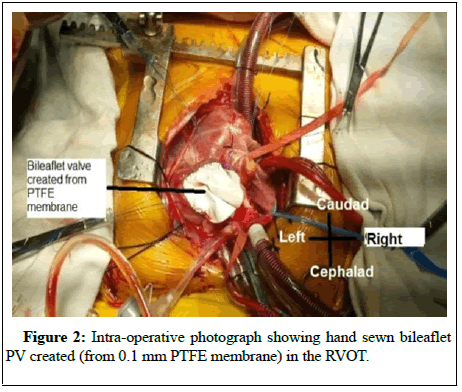
In view of absence of airway symptoms and absence of LPA, the dilated RPA was only partially plicated. RVOT reconstruction was done by creating a bileaflet valve from 0.1-mm PTFE membrane using Graham Nunn technique (Figure 2) and augmentation of RVOT by a rectangular patch of treated pericardium [4].
Trans-Esophageal Echocardiography (TEE) revealed mild Pulmonary Regurgitation (PR) with peak gradient of 22 mmHg. Postoperative course was uneventful. At 4 years follow up, patient is asymptomatic with preserved RV function.
Discussion
Absent Pulmonary Valve Symdrome (APVS) is characterized by a rudimentary PV and aneurysmal dilatation of central pulmonary arteries [5]. It occurs in 2.4% to 6.3% of patients with TOF [6] Coexistence of APV with complete absence of the LPA is extremely rare. Till now only 17 patients of APVS with TOF and complete absence of left PA has been reported [1-3]. Complete absence of RPA in association with APVS has never been reported [2].
Cardiac catheterization and angiography are usually diagnostic. As the entire right ventricular stroke volume is directed to the unilateral pulmonary artery, aneurysmal dilatation of connected PA can occur early and be more pronounced. Timing of surgical intervention is dictated by clinical status as well as onset of RV dysfunction.
There is no consensus regarding reconstruction of RVOT is concerned, considering the rarity of this variant. Unlike other variants of TOF, valveless reconstruction of RVOT is bound to fail early in this subset. RV dysfunction may occur by combination of Pulmonary Regurgitation (PR) and a single pulmonary artery, which may result in pulmonary hypertension. This will worsen PR, creating a vicious cycle ultimately leading to early onset of RV dysfunction [7]. Co existence of free PR , single lung for RV outflow and borderline Pulmonary Vascular Resistance (PVR), all will cause acute or subacute RV dysfunction, if valveless reconstruction is opted for.
We believe construction of a fully competent valve is a must in the primary surgery itself. Fuad Abbag reported RV dysfunction as early as three years after transannular patch using bovine pericardium. Valved pulmonary homograft was placed after 3 years to avoid further impairment of RV2. Conduit repair can provide a competent valve in pediatric age group, but it has inherent problems. Other options include PV constructed from pericardium or 0.1 mm PTFE membrane. In view of sudden deaths reported in vast majority of these patients in follow up, we believe durability of the valve is also of paramount concern. Graham, et al. reported that all the pericardial valves constructed by them for RVOT developed free PR whereas the bileaflet PTFE (0.1 mm) valves have remained competent with regurgitant fractions of only 5% to 30% and this has remained stable with time [4]. Our patient, even at 4 years of follow up is showing mild PR with preserved RV function.
Conclusion
To conclude, high mortality in this variant of TOF is expected. Primary repair must include construction of a competent and durable PV, preferably using 0.1 mm PTFE membrane in the primary surgery itself.
References
- McCaughan BC, Danielson GK, Driscoll DJ, McGoon DC (1985) Tetralogy of Fallot with absent pulmonary valve: Early and late results of surgical treatment. J Thorac Cardiovasc Surg 89: 280–287.
- Abbag F (2006) Unilateral absence of a pulmonary artery in absent pulmonary valve syndrome: A case report and review of literature. Ann Thorac Cardiovasc Surg 12: 368–372.
- Avsar, M.K., Demir, T, Demir, H.B (2015) Absence of left pulmonary artery in tetralogy of fallot with absent pulmonary valve syndrome. J Card Surg 30: 104-107.
- Nunn GR, Bennetts J, Onikul E (2008) Durability of hand-sewn valves in the right ventricular outlet. J Thorac Cardiovasc Surg 136: 290–296.
- Kirshbom PM, Kogon BE (2004) Tetralogy of Fallot with absent pulmonary valve syndrome. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 7: 65–71.
- Rao BN, Anderson RC, Edwards JE (1971) Anatomic variations in the tetralogy of Fallot. Am Heart J 81: 361–371.
- Pool PE, Vogel JH, Blount Jr SG (1962) Congenital unilateral absence of a pulmonary artery: The importance of flow in pulmonary hypertension. Am J Cardiol 10: 706–732.
Citation: Mahajan S, Khanna S, Patel R, Halder V, Bansal V (2021) Unilateral Absence of Left Pulmonary Artery with Absent Pulmonary Valve Syndrome: Surgical Perspective on Primary Repair. J Card Pulm Rehabil 5: 144. DOI: 10.4172/jcpr.1000144
Copyright: © 2021 Mahajan S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2693
- [From(publication date): 0-2021 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 2032
- PDF downloads: 661