Unexpected Presentation of a Twenty Year Old Orbital Floor Reconstruction
Received: 23-Aug-2016 / Accepted Date: 24-Aug-2016 / Published Date: 31-Aug-2016 DOI: 10.4172/2161-119X.1000260
252813Introduction
A thirty-nine year old man presented with a six month history of persistent infra-orbital infection which had failed to resolve following multiple courses of oral antibiotics.
Examination revealed an erythematous swelling with an associated discharging sinus within the right infraorbital crease alongside diplopia in strained upward gaze. Pupillary levels were equal however the lower right eyelid was depressed and exhibited a historical scar.
Further questioning revealed a history of post-traumatic orbital floor reconstruction twenty years prior to presentation.
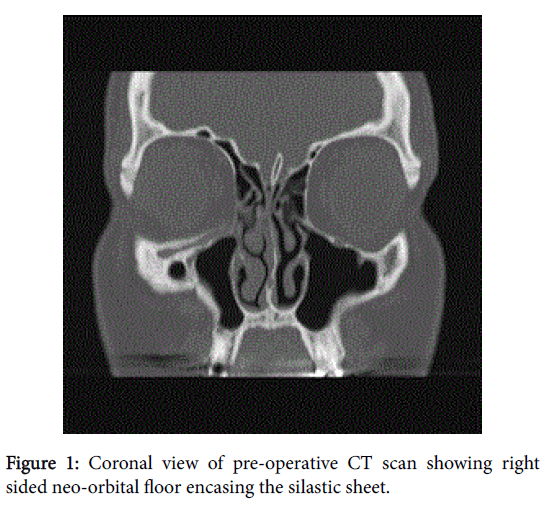
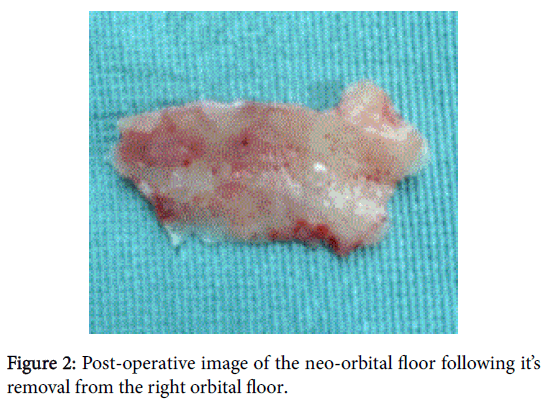
Computed tomography imaging unexpectedly revealed two separate orbital floors (Figure 1) thought to have formed secondary to a silicone sheet reconstruction. Both the new orbital floor (Figure 2) and the implant were removed and histopathological results revealed only chronic suppurative granulation tissue. Post-operatively the infection had resolved, however no improvement was seen regarding his diplopia.
Several materials are available for reconstructing orbital floor defects, including autologous bone grafts, silicone elastomer, porous polyethylene, titanium mesh and more recently PEEK.
Although cheap and easily accessible, silicone elastomers are associated with a higher complication rate making their current use controversial [1].
Frequently reported complications include persistent pain, chronic infection, migration, and extrusion of the implant [2]. Other reported complications include dacryocystitis, skin fistula, orbit maxillary communications and cyst formation [3].
Morrison et al reviewed 311 patients reconstructed with silastic implants and found that implant removal was necessary in 13.2% of patients due to persistent infection, pain, extrusion, and diplopia [2] Yun et al conducted a review of 115 patients treated with silastic sheets; 4.3% needed implant removal due to infection, hematoma, displacement, or extrusion, with a mean removal time of 23.3 months [4].
The majority of post-implantation silicone complications become evident in the early post-operative phase, but complications have been reported up to 31 years later [2,5] However, to our knowledge no report of a secondary orbital floor formation has ever been made.
This case highlights the importance of being vigilant of potentially rare underlying causes of infection whilst having an awareness of historical treatment methods and how they can still impact upon current practice.
References
- Moon SJ, Suh HS, Park BY, Kang SR (2014) Safety of Silastic Sheet for Orbital Wall Reconstruction. Archives of Plastic Surgery 41: 362-365.
- Morrison AD, Sanderson RC, Moos KF (1995) The use of silastic as an orbital implant for reconstruction of orbital wall defects: review of 311 cases treated over 20 years. J Oral MaxillofacSurg 53: 412–417.
- Bourgault S, Bordua-Robert M, MolgatYM (2001) Recurrent orbital cyst as a late complication of silastic implant for orbital floor fracture repair. Can J Ophthalmol 46: 368-369.
- Yun HK, Yi S, Joh SP, Ahn ST, Lim P (2001) Complications after open reduction of blow-out fracture using silicone sheet. J Korean Cleft Palate-CraniofacAssoc 2: 72–76.
- Verma, S, Garg A,Nastri A (2014) Orbitomaxillary mass after repair of the orbital floor. Br J Oral MaxillofacSurg 52: 977-979.
Citation: Davies I, Chambers P (2016) Unexpected Presentation of a Twenty Year Old Orbital Floor Reconstruction. Otolaryngol (Sunnyvale) 6:260. DOI: 10.4172/2161-119X.1000260
Copyright: ©2016 Davies I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 9927
- [From(publication date): 8-2016 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 9284
- PDF downloads: 643