Understanding Quality of Life in African Americans with Lupus (UQAN) in South Carolina
Received: 07-Jun-2018 / Accepted Date: 05-Jul-2018 / Published Date: 09-Jul-2018 DOI: 10.4172/2161-0711.1000620
Keywords: African americans; Women’s health; Interviews psychological; Stress physiological; Lupus erythematosus systemic
Introduction
In lupus and other autoimmune diseases, the immune system loses its ability to differentiate between foreign substances and its own cells and tissues, causing the body to attack itself. Lupus has a wide spectrum of clinical presentations, which are characterized by remissions and exacerbations. Systemic Lupus Erythematosus (SLE) is the most diverse of the autoimmune diseases because it can affect any part of the body, although most commonly the skin, joints, blood, and kidneys, and can be life-threatening [1]. There are approximately two million people in the United States who suffer from SLE, but it is estimated that only 500,000 to 1.5 million Americans have been formally diagnosed with lupus. More than 16,000 Americans develop lupus each year. Young women are most frequently affected by the disease, outnumbering male patients ten to one [2]. The disease usually strikes between the ages of 15 and 40 years, and African Americans are at particularly high risk for the disease. In the United States, African Americans have three-fold higher incidence and prevalence rates of SLE, as well as cause-specific mortality rates, compared with whites [3-6].
Psychosocial stress is believed to be positively associated with lupus disease activity due to its ability to compromise immune function. Recommendations to lupus patients to avoid stress are based on numerous studies that have demonstrated associations between daily stress and disease exacerbations [7-11]. Daily stress is related to impairments involving visual memory, fluency and attention in patients with SLE [10]. Very little is known about the impact of psychosocial stress on underlying biological mechanisms, although data indicate that lupus patients differ from healthy controls in stressinduced immune responses [7-11]. Even less is known about this phenomenon in African American lupus patients, although, as a group, African Americans display the highest rates of lupus. Due to the exposure of African Americans to a unique trajectory of stressors throughout their life course, it may be critical to address this area as a contributor to disease development and severity in this high risk group.
A large body of evidence has shown that health-promoting programs in stress management have been successful in helping people improve their health practices and related health conditions [12].
Based on reviews of scientific literature, investigators have suggested that therapeutic interventions should be proposed to reduce psychological distress to improve quality of life and possibly moderate the evolution of chronic and unpredictable diseases like SLE [11]. Such techniques have resulted in short-term improvement in pain, psychological function, and perceived physical function among persons with SLE [12]. Two programs that have been shown to be successful in improving conditions in patients with arthritis are the Arthritis Self- Management Program (ASMP) and the generic Chronic Disease Self-Management Program (CDSMP). Each program incorporates six weeks of peer led sessions, including both diseasespecific and more general self-help content.
Arthritis self-management education delivered by small-group, home study, computer, and Internet modalities have demonstrated significant improvements in health distress, self-reported global health, and activity limitation, with trends toward improvement in selfefficacy and mental stress management [12-36]. Consequently, numerous national agencies have recommended arthritis selfmanagement education to complement medical care [37]. Despite these recommendations, arthritis self-management education has reached only a limited number of people.
Therefore, the ultimate goal of the Understanding Quality of Life in African Americans with Lupus (UQAN) Project is to generate strategies for more effective expansion of and increased participation in critical health promotion initiatives to populations in South Carolina that need them most (namely African Americans with lupus). This project elicited responses from the target population to assess what motivates them to engage in or keeps them from participating in such public health services, and what influences their decision to participate or not. This project has very high potential impact because of the likelihood that its findings can be rapidly translated into improved delivery of health care with relevance to health disparities. If widely implemented, morbidities and mortality related to lupus overall could be drastically reduced, since African Americans make up the largest portion of lupus cases. The potential economic impact of such a project is considerable since previous studies have observed that group psychotherapy for medical patients can reduce costs for medical care [37] and that patients in intervention groups had fewer emergency room visits, hospitalizations and nights in the hospital [38,39].
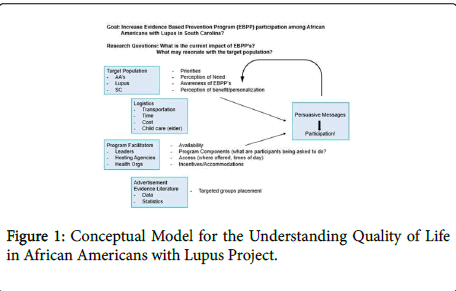
The conceptual model (Figure 1) guiding the UQAN Project includes two levels of participants; the target population and program facilitators. Characteristics of the target population are African American race/ethnicity, lupus disease status, and South Carolina residence.
Program facilitators are program leaders, hosting agencies, and health organizations. Considerations of the target population include their priorities, perceptions of need and/or benefit, and awareness of evidence based prevention programs (EBPP’s). Personal factors/ characteristics, such as personality type (e.g., introversion/ extroversion), depression, hopelessness, social support, and lack of trust are also important. Additional logistical considerations of the target population include transportation, time, cost, and child or elder care. Considerations of the program facilitators include availability of programs, program components or what program participants are being asked to do, access to programs (i.e., where and when they are offered), and tangible incentives/accommodations. Also connected to the program facilitator group are decisions related to advertisement of programs, which include evidence/data and statistics reflected in scientific and lay literature, placement, and groups targeted. Considerations of both groups can be combined to generate persuasive messages that increase participation. This conceptual model is informed by community-institution partnership standards for achieving success while maximizing the benefits of the communitybased participatory research (CBPR) approach. These include focusing research questions on health issues of greatest relevance to the communities at highest risk, thus increasing the relevance of intervention approaches and subsequent likelihood of success [40-43].
To assess what influences decisions of African Americans with lupus in South Carolina to participate in EBPP’s or not, the following research questions were addressed:
What is/are the most important individual (i.e. personally mediated) factors that determine acceptability and utilization of health promoting programs among African Americans with lupus in South Carolina?
What are the most important, interpersonal (i.e. peer or familial) factors that determine acceptability and utilization of health promoting programs among African Americans with lupus in South Carolina?
What are the most important community level factors that determine acceptability and utilization of health promoting programs among African Americans with lupus in South Carolina?
Methods
Research design
The reported qualitative study was designed to assess the reach of evidence based prevention programs in African Americans with lupus in South Carolina. Interviews were used to elicit information about the most important individual (i.e. personally mediated), interpersonal (i.e. peer or familial), and community level factors that determine acceptability and utilization of health promoting programs among African Americans with lupus in South Carolina. Study participation involved patient participation in one interview and collection of responses from patients that were analyzed for themes to be shared with key stakeholders. Two interviews were held to obtain this information.
Recruitment
Purposeful random sampling was used to select a smaller group within the target population of African Americans with lupus in South Carolina. Patients invited to participate in interviews were African American lupus patients enrolled in the “SLE Clinic Database Project”at MUSC. There are 364 patients in the web-based database, but out of the 364, only 177 have consented to have multiple visits. All 177 patients have consented to be re-contacted for future studies. All patients have American College of Rheumatology (ACR) criteria and disease activity information available, as well as quality of life measures obtained in the database questionnaire. This cohort includes 162 females and 15 males, of which 128 are African American, 43 are Caucasian, four are Hispanic, and two are Native American. Fifty-one of the 177 are also enrolled in the SLE in Gullah Health (SLEIGH) Study. This group of 51 patients is comprised entirely of African Americans whose grandparents were born in the Sea Island areas of South Carolina or Georgia.
Recruitment efforts were limited to participants residing in areas where EBPP’s are offered. Eligible patients were contacted by phone, informed about the project, and invited to participate. Phone attempts were made until target recruitment (n=2) was achieved. Participants who agreed to participate chose the date, time, and location most convenient for them for the interview.
Interviews
The interviewer provided incentives and obtained oral informed consent at the time of the interview. Each interview was recorded with prior permission of participants. Interview questions focused on health promotion practices, individual participants’ practices, participants’ beliefs and attitudes about EBPP’s, barriers in seeking health promoting programs, and disease-related stress (see Appendix A). For instance, health promotion practices include those that are addressed as part of EBPP’s (e.g., What types of things do you do to relieve stress/ pain?). Individual participants’ practices include adoption of any of those identified techniques/strategies. Participants’ beliefs and attitudes include theories about the effectiveness of EBPP’s (e.g., What types of activities do you believe really work to relieve stress/pain?). Barriers to seeking health promotion programs include cost, time, transportation, child care, and not knowing where to go (e.g., What types of things keep you from pursuing the activities you believe really work to relieve stress/pain?). Disease-related stress includes complicated therapeutic and care regimens and difficulty managing flares (e.g., What are some of the most difficult aspects of your disease experience?). In addition, participants were encouraged to talk about problems that were not identified, but they felt were important.
Analytical methods
A digital audio file of both interviews was transcribed verbatim into Microsoft Word. The interviewer listened to each audio file while reading the transcribed text file to verify accuracy and that identifying information was removed. Edits to the text file were made accordingly. The manually coded transcript was then entered into QSR NVivo 10 (Qualitative Solutions and Research, Pty Ltd, Victoria, Australia), a software program, for managing, coding, analyzing, and retrieving qualitative data. An emergent coding strategy was used to code the data. Text was sorted into a short list of categories or “significant statements” that were determined by matching text segments in the database. An initial set of five to six categories with shorthand labels or codes was expanded as the text in the database was reviewed and rereviewed. Assigned code names or labels were a mixture of language directly from participants, health sciences terminology, and any other names that best described the information.
In the classification of textual data, initial categories were reduced and combined into three themes or “meaning units” that are used to present results. The data that was coded and developed into themes was the individual experiences of one participant and the context of those experiences, with respect to their knowledge of and interaction with evidence based prevention programs (EBPP’s) aimed at improving quality of life.
Ethics
This study conforms to the Declaration of Helsinki and was approved by the institutional review board (IRB) at the University of South Carolina (USC). The interviewer provided incentives and obtained oral informed consent at the time of the interview. Each interview was recorded with prior permission of participants.
Results
Study findings reflect factors that influence the decisions of two African American women with lupus in South Carolina to participate in EBPP’s or not, including important individual, interpersonal, and community level factors. These findings are presented here under three general topics: 1) Perceptions of stress; 2) Activities to reduce stress; and 3) Cost as a barrier (Table 1). Each of these findings was supported by multiple references from the participants. A brief thematic narrative of the findings follows.
| 1. Perceptions of stress |
| • Frustration • Pain • Inability to concentrate • Work • Worry |
| 2. Activities to reduce stress |
| Physical activity • Being outdoors • Medication • Sleep, rest, relaxation • Time with friends and family |
| 3. Cost as a barrier |
| 4. Esteem and physical appearance/ability |
| 5. Providing explanation |
Table 1: Summary of Thematic Findings.
Narrative of findings
Perceptions of stress. The participants shared various feelings and situations they associated with stress, which included both mental and physical attributes. These included frustration, pain, inability to concentrate, work, and worry:
“Body hurting, my body hurting real bad, um mental stress or mental strain, uh not feeling well, um emotionally crippled, because I can’t think straight, um worry, frustration, um can’t sleep, when I hear the word stress”.
“Primarily aggravation… when someone gets on my nerve it goes and goes for hours and it turns into stress and then there goes the physical.”
Activities to reduce stress. Both participants went on to describe the kinds of activities that work to reduce stress for her, and one of which included both personal and community activities:
“What do I do? Um right now I I try to rest, and in terms of rest, I I like to read, I like to um watch a funny cartoon, um I like to sleep, um I try to sleep as much as I can, it’s hard sometimes, um um I talk to a friend, I try to take a walk, I walk as far as I can walk cuz I love being out in the air, um the fresh sunlight, and it helps me think if I can if I can walk, if I’m feeling up to it. Um that helps me relieve stress as it relates to my disease”.
“I usually do a house cleansing for myself… you have to really be ready to let it go because it will physically cause you difficulties with the lupus if you do not try and get that stress off you. Keep your life as calm as possible.”
Cost as a barrier. Both participants expressed that cost was a concern when considering activities that work to reduce her stress, particularly as it relates to the cost of medications or activities that have proved to reduce or eliminate pain and other symptoms that cause stress:
“…one of the other things we were talking about where we said frustration, but the medications, the cost of the medications; the cost of the medications are so astronomical. I’m lucky I’m blessed that I have insurance and when I look at that number and I see what it would be without insurance, I go oh my gosh thank you goodness I’m thinking about people that don’t have insurance um and that bothers me. That bothers me cuz what if I don’t what if I am the one that’s underserved next month because of my lupus?”
“Lack of money…I definitely want to [join the Wellness Center] and I want to have access to the pool and everything but like $300…things you want to do you try to pay for but right now money seems to be my only obstacle.”
Esteem and Physical Appearance/Ability. The participants explained their diagnosis resulted in side effects from their lupus as well as medication. This change to their outward appearance affected their confidence around others, self-esteem, and create stress when in a social setting:
“And now I have to try harder to look decent to myself, it’s about me when I look in the mirror. I don’t care what you say.”
Providing Explanation. The participants discussed how verbalizing their pain level can create stress within their lives as pertaining to finances or friendships. Often, their integrity is questioned by others who are not fully aware of the physical toll of a lupus diagnosis. Furthermore, one participant explained the frustration and stress of attempting to explain the variant nature of her disease.
“You can’t call into work like you need to. You’re hurting so bad and you just have to make yourself, that’s if you can, make yourself get up and go ‘cus you don’t wanna get look at like Oh boy here you go, you’re not, you’re out of work again. Here she goes, she’s not coming to work again, What’s wrong with her? Something’s always wrong with her. That something always wrong with you type of umm stigma that you feel.”
“The most difficult aspects… the wolf characteristic where you hear the boy cries wolf cuz you fee okay one moment then you feel awful the next moment and it’s hard to explain to folks that oh my goodness now I can’t make it up the stairs or I can’t make it um as far as I thought we were going to be able to walk… something of that sort um very frustrating”
“My old friends were rushing me to be at a higher place and it hurted [sic] me because they weren’t allowing me to be sick or to be where I was until I was ready to move forward.”
Discussion
A predominant trend, interwoven throughout all responses, was the participants’ experience of pain. This demonstrated that this personal disease-mediated factor may play a larger role in patient decisions to engage in EBPP’s or not, in contrast to other characteristics of the target population in the proposed conceptual model (priorities, perceptions of need and/or benefit, awareness of EBPP’s, personality type, depression, hopelessness, social support, lack of trust, transportation, time, cost, and child or elder care), and may need to be a major component of outreach messages (i.e., future campaigns may want to focus on just how much these programs improve experiences of pain).
Findings can be used to increase and sustain the reach of EBPPs to people with lupus and improve tracking to assess effectiveness and ensure that lupus, including strategies to improve quality of life through EBPPs, are addressed. This process could forge relationships between healthcare providers, health promoting organizations, and academic researchers, and could generate approaches for arthritis, lupus, and other rheumatic conditions. Specific steps could include linkages among healthcare providers working with minority populations throughout the state of South Carolina to develop more targeted interventions aimed at assisting SLE patients with disease management.
Ethics Approval and Consent to Participate
This study was approved by the institutional review board (IRB) at the University of South Carolina (USC). The interviewer provided incentives and obtained oral informed consent at the time of the interview. Each interview was recorded with prior permission of participants.
Acknowledgements/ Funding
This work was supported by Grant No. 1 K01 AR060026-01
Authors’ Contributions
Conducted interviews: EMW. Conceived and designed the manuscript: EMW. Analyzed and summarized the data: EMW, TS, CV. Wrote the first draft of the manuscript: EMW. Contributed to the writing of the manuscript: TS, CV. Agree with manuscript results and conclusions: EMW, TS, CV. Jointly developed the structure and arguments for the paper: EMW, TS, CV. Made critical revisions and approved final version: EMW, CV, TS. All authors reviewed and approved of the final manuscript.
References
- Grossman J, Kalunian K (2002) Principles of therapy and local measures. In Dubois' lupus erythematosus, Wallace, Philadelphia.
- Cooper GS, Dooley MA, Treadwell EL, St Clair EW, Gilkeson GS (2002) Hormonal and reproductive risk factors for development of systemic lupus erythematosus: Results of a population-based, case-control study. Arthritis Rheum 46: 1830-1839.
- Alarcon G, Beasley T, Roseman J, McGwin G, Fessler B, et al. (2005) Ethnic disparities in health and disease: The need to account for ancestral admixture when estimating the genetic contribution to both (lumina xxvi). Lupus 14: 867-868.
- Oates JC, Levesque MC, Hobbs MR, Smith EG, Molano ID, et al. (2003) Nitric oxide synthase 2 promoter polymorphisms and systemic lupus erythematosus in african-americans. J Rheumatol 30: 60-67.
- Centers for Disease Control and Prevention (2015) Department of health and human services. Justification of estimates for appropriation committees.
- Rus V Hochberg M (2002) The innate immune system In Dubois' lupus erythematosus, Philadelphia.
- Peralta-Ramirez M, Jimenez-Alonso J, Godoy-Garcia J, Perez-Garcia M (2004) The effects of daily stress and stressful life events on the clinical symptomatology of patients with lupus erythematosus. Psychosom Med 66: 788-794.
- Birmingham D, Nagaraja H, Rovin B, Spetie L, Zhao Y, et al. (2006) Fluctuation in self-perceived stress and increased risk of flare in patients with lupus nephritis carrying the serotonin receptor 1a -1019 g allele. Arthritis Rheum 54: 3291-3299.
- Pawlak C, Witte T, Heiken H, Hundt M, Schubert J, et al. (2003) Flares in patients with systemic lupus erythematosus are associated with daily psychological stress. Psychotherapy and Psychosomatics 72: 159-165.
- Peralta-Ramirez M, Coin-Mejias M, Jimenez-Alonso J, Ortego-Centeno N, Callejas-Rubio J, et al. (2006) Stress as a predictor of cognitive functioning in lupus. Lupus 15: 858-864.
- Bricou O, Taieb O, Baubet T, Gal B, Guillevin J, et al. (2006) Stress and coping strategies in systemic lupus erythematosus: A review. Neuroimmunomodulation 13: 283-293.
- Greco C, Rudy T, Manzi S (2004) Effects of a stress-education program on psychological function, pain, and physical function of systemic lupus erythematosus patients: A randomized controlled trial Arthritis Rheum 51: 625-634.
- Lorig K, Lubeck D, Kraines R, Seleznick M, Holman H (1985) Outcomes of self-help education for patients with arthritis. Arthritis Rheum 28: 680-685.
- Lorig K, Ritter P, Laurent D, Fries J (2004) Long-term randomized controlled trials of tailored-print and small-group arthritis self-management interventions. Medical Care 42: 346-354.
- Lorig K, Ritter P, Laurent D, Plant, K (2008) The internet-based arthritis self-management program: A one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Rheum 59: 1009-1017.
- Austin J, Maisiak R, Macrine D, Heck L (1996) Health outcome improvements in patients with systemic lupus erythematosus using two telephone counseling interventions. Arthritis Care Res 9: 391-399.
- Carter R, Nunlee-Bland G, Callender C (2011) A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect Health Inf Manag.
- Fries J, Carey C, McShane D (1997) Patient education in arthritis: Randomized controlled trial of a mail-delivered program. J Rheumatol 24: 1378-1383.
- Gaab J, Sonderegger L, Scherrer S, Ehlert U (2006) Psychoneuroendocrine effects of cognitive-behavioral stress management in a naturalistic setting a randomized controlled trial. Psychoneuroendocrinology 31: 428-438.
- Goeppinger J, Arthur M, Baglioni A, Brunk S, Brunner C (1989) A reexamination of the effectiveness of self-care education for persons with arthritis. Arthritis Rheum 3: 706-716.
- Barlow J, Turner A, Wright C (2000) A randomized controlled study of the arthritis self-management program in the uk. Health Educ Res 15: 665-680.
- Bijlani R, Vempati R, Yadav R, Ray R, Gupta V, et al. (2005) A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med 11: 267-274.
- Brady T, Kruger J, Helmick C, Callahan L, Boutaugh M (2003) Intervention programs for arthritis and other rheumatic diseases. Health Educ Behav 30: 44-63.
- Derose S, Nakajiro R, Ziel F (2009) Automated messaging to improve compliance with diabetes test monitoring. The American Journal Of Managed Care 15: 425-431.
- Edworthy S, Dobkin P, Clarke A, Da Costa D, Dritsa M, et al. (2003) Group psychotherapy reduces illness intrusiveness in systemic lupus erythematosus. J Rheumatol 30: 1011-1016.
- Franklin V, Waller A, Pagliari C, Greene S (2006) A randomized controlled trial of sweet talk, a text-messaging system to support young people with diabetes. Diabetic Medicine 23: 1332-1338.
- Hanauer D, Wentzell K, Laffel N, Laffel L (2009) Computerized automated reminder diabetes system (cards): E-mail and sms cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther 11: 99-106.
- Juzang I, Fortune T, Blakc S, Wright E, Bull S (2011) A pilot programme using mobile phones for hiv prevention. J Telemed Telecare 17: 150-153.
- Lorig K, Ritter P, Plant K (2005) A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthritis Rheum 53: 950-957.
- Maisiak R, Austin J, West S, Heck L (1996) The effect of person-centered counseling on the psychological status of persons with systemic lupus erythematosus or rheumatoid arthritis: A randomized, controlled trial. Arthritis Care and Research 9: 60-66.
- O'Brien G, Lazebnik R (1998) Telephone call reminders and attendance in an adolescent clinic. Pediatrics 101: E6.
- Pena-Robichaux V, Kvedar J, Watson A (2010) Text messages as a reminder aid and educational tool in adults and adolescents with atopic dermatitis: A pilot study. Dermatol Res Pract.
- Bellg A (2003) Maintenance of health behavior change in preventive cardiology. Internalization and self-regulation of new behaviors. Behav Modif 27: 103-131.
- Kruger J, Helmick C, Callahan L, Haddix A (1998) Cost-effectiveness of the arthritis self-help course. Arch Intern Med 158: 1245-1249.
- Lorig K, Holman H (1993) Arthritis self-management studies: A twelve-year review. Health Education Quarterly 20: 17-28.
- Lorig K, Mazonson P, Holman H (1993) Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis Rheum 36: 439-446.
- Lorig K, Sobel D, Stewart A, Brown BW, Ritter P, et al. (1999) Evidence suggesting that a chronic disease self-management program can improve health status while reducing utilization and costs: A randomized trial. Medical Care 37: 5-14.
- Lorig K, Ritter P, Stewart A, Sobel D, Brown B, et al. (2001) Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care 39: 1217-1223.
- Lorig K, Sobel D, Ritter P, Laurent D, Hobbs M (2001) Effect of a self-managment program on patients with chronic disease. Effective Clinical Practice 4: 256-262.
- Israel B, Parker E, Rowe Z, Salvatore A, Minkler M, et al. (2005) Community-based participatory research: Lessons learned from the centers for children's environmental health and disease prevention research. EnvironHealth Perspect 113: 1463-1471.
- Israel B, Schulz A (2012) Methods in community-based participatory research. (2nd edn).; Jossey-Bass: San Franciso.
- Israel B, Schulz A, Parker E, Becker A (1998) Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health 19: 173-202.
- Minkler M (2005) Community-based research partnerships: Challenges and opportunities. J Urban Health 82: ii3-ii12.
Citation: Williams EM, Singleton T, Vrana C (2018) Understanding Quality of Life in African Americans with Lupus (UQAN) in South Carolina. J Community Med Health Educ 8: 620. DOI: 10.4172/2161-0711.1000620
Copyright: © 2018 Williams EM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4080
- [From(publication date): 0-2018 - Nov 19, 2025]
- Breakdown by view type
- HTML page views: 3194
- PDF downloads: 886