Understanding and Managing Sexual Disinhibition in Mentally Ill Clients
Received: 10-Jul-2018 / Accepted Date: 03-Oct-2018 / Published Date: 08-Oct-2018
Introduction
Mental illness and sexuality have high significance and connection. People diagnosed with serious mental disorders have a great impact on their sexuality. Either illness related, or developed because of medications as well [1]. It is observed in many psychiatric settings that clients admitted to psychiatric settings for treatment most of the time exhibit inappropriate sexual behavior within the initial hours of admission. Over familiarity and inappropriate sexual touching without consent is commonly observed [2]. Some people with mental illness have increase in sexual desire and need to fulfill the sexual urge more often. On the other hand, some clients experience decrease in sexual desire and have little or no feelings related to sexual relationships or desires [3]. Erotic or sexual desires are also verbalized by many clients as hallucinations. Which are pressured sexual behaviors on which they have no control [4].
Clients with serious mental illness and exhibiting inappropriate sexual behaviors are considered under sexual disinhibition. Sexuality is private and personal in many cultures, also it is a based on person’s choice and consent, disinhibition occurs when person don’t follow socio-cultural rules to express their feelings of sexual thoughts, impulses, and needs. This is mainly due to illness, procedures or medications [5]. Inappropriate sexual behaviors and Sexual disinhibition can include a sexual talk that includes foul or inappropriate language or sexual acts like touching, grabbing, masturbating or exposing [8]. It can be directed or in a disinhibited way like publically touching or rubbing the genitals, inappropriate and nonconsensual touching to acquaintance or strangers, commenting sexual jokes or sexual assault [6,8].
In both eastern and western context, sexuality is about rights and is related to privacy. It’s a personal matter which is decided by a person to whom he or she should marry or have sexual relationships or show love. Intimacy is completely personal and private there is no space of exhibiting it in public. Looking more intensely into eastern culture; public kissing, grabbing hand, or touching a spouse is even taboo. So, that can be highly imagined that how inappropriate it would be considered in terms of inappropriate sexual behaviors [7]. People don’t like to share their personal and private sexual thoughts in public. All these activities are kept in privacy. Neither a sexual comment nor a joke is appreciated nor any sexual foul communication that makes uncomfortable. On other hand people with sexual disinhibition and inappropriate sexual behavior can’t resist to keep their thoughts private. Many a times due to their illness they forget social norms and rules and practice inappropriate touching, commenting or grabbing [8].
Clients with dementia, schizophrenia, anxiety disorder or delusionary behaviors have commonly seen practicing Sexual disinhibition [4,9].
Observations
Clinically the authors have witnessed different situations; some of them are listed below.
• Homosexual behavior of a male client with other at the rehabilitation center.
• A young girl grabbing psychiatrist’ from back when he enters the ward.
• An adult male rubbing his genitals on the wall near the nursing station.
• Sharing with the shift nurse about sexual experiences with spouse during mental status examination.
• A young male entering the examination room periodically looking at the female nurse, smiling, showing inappropriate gestures and returning to the room.
• An adult female hides her face from the doctor and reports sexual desires relating to him while he visits.
• Exhibiting genitals to other clients and remain naked periodically. Coming out of the room without cloths.
• Naming nurses or doctors with some terms that are erotic and sexually inappropriate or asking about sexual preferences from nurses or doctors in the shift.
Strategic frame work helps nurses, doctors and therapist to take care of clients and manage their behaviors therapeutically [4,9].
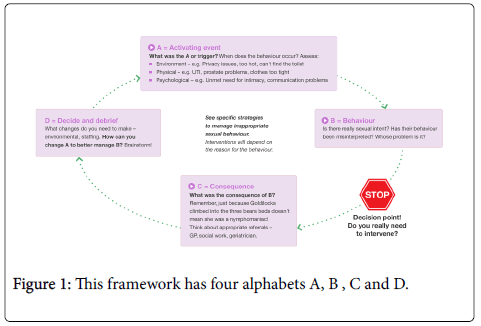
A is considered as activating event. There is a need of assessment that whether a triggering factor is environmental, physical or psychological. Environmental factor includes privacy issues, environmental stimulus like weather is too hot or access of toilet. Physical factors include wearing tight clothing or having prostrate problems. Psychological factors include need of intimacy or having communication problems (Figure 1).
B denotes behavior, which includes behavior shown by the patient. It can be verbal comment or physical touch to stranger. After this behavior, a therapist or staff needs to stop these actions and work on setting limits for the client.
C is for consequences just after the behavior. Nurses, therapist and care givers should confront patients about their behavior and its consequences, which can affect their relationship with others.
Last is D for decide and debrief that what were the triggering factors that induced this kind of behavior. Care givers should avoid triggering these behaviors after knowing the stimuli for the specific client.
Sexual needs are universal and everyone experience it. It doesn’t mean that as care givers we should not provide opportunity to clients so they can express their sexual desires. Divert them in arts, music, and ironing, washing etc. at the rehabilitation center or the hospital so that they can utilize their energies in other activities that are publically visible. Later, talk to them and discuss about their issues and provide them privacy in a separate and individual room so that they can work on their desires. Try to keep an eye on other clients who can be potentially victimized because of sexually disinhibited clients.
References
- Bardell A, Lau T, Fedoroff JP (2011) Inappropriate sexual behavior in a geriatric population. International Psychogeriatrics 23: 1182-1188.
- del Mar-Baños MM, Márquez-Hernández VV, Gutiérrez-Puertas L, Aguilera-Manrique G, Gutiérrez-Puertas V, et al. (2017) Sexual Behavior in Patients with Psychosis Admitted to a Hospital Unit. Issues in Mental Health Nursing 38: 473-479.
- Johnson C, Knight C, Alderman N (2006) Challenges associated with the definition and assessment of inappropriate sexual behaviour amongst individuals with an acquired neurological impairment. Brain Injury 20: 687-693.
- Bendigo Health (1999) Â Preventing and Managing Sexual Disinhibition or Inappropriate Sexual Behavior.
- Derouesnee C, Guigot J, Chermat V, Winchester M, Lacomblez L (1996) Sexual Behavioural Changes in Alzheimer's Disease. Alzheimer Disease and Associated Disorders.
- Global from Asia (2018) The Differences Between East And West In Terms Of Culture And Education.
- De Giorgi R, Series H (2016) Treatment of Inappropriate Sexual Behavior in Dementia. Current Treatment Options in Neurology, p: 41.
Citation: Soomar SM, Ali UU (2018) Understanding and Managing Sexual Disinhibition in Mentally Ill Clients. Psychol Psychiatry 1: 101.
Copyright: © 2018 Soomar SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 10055
- [From(publication date): 0-2017 - Sep 23, 2025]
- Breakdown by view type
- HTML page views: 9111
- PDF downloads: 944