Review Article Open Access
Uncomplicated Hydatid Cysts of the Liver: Clinical Presentation, Diagnosis and Treatment
Kazim Duman1*, Mustafa Girgin2 and Salih Hamcan3
1Department of General Surgery, Elazig Military Hospital, Elazig, Turkey
2Department of General Surgery, Faculty of Medicine, Firat University, Elazig, Turkey
3Department of Radiology, Gulhane Military Medical Academy, Ankara, Turkey
- *Corresponding Author:
- Kazim Duman, MD
Elazig Military Hospital, Department of General Surgery
Elazig, Turkey
Tel: 0538 385 9511
E-mail: drkduman@gmail.com
Received date: April 5, 2016; Accepted date: May 19, 2016; Published date: May 24, 2016
Citation: Duman K, Girgin M, Hamcan S (2016) Uncomplicated Hydatid Cysts of the Liver: Clinical Presentation, Diagnosis and Treatment. J Gastrointest Dig Syst 6:430. doi:10.4172/2161-069X.1000430
Copyright: © 2016 Duman K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Hydatid cyst of the liver is zoonosis caused by the larval stages of taeniid cestodes belonging to the genus Echinococcus and is still endemic in the South European regions, Asia, South America, North Africa, Australia, New Zealand and several Asian and European countries. The diagnosis of non complicated hydatid cyst of the liver depends on clinical suspicion. They appear in two ways as general (systemic) symptoms, and local symptoms based on the site and organ on which larva settles. While cysts sometimes recover spontaneously, more severe clinical presentations are observed in immunosuppressive individuals. Ultrasonography is the gold standard diagnostic tool and E. Granulosus antigen 5 (Ag5) and antigen B (Ag B) obtained from cyst fluid are used as a serologic diagnostic method in combination with the imaging method. The current treatment of hydatid cyst of the liver varies from surgical intervention to minimally invasive treatments (percutaneous drainage) or medical therapies. Surgery is still the best treatment tool. Percutaneous drainage and treatment of the cyst is a good option to surgery in selected cases. Multiple, superficial single cysts are the most suitable ones for surgical treatment. Also for complicated infected cysts pressing biliary tree and vital organs, surgery should be the first choice of treatment coming to mind. We believe that the laparoscopic approach should be safe to uncomplicated cysts. The purpose of our article is to provide a current review of clinical, diagnostic, and therapeutic features of hydrated cyst diseases.
Keywords
Hydatid cyst; Clinical features; Diagnosis; Treatment
Introduction
The causing agent of cystic echinococcosis or hydatid cyst disease of the liver is Echinococcus Granulosus (E. Granulosis) belonging to taeniidae family of cestoda class, with the height of 2-6 mm and the maximum width of 0.6 mm, consisting of 3-4 rings [1,2]. Based on their genetic structures and biological properties, six different types of E.granulosis (sheep, cattle, horse, camel, swine and deer) have been shown. Sheep type is the most common form in human infections [3,4].
There are two hosts in the life-cycle of the parasite. The first one is the “primary host” assessed as the last or definitive host, and the second one is the “intermediate host” in which the illness occurs. Adult forms are present in the intestines of primary host animals including cats, dogs, wolfs and foxes, and here, they only cause intestinal parasitosis but not organ disease. Adult parasite lives approximately for 5 months in dog intestines [5,6]. “Definitive hosts” spread millions of parasite eggs defecation. Sheep and other herbivorous animals becomes “intermediate host” for the parasite when they eat herbs contaminated with these eggs, or humans become “intermediate host” for the parasite when they eat fruits or vegetables contaminated with these eggs. Embryo (oncosphere) which comes out of the egg taken via gastrointestinal tract, adheres to intestinal wall with its hooks, then enters into circulation and reaches firstly to the liver. Thus, liver is the most common site of disease in humans with 60-70% rate. The second common organ is lung with 20-25% rate. Other than these sites, disease may occur via systemic circulation in another organ (spleen, kidney, bone, brain etc.) with 10% rate.
Embryo loses its scolex when it settles in an organ, and takes the cyst form consisting of cuticula (exocyst) and germinal membrane (endocyst). The cyst has sterile, clear fluid inside, and this cystic structure is wrapped with a fibrous capsule “pericyst”. When alive hydatid cysts are eaten by the last host dog, the infection chain is completed, and the life cycle returns to beginning [5,6]. Hepatic cystic echinococcosis is life-threatening disease because of their medical and economical impact and their wide geographical distribution. The purpose of our article is to provide a current review of clinical, diagnostic, and therapeutic features of hidatid cyst diseases.
Epidemiology
Infestation is common in geographical regions with continuous contact with domestic carnivorous animals and livestock animals like sheep. It is thought to come to Europe via dogs of whalers from Iceland [7]. South European regions, Asia, South America, North Africa, Australia and New Zealand are endemic areas [8]. The reason of high prevalence is the abundance of sheep, goat herds grown by the countries. It is sporadic in North America in areas except Alaska and Northwest Canada. It is endemic in Turkey, Mediterranean countries, Middle East, South America, New Zealand, and South Africa. In all European countries (excluding Ireland, Iceland and Denmark), the incidence is reported to be 1- 8/100,000, and the highest prevalence is seen in Mediterranean coastline [9]. China is one of the most important endemic areas for hydatid cyst with the incidence detected to be 8.7– 42/100,000 [10]. Tanzania, Malta, South Cyprus and New Zealand became hydatid cyst free zones with their applied public health policies [11].
In our country; the incidence is between 1/20,000 and 20/1,000,000, and the infection rates in dogs are in the range of 0.32%- 40% [6]. The incidence of the disease is increased in the territories where people make their living from livestock such as rural regions of East and Southeast Anatolia. Factors such as agriculture-based subsistence, low socio-economic status, regional climate, and uncontrolled and unhygienic animal slaughtering increase the incidence.
Clinical Features
They appear in two ways as general (systemic) symptoms, and local symptoms based on the site and organ on which larva settles. While cysts sometimes recover spontaneously, more severe clinical presentations are observed in immunosuppressive individuals.
Systemic signs and immunology; in early stages of cyst development, significant macrophage, neutrophil, eosinophil response are observed. Elevated levels of IgE, IgG2, and IgG4 are implicated for allergic reactions such as pruritus, hives, and anaphylactic shock [12]. Systemic findings deveolop as a result of complex antigenic organization via mutual down regulation of Th1 cytokines (Interferon- γ) and Th2 cytokines (IL-4, IL-5, IL-6) [13]. These reactions have been shown both in experimental studies and human trials [9]. These allergic reactions leading to anaphylaxis may also occur as a result of cyst rupture [14].
Local signs; A great majority of hydatid cyst patients have no complaint or sign. Cysts usually grow 1-5 mm in diameter every year, and the disease starts to cause symptoms a few years after the onset. Incidentally detected cysts have approximately 10-20 years of history. Symptoms develop slowly. Epigastric and/or right hypochondriac pain, nausea and vomiting are frequently observed. 85-90% of the cases have single organ involvement, and more than 70% of patients have a single cyst. Based on the organ in which the cyst settles and the environment they affect, they may show various clinical manifestations changing from cholangitis with biliary ruptures, portal hypertension, biliary obstruction and fistules, and ascites to abscess formation [15].
Diagnosis
At first, most clinicians does not consider this as it develops slowly without any pathognomonic signs, however factors such as visiting endemic areas within the last 10 years, prolonged contact with dogs in rural regions and insufficient personal hygiene, in the patient’s history will support the diagnosis. Diagnosis is made through a good combination of imaging studies and serologic tests. No disease-specific finding is observed in complete blood test and blood chemistry analyses. Transaminase elevation, bilirubin elevation and gamma glutamyl transferase elevation may be seen in liver cysts. In the Case of cyst rupture to bile ducts, increased alkaline phosphatase, hyperamylasemia and eosinophilia may be seen as well.
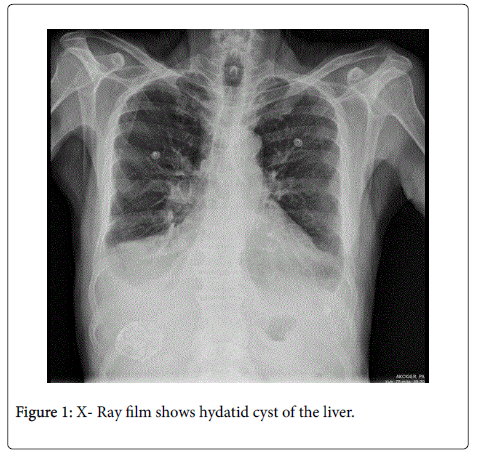
Direct X-ray films are not diagnostic for hydatid cyst, but may lead to the suspicion of disease (Figure 1). In case of complicated hydatid cyst, ‘air meniscus sign’ due to air passage between endo- and ectocyst may be seen in chest X-ray. Other signs that may be seen in direct Xray films include ‘water-lily sign’, ‘double-dome arch sign’ and ‘calcification’. Moreover, elevation in diaphragma may suggest hydatid cyst of the liver [16].
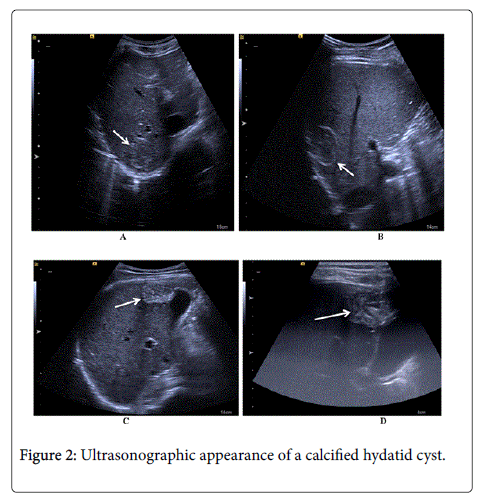
Abdominal Ultrasound (USG); It is the gold standard diagnostic method [15]. The contents and count of the cysts, the status of the adjacent organ, and vital status of cyst content can be identified. Ultrasonographic findings considered as pathognomonic for hydatid cyst are round or oval anechoic cyst presence with snow flake sign and clearly visible cyst walls, multiseptated cyst presence with cartwheel appearance, and multiseptated cyst presence with daughter vesicles (Figure 2). Gharbi classification based on the ultrasonographic appearance of the cyst was recently updated by World Health Organization - Informal Working Group on Echinococcosis (WHOIWGE) (Table 1) [17,18].
| Gharbi Classification | |
|---|---|
| Type | Explanations |
| I | Pure cystic |
| II | Cystic formation containing weathered membranes |
| III | Multiple septa / daughter cysts containing vesicles |
| IV | Hyperechoic heterogeneous solid mass appearance |
| V | Calcified thick- walled cysts |
| WHO- IWGE (*) Classification | |
| CL | Unilocular cystic lesion |
| CE1 | Unilocular anechoic cyst. Hydatid sand visible |
| CE2 | Multivesicular, multiseptated cyst |
| CE3a | Cyst containing a floating membrane due to detachment of the endocyst |
| CE3b | Cyst with a predominantly solid content due to membranes and few peripheral daughter cysts |
| CE4 | Degenerate cyst structure, no daughter vesicles |
| CE5 | Calcified thick-walled cysts. |
Table 1: Gharbi and WHO- IWG classification according to the ultrasonographic appearance of hydatid cyst [14,15].
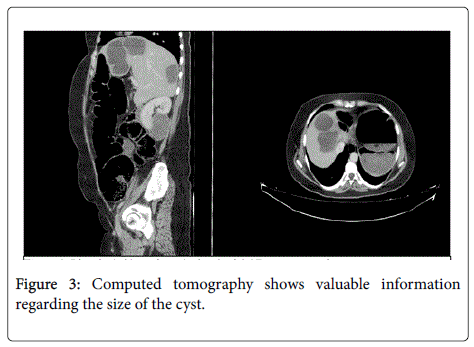
Ultrasonography may sometimes be insufficient for the differential diagnosis of the lesion seen in the images. In this case computerized tomography (CT) and magnetic resonance imaging (MRI) may be used. CT is an imaging technique which can detect cysts ≥ 1 cm, has the potential of assessing each organ and is very beneficial in the differential diagnosis. Diagnostic accuracy rates were reported to be between 61-96% in literature [19]. CT gives valuable information regarding the size of the cyst, septation presence, the integrity of germinative membrane, status of liver parenchyma, location and the depth of the cyst and adjacency with bile ducts (Figure-3). The presence of daughter cysts and exogenous cysts can also clearly be seen on CT [20]. Pathognomonic appearances are collapsed membrane and presence of daughter vesicles. Typical eggshell- like appearance is seen in completely calcified cysts. The size of the cyst can be estimated as well. CT is valuable when we considering surgical treatment, especially the laparoscopic method is to be used. Magnetic resonance imaging (MRI) ensures well structural details of the hydatid cysts. Although it might be helpful for demonstrating the lesion in the liver, it does not provide additional information in hepatic lesions and it is not costeffective when compared with either ultrasonography or CT [21,22]. MRI is especially indicated in cerebral pathologies.
Traditional immunodiagnostic tests (e.g. Casoni skin test, Complement fixation test) are not used today. Detection of E.Granulosus -specific antigen and immune complexes with ELISA is significant in more than 90% of the patients. E.Granulosus antigen 5 (Ag5) and antigen B (Ag B) obtained from cyst fluid are used as a serologic diagnostic method in combination with the imaging methods [23].
Detection of Echinococcus antibodies has 93.5% sensitivity and 89.7% specificity [24]. In some small hydatid cysts in cases where Echinococcus antibodies could not be detected, ultrasound-guided percutaneuous biopsies may be performed. However, in order to prevent secondary hydatid cyst formation when performing this procedure, Albendazole (oral) treatment must be initiated 4 days before the procedure, and must be continued for one month. In recent years, contrast-enhanced ultrasound (CEUS) is also used in these cases in which antibody could not be detected, to exclude malignancy [25].
Treatment
The aim of the treatment is to eliminate parasites, preventing recurrence and reducing morbidity and mortality. Size, site, count of the cyst, cohesion of experienced surgeon and radiologist seem to be the most prominent factors to reach this goal. The most suitable choice of medical treatment, surgical treatment (Open- Laparoscopic) and percutaneous radiological interventions should be administered for the most suitable patient.
Medical Treatment; Firstly, mebendazole and albendazole from benzimidazole carbamate group became available, and other members of the group were derived in time [26]. They cause degeneration in Echinococcus mitochondria and endoplasmic reticulum. In CE1- CE3a cysts smaller than 5 cm and in inoperable cases, medical treatment can be used as a combination of 10 mg/kg Albendazole, 40 mg/kg Mebendazole divided into 3 for 3 to 6 months to prevent recurrences after surgery. It is not recommended for use in calcified and inactive cysts.
In recent studies, Albendazole has been reported to be preferred more as it has higher gastrointestinal absorption and bioavailability [27]. The most common side effects are nausea, hepatotoxicity, neutropenia and alopecia. Medical treatment is not recommended in pregnant women, and in liver and bone marrow insufficiency.
Moreover Albendazole at daily 40 mg/kg dose combined with another chemotherapeutic praziquantel for 1 week has been shown to be more effective than Albendazole alone [28].
Percutaneous Interventions (PAIR = P: puncture, A: aspiration, I: injection, R: respiration); Suggested by Ben Amor in 1986, this technique is the first choice of treatment according to some authors [29]. However we recommend this more to repeating recurrences, and patients who are unwilling to undergo surgery. It is used in hydatid cyst cases smaller than 6 cm without cysto-biliary fistule. In bigger cysts, catheterization procedure described by Akhan et al. in 1993 is applied [30]. It should not be performed in undrainable, complicated, at-risk localized cysts with daughter vesicles, in children younger than 3 years old and in uncooperative patients [31].
The procedure is performed by entering into cyst with 19 gauge needle with USG guidance (P), care is advised, not to pour the contents of the cyst into the abdomen. Approximately half of the cyst volume is aspirated (A), and 20% serum saline in one-third of the cyst volume is injected in place of it (I), then after 20 minutes of waiting, the cyst is re-aspirated (R). In cysts bigger than 6 cm, catheterization is performed by placing 6-9 French pigtail catheters into cavity and leaving it there for drainage for a duration of 24 hours. In catheterization, the presence of any association between cyst and biliary tract is determined with cystography, alcohol in one-third of the cyst volume is injected into cavity, then after 20 minutes aspiration is performed, thus providing protoscolocidal/sclerotic effect [29,31].
In literature, the complication rate is 15% on average and recurrence rate is 1.5% [31]. Main complications are hives, hypotension, biliary rupture and infection.
Surgical Treatment; CE2- CE3b stage, multiple, superficial single cysts are the most suitable ones for surgical treatment. Also for complicated infected cysts pressing biliary tree and vital organs, surgery should be the first choice of treatment coming to mind. Two different methods of surgery can be used, namely radical and conservative procedures. Less recurrence is seen after radical procedures, however they present higher operative risks.
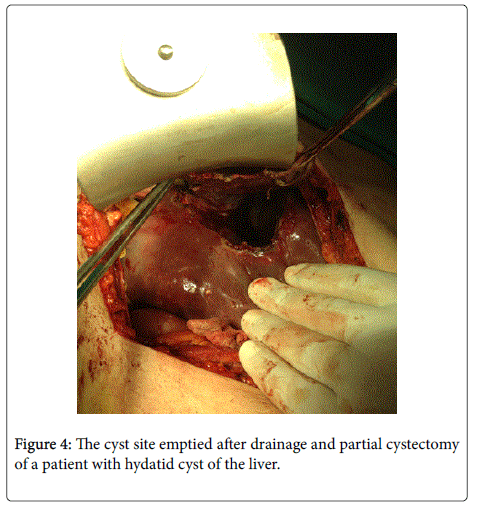
A. Conservative Procedures; Firstly, cyst content is aspirated with needle through the most curved site, then protoscolocidal agent is injected into the cyst through here, and kept there for 20 minutes. Most frequently, we use 20% Hypertonic Saline solution for this procedure. After 20 minutes, a window is opened through this aspiration site and cyst content taken out of abdomen with spoon. During this procedure, to prevent cyst content pouring into abdomen and to avoid anaphylaxis, it is important to cover the surrounding area of the window of cyst excision with gauze compresses impregnated with scolocidal agent. As protoscolocidal agent; Formalin, Glucose, Povidone Iodine, Silver nitrate, Cetrimide, Chlorhexidine can be used [32,33]. Most commonly used procedures may be listed as Partial Cystectomy with one of the procedures including drainage and/or omentoplasty, Capitonnage, Marsupialization, Myoplasty, and Rouxen- Y cystojejunostomy [29,31]. Figure-4 shows the cyst site emptied after drainage and partial cystectomy of a patient with hydatid cyst of the liver.
B. Radical procedures; They can be applied as Cystopericystectomy, hepatic resections, and liver transplantation [29,31].
In peripheral anterior located cysts (cysts not located profoundly and adjacent to vital organs), laparoscopic surgery can be performed with its all advantages. Manipulation is restricted, and during the operation, control of cyst content at first entry is limited. In literature, complication rate was reported to be 13% on an average and recurrence rate was reported to be in the range of 0-9%. So far longterm results are limited in literature [34,35].
Discussion and Conclusion
Advanced age, pregnancy, multiple cysts, comorbidity, and calcifiedinactive cysts are important considerations for treatment [23,35]. For medical treatment, Albendazole has been proven to be superior to other medical agents in randomized trials [36].
In literature, recurrences have been observed more frequently in patients undergone conservative procedure compared to the patients undergone radical surgery (24% vs . 3%), and the morbidity was detected to be higher (11% vs . 3%) [37]. Radical surgical procedures are better choices than conservative procedures (level of evidence of 2b and recommendation grade B) [35].
In many retrospective trials, complications such as infection and biliary fistule after external drainage are found to be observed more frequently compared to other conservative methods. Moreover, these complications were found to be lower after Omentoplasty (Level of evidence of 2b and recommendation grade B) [35,38].
In literature, complication rate of laparoscopic surgery was reported to be 13% on average and recurrence rate was reported to be in the range of 0-9%. Though long-term results remain to be limited in the literature so far, it was considered to be performed safely in selected cases (Level of evidence of 3 and recommendation grade C) [34,35].
In a meta-analysis performed by Smego et al., patients administered with Albendazole together with PAIR had lower morbidity and recurrence rates and shorter hospitalization periods compared to the patient’s undergone surgery [39]. While PAIR procedure is the first choice according to some authors, generally accepted opinion is that there is a need for more randomized trials.
Cystic diseases can be seen in other organs should be considered in the differential diagnosis of hidatid diseases. Due to hydatid cysts have germinal membrane with developed daughter vesicles whick have swimming protoscolex of fluids in many cases; It can be easily separated from other cystic diseases. However, the situation especially in early stage may force physicians. Hydatid cyst should be considered in the differential diagnosis of the following pathologies: Simple cysts, non-organize hematoma, necrotic tumor, cystic metastatic carcinoma, hemangioma, pyogenic abscesses, Amoeba abscess, Tuberculosis, fungal infections [40,41].
Finally, I would like to mention briefly the atypical located hydatid cysts and end this study. They are usually detected incidentally seen 10% amount of all. Especially in endemic areas when they are detected, they should be considered absolute favorites organs (liver, lung, brain) and, we must be examined, whole body scan should be performed. In 1965, Grassi classified atypical cases of hydatid cysts according to the incidence; Frequent group (kidney, spleen, bone and muscle), More rare group (brain, pancreas, diaphragm, thyroid gland, heart, breast, salivary gland, the pelvic area), At least the group (prostate, pituitary gland, adrenal gland, lymph node, peripheral nerves, orbit). Important feature of a typical installation; Vital organs sometimes losses (nephrectomy, splenectomy), is to amputations and even result in death [42-45].
References
- Eckert J, Conraths FJ, Tackmann K (2000) Echinococcosis: an emerging or re-emerging zoonosis? Int J Parasitol 30: 1283-1294.
- Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, et al. (2003) Hydatid disease from head to toe. Radiographics 23: 475-494.
- Chabane-Banaoues R, Oudni-M'radM, M'rad S, Mezhoud H, Babba H (2016) Environmental Contamination by Echinococcusgranulosussensulato Eggs in Relation to Slaughterhouses in Urban and Rural Areas in Tunisia. Korean J Parasitol 54:113-118.
- Thompson RC, McManus DP (2001) Aetiology: parasites and lifecycles. In: Eckert J, Gemmell M, Meslin FX, Pawlowski Z. WHOI/OIE manual on echinococcosis in humans and animals: a public health problem of global concern. Paris: World Organisation for Animal Health 1-19
- Carrim ZI, Murchison JT (2003) The prevalence of simple renal and hepatic cysts detected by spiral computed tomography. ClinRadiol58: 626-629
- Karaman U, Mman O, Kara M, Gicik Y, Aycan OM, et al. (2005) [Hydatid cyst prevalence in the region of Kars.]. TurkiyeParazitolDerg 29: 238-240.
- AgudeloHiguita NI, Brunetti E, McCloskey C (2016) Cystic Echinococcosis. J ClinMicrobiol 54: 518-523.
- CadavidRestrepo AM, Yang YR, McManus DP, Gray DJ, Giraudoux P, et. al. (2016) The landscape epidemiology of echinococcoses. Infect Dis Poverty 5:13.
- Lissandrin R, Tamarozzi F, Piccoli L, Tinelli C, De Silvestri A, et. al. (2016) Factors Influencing the Serological Response in Hepatic Echinococcusgranulosus Infection. Am J Trop Med Hyg 94:166-171.
- Chi P, Zhang W, Zhang Z, Hasyet M, Liu F, et. al. (1990) Cystic echinococcosis in the Xinjiang/Uygur Autonomous Region, People’s Republic of China. Demographic and epidemiologic data. Trop Med Parasitol 41: 157-162.
- Christofi G, Deplazes P, Christofi N, Tanner I, Economides P, et. al. (2002) Screening of dogs for Echinococcusgranulosuscoproantigen in a low endemic situation in Cyprus. Vet Parasitol 104: 299-306
- Zhang W, Li J, McManus DP (2003) Concepts in immunology and diagnosis of hydatid disease. ClinMicrobiol Rev 16: 18-36.
- McManus DP, Bryant C (1995) Biochemistry, physiology and molecular biology of Echinococcus. In: RCA Thompson and AJ Lymbery, editors. The biology of Echinococcus and hydatid disease. Wallingford: CAB International 355-410
- Atli M, Kama NA, Yuksek YN, Doganay M, Gozalan U, et al. (2001) Intrabiliary rupture of a hepatic hydatid cyst: associated clinical factors and proper management. Arch Surg 136: 1249-1255.
- Nunnari G, Pinzone MR, Gruttadauria S, Celesia BM, Madeddu G, et al. (2012) Hepatic echinococcosis: clinical and therapeutic aspects. World J Gastroenterol 18: 1448-1458.
- von Sinner WN (1997) Imaging of cystic echinococcosis. Acta Trop 67: 67-89.
- Brunetti E, Kern P, Vuitton DA; Writing Panel for the WHO-IWGE (2010) Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114: 1-16.
- WHO Informal Working Group. (2003) International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop 85: 253-261.
- Marrone G, Crino' F, Caruso S, Mamone G, Carollo V, et al. (2012) Multidisciplinary imaging of liver hydatidosis. World J Gastroenterol 18: 1438-1447.
- Nagarajan K, Sekar D, Babu JV, Kamath A (2013) Hydatid cyst of the liver causing inferior vena caval obstruction. J Assoc Physicians India 61: 671-673.
- HoÅÂ?ody-ZarÄÂ?ba J, ZarÄÂ?ba KP, KÄÂ?dra B (2013) Assessment of the accuracy of preoperative imaging methods in the diagnosis of hepatic single-chamber echinococcosis. Pol PrzeglChir 85:693-698.
- Dolay K, Akbulut S (2014) Role of endoscopic retrograde cholangiopancreatography in the management of hepatic hydatiddisease. World J Gastroenterol 20:15253-15261.
- Sayek I, Onat D (2001) Diagnosis and treatment of uncomplicated hydatid cyst of the liver. World J Surg 25: 21-27.
- Sbihi Y, Rmiqui A, Rodriguez-Cabezas MN, Orduña A, Rodriguez-Torres A, et al. (2001) Comparative sensitivity of six serological tests and diagnostic value of ELISA using purified antigen in hydatidosis. J Clin Lab Anal 15: 14-18.
- Lantinga MA, Gevers TJ, Drenth JP (2013) Evaluation of hepatic cystic lesions. World J Gastroenterol 19: 3543-3554.
- Chaia J, Menghebata WJ, Weia J, Deyua S, Bina L, et al. (2004) Observations on clinical efficacy of albendazole emulsion in 264 cases of hepatic cystic echinococcosis. Parasitology International 53:3-10
- Arif SH, Shams-Ul-Bari, Wani NA, Zargar SA, Wani MA, et al. (2008) Albendazole as an adjuvant to the standard surgical management of hydatid cyst liver. Int J Surg 6: 448-451.
- Cobo F, Yarnoz C, Sesma B, Fraile P, Aizcorbe M, et. al. (1998) Albendazole plus praziquantel versus albendazole alone as a pre-operative treatment in intra-abdominal hydatisosis caused by Echinococcusgranulosus. Trop Med Int Health 3: 462-466.
- Sayek I, Tirnaksiz MB, Dogan R (2004) Cystic Hydatid Disease: Current Trends in Diagnosis and Management. Surg Today 34: 987-996
- Akhan O, Dincer A, Gokoz A, Sayek I, Havlioglu S, et. al. (1993) Percutaneous treatment of abdominal hydatid cysts with hypertonic saline and alcohol. An experimental study in sheep. Invest Radiol 28: 121-127.
- Yagci G, Ustunsoz B, Kaymakcioglu N, Bozlar U, Gorgulu S, et. al. (2005) Results of Surgical, Laparoscopic, and Percutaneous Treatment for Hydatid Disease of the Liver: 10 Years’ Experience with 355 Patients. World J Surg 29: 1670-1679
- Topcu O, Sumer Z, Tuncer E, Aydin C, Koyuncu A (2009) Efficacy of chlorhexidinegluconate during surgery for hydatid cyst. World J Surg 33: 1274-1280.
- Dervenis C, Delis S, Avgerinos C, Madariaga J, Milicevic M (2005) Changing concepts in the management of liver hydatid disease. J GastrointestSurg 9: 869-877.
- Seven R, Berber E, Mercan S, Eminoglu L, Budak D (2000) Laparoscopic treatment of hepatic hydatid cysts. Surgery 128: 36-40.
- Gomez I Gavara C, López-Andújar R, Belda Ibáñez T, RamiaÁngel JM, MoyaHerraiz A (2015) Review of the treatment of liver hydatid cysts. World J Gastroenterol 21:124-131.
- Franchi C, Di Vico B, Teggi A (1999) Long-term evaluation of patients with hydatidosis treated with benzimidazolecarbamates. Clin Infect Dis 29: 304-309.
- Tagliacozzo S, Miccini M, Amore Bonapasta S, Gregori M, Tocchi A (2011) Surgical treatment of hydatid disease of the liver: 25 years of experience. Am J Surg 201: 797-804.
- Balik AA, BaÅÂ?oÄÂ?lu M, Celebi F, Oren D, Polat KY, et al. (1999) Surgical treatment of hydatid disease of the liver: review of 304 cases. Arch Surg 134: 166-169.
- Smego RA, Bhatti S, Khaliq AA, Beg MA (2003) Percutaneous aspiration-injection-reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: ametaanalysis. Clin Infect Dis 37: 1073-1083.
- Serbest S, Tiftikci U, Uludag A (2016) Unusual Localization of a Primary Hydatid Cyst: Scaphoid Bone: A Case Report. Medicine (Baltimore) 95: e3290.
- ÅÂ?ahin B, ÇomoÄÂ?lu ÅÂ?, Polat B, DeÄÂ?er K (2016) Hydatid cyst in unusual location: Pterygopalatine fossa-infratemporal fossa. AurisNasus Larynx 43: 464-467.
- Grassi G (1965) Contributoallo studio di alcunelocalizzazioni rare dele cisti da echinoccosis. GazzSanit9: 428-434.
- Calayan K, Celik A, Ko A, Kutluk AC, Altinli E, et al. (2010) Unusual locations of hydatid disease: diagnostic and surgical management of a case series. Surg Infect (Larchmt) 11: 349-353.
- Col C, Col M, Lafçi H (2003) Unusual localizations of hydatid disease. Acta Med Austriaca 30: 61-64.
- Granata A, Basile A, Bruno GA, Saita A, Falsaperla M, et al. (2011) A complex renal cyst: it is time to call the oncologist? Int J Nephrol 2011: 893985.
--
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 20857
- [From(publication date):
June-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 19715
- PDF downloads : 1142