Case Report Open Access
Ultrasound-guided Phrenic Nerve Block for Intractable Hiccups in Patients with Metastatic Colon Cancer: A Case Report
Tiffani D Pittman*, Andra DiStephano, Robert Chow and Ron SametDepartment of Anesthesia, Acute Pain and Regional Anesthesia at University of Maryland, Baltimore, MD, USA
- *Corresponding Author:
- Tiffani D Pittman
Department of Anesthesia
Acute Pain and Regional Anesthesia at University of Maryland, Baltimore
MD, 22 South Greene Street S11CO, Baltimore, MD, 21201
Tel: 301-405-1000
E-mail: tiffani.d.pittman@gmail.com
Received date: March 05, 2017; Accepted date: April 03, 2017; Published date: April 7, 2017
Citation: Pittman TD, DiStephano A, Chow R, Samet R (2017) Ultrasound-guided Phrenic Nerve Block for Intractable Hiccups in Patients with Metastatic Colon Cancer: A Case Report. J Palliat Care Med 7:302. doi: 10.4172/2165-7386.1000302
Copyright: © 2017 Pittman TD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Intractable hiccups can be a debilitating condition in cancer patients especially for those who have recently undergone thoracic or abdominal surgery and have tumor loads causing diaphragmatic irritation. The following case report details complete resolution of severe intractable hiccups due to an ultrasound guided phrenic nerve block in a patient with unresectable metastatic colon cancer. Ultrasound guided phrenic nerve block modification of the commonly performed interscalene brachial plexus may prove beneficial in relieving hiccups when medication therapy has failed or causes untoward side effects.
Keywords
Hiccups; Ultrasound guided; Phrenic nerve; Interscalene brachial plexus
Introduction
Hiccups are thought to be a result of an involuntary reflex arc that induces diaphragmatic spasm with contraction of the intercostal muscles immediately followed by closure of the glottis [1]. For most patients, hiccups are self-limited, lasting less than forty-eight hours. However, for those that suffer from persistent hiccups (lasting longer than 48 hours) and intractable hiccups (lasting longer than 2 months), the sequelae from the hiccups can be exhausting [2]. Patient suffering from these cases of debilitating hiccups can experience associated vomiting, decreased oral intake, dehydration, metabolic derangements, fatigue, sleep disturbances, depression and anxiety [2]. Additionally, patients that have undergone recent surgical procedures, the persistent and intractable hiccups can contribute to increased pain and wound dehiscence. The case presented is one in which an ultrasound-guided phrenic nerve block was performed for a patient with cancerassociated intractable hiccups.
Case Report
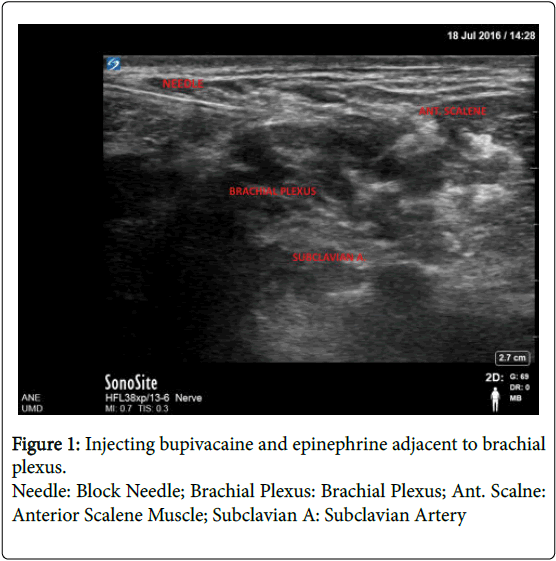
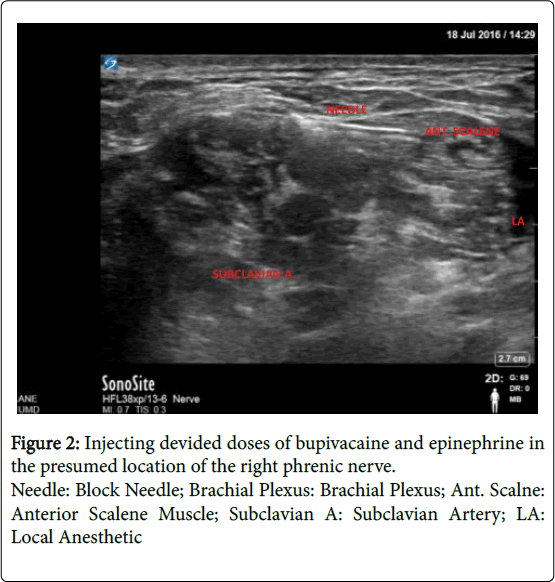
A 47-year-old male with a past medical history of hypertension, type 2 diabetes mellitus, and stage IV colon cancer with metastasis to the liver and peritoneum recently began suffering from intractable hiccups thought to be related to diaphragmatic irritation or invasion of his metastatic cancer. The patient initially presented to the pre-surgical admitting unit for scheduled colon cancer surgery and was to undergo an exploratory laparatomy with lysis of abdominal adhesions and administration of hyperthermic intraperitoneal chemotherapy (HIPEC). The regional anesthesia and acute pain medicine service placed a preoperative thoracic epidural for postoperative analgesia. Intra operatively, following abdominal exploration the surgeons aborted further interventions due to increased tumor burden and intra-abdominal adhesions. In perioperative discussions with the patient, he stated that the hiccups had become so burdensome that he was unable to eat, sleep restfully, or speak in complete sentences. In the past the patient was treated unsuccessfully with chlorpromazine, baclofen and haloperidol. During this hospital admission, the palliative care service was consulted for management of the patient’s intractable hiccups. Intravenous chlorpromazine 50 mg tid, intravenous metoclopramide 10 mg qid and gabapentin 300 mg tid was prescribed. Despite aggressive pharmacologic therapy for several days, the patient's hiccups persisted and were a source of significant discomfort. The regional and acute pain medicine service was re-consulted to evaluate the patient for a possible phrenic nerve block to treat the hiccups. We offered the patient an ultrasound-guided phrenic nerve block as a modification of our standard ultrasound guided interscalene brachial plexus blocks. We warned the patient that the procedure may not alleviate his hiccup symptoms and may induce motor and sensory blockade of the shoulder and arm. After informed consent, the decision was made to block the right side, given the known tumor burden in his liver and likely irritation or invasion of the right diaphragm. Standard ASA monitors were applied and ultrasound visualization using a Sonosite X-porte (Bothell, WA) of the right scalene muscles in short axis was performed. A 22 gauge Arrow (Morrisville, NC) block needle was inserted in-plane from lateral to medial and directed toward the interscalene fossa (Figure 1). Five milliliters of 0.0625% bupivacaine with 1:400,000 epinephrine was injected adjacent to the brachial plexus. The needle was then advanced anteromedially to the anterior scalene muscle and fifteen milliliters of the same solution was administered in divided doses in the presumed location of the right phrenic nerve (Figure 2). Within ten minutes, the patient’s hiccups resolved completely and after 30 minutes no signs of motor or sensory deficits in the right upper extremity were appreciated. Follow up approximately 2 months after the block was performed revealed no recurrence of hiccups.
Discussion
The etiology of hiccups in patients with advanced stages of cancer can be multifactorial [2]. These include direct injury or inflammation of the hiccup reflex arc, medication effect, metabolic derangements, as well as direct irritation of the diaphragm by the malignancy itself. Several medications have been proposed to treat persistent or intractable hiccups, however the FDA has only approved intravenous chlorpromazine as a successful line of treatment. Other medications that have been attempted include: metroclopramide, baclofen, tricyclic antidepressants, antiepileptics (valproic acid, carbamazipine and phenytoin), and nifedipine [3].
In the case presented above, the patient’s hiccups were thought to be secondary to irritation of the diaphragm from metastatic colon cancer. With no further surgical or chemotherapeutic interventions offered to decompress the tumor load, resolution of the hiccups would be extremely unlikely. After the patient did not respond to several days of multi-drug therapy, a phrenic nerve block was suggested with the hope of interrupting the hiccups reflex arc. This rationale is in accordance with evidence that suppression of the respiratory rhythmic cycle either with breath-holding, pharyngeal irritation or phrenic nerve anesthesia or transection can decrease the frequency and severity of hiccups or cure them indefinitely.
The phrenic nerve courses between the anterior scalene and sternocleidomastoid muscles, oblique to the jugular vein as it descends from the C3, C4 and C5 anterior rami. It is a thin nerve, and although ultrasound makes visualization of the brachial plexus standard practice, identifying the phrenic nerve is not always reliable [4]. It is common knowledge that when performing an interscalene block, the ipsilateral phrenic nerve is invariably also anesthetized, presumably due to spread of local anesthetic anteromedially to the anterior scalene muscle. We were thus able to easily obtain standard ultrasound views of the interscalene brachial plexus and modify the administration of the local anesthetic to target the phrenic nerve. A majority of local anesthetic was deposited in the space where the phrenic nerve is known to be located, anteromedial to the anterior scalene muscle, and the patient’s hiccups resolved. With infiltration of local anesthetic in this plane, there was concern that the patient would have some associated shoulder and upper arm weakness attributable to spread of local anesthetic to the brachial plexus. We chose to use a dilute concentration (0.0625% bupivacaine) of local anesthetic in hopes of avoiding arm and shoulder motor blockade. Other cases describing the use of interscalene approach for phrenic nerve block used concomitant nerve stimumation [5], or electromyography (EMG) and fluoroscopy [1] in efforts to target only the phrenic nerve. This case shows that a simple modification of the standard ultrasound guided interscalene brachial plexus block can result in effective phrenic nerve block and subsequent relief from hiccups without significant brachial plexus motor blockade.
Some additional questions remain. For example which side of the diaphragm to block? One must remain cautious to avoid bilateral phrenic nerve blockade, as even dilute concentrations of local anesthetic cannot guarantee safety from respiratory compromise. In our case, we chose to block the right phrenic nerve, given the known tumor involvement on that side. However, we don’t know if a left-sided block would have been equally effective. Similarly, we were unsure how long the relief from hiccups would last. Dilute concentrations of bupivacaine should not be expected to last much longer than 8-12 hours, however this patient remained free of hiccups for more than 2 months. Perhaps interruption of the repetitive reflex arc of hiccups for a short period of time provided lasting relief or made the pharmacologic therapy more effective. Regardless, given the low risk and side-effect profile, repeating the block at future intervals would not have been unreasonable if hiccups were to recur.
There is no gold standard treatment for persistent and intractable hiccups [5]. However, it seems prudent to pursue treatments options as hiccups can be debilitating for those who suffer from them. In patients with cancer suffering from hiccups multi-modal options including phrenic nerve blocks should be considered especially if there is poor or no response to established medication therapies. Many facilities may lack EMG and fluoroscopic capability and expertise, however ultrasound is now readily available in most settings. An ultrasoundguided phrenic nerve block as a modification of the commonly performed interscalene brachial plexus may prove beneficial in relieving hiccups when medication therapy has failed or causes untoward side effects.
References
- Young JS, Song DH, Kim JJ, Kim YD, Kim CK, et al. (2015) Recurrent intractable hiccups treated by cervical phrenic nerve block under electromyography: report of a case. Surg Today 45: 1446.
- Rizzo C, Vitale C, Montagnin M (2013) Management of Intractable hiccups: An Illustrative Case and Review. Am J HospPalliat Medicine 3: 2
- Howard R (1992) Persistent hiccups. BMJ 305: 1237.
- Okuda Y, Kamishima K, Aria T (2008) Combined use of ultrasound and nerve stimulation for phrenic nerve block. Can J Anesth55:3.
- Lier P, Felleiter P (2013) General Anesthesia or Phrenic Nerve Block for Treatment of Chronic Hiccups? AnesthAnalg 96:907-916.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 4449
- [From(publication date):
May-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 3597
- PDF downloads : 852