Case Report Open Access
Tuberculous Tenosynovitis Of The Wrist Joint: Imaging Findings On MRI
Naveen Rajadurai*Musculoskeletal Interventional Radiologist, Diagnostic Imaging Department, Hospital Sungai Buloh, Sungai Buloh, Selangor 47000, Malaysia
- Corresponding Author:
- Naveen Rajadurai
Musculoskeletal Interventional Radiologist,
Diagnostic Imaging Department, Hospital Sungai Buloh,
Sungai Buloh, Selangor 47000, Malaysia
Tel: +60361454333
E-mail: drnavraj@yahoo.com
Received Date: October 26, 2016; Accepted Date: November 21, 2016; Published Date: November 24, 2016
Citation: Rajadurai N (2016) Tuberculous Tenosynovitis Of The Wrist Joint: Imaging Findings On MRI. J Infect Dis Ther 4:307. doi: 10.4172/2332-0877.1000307
Copyright: © 2016 Rajadurai N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Tuberculosis of the musculoskeletal system is uncommon and presents in 10% of extrapulmonary tuberculosis. Although atypical presentation of TB includes spine (51%) pelvis (12%), hip and femur (10%), knee and tibia (10%), and ribs (7%), tuberculous infection of the wrist is rare. Tuberculosis still remains the primary cause of tendon sheath infection even though it is an uncommon site of extra-articular TB. Due to its delayed initial diagnosis and because it mimics many other disease processes, many complications arise secondary to tuberculous tenosynovitis. Median nerve compression leading to carpal tunnel syndrome may also occur in these patients. This report discusses the imaging findings on MRI of a patient who presented with wrist swelling and was confirmed to have tuberculosis of the wrist on histopathological examination.
Keywords
Tuberculous tenosynovitis; Wrist; Extra-articular tuberculosis; Extrapulmonary tuberculosis; MRI findings; Acid fast bacili
Introduction
Tuberculosis of the musculoskeletal system is uncommon and presents in 10% of extrapulmonary tuberculosis. Although atypical presentation of TB includes spine (51%) pelvis (12%), hip and femur (10%), knee and tibia (10%), and ribs (7%), tuberculous infection of the wrist is rare [1]. Tuberculosis still remains the primary cause of tendon sheath infection even though it is an uncommon site of extraarticular TB. Due to its delayed initial diagnosis and because it mimics many other disease processes, many complications arise secondary to tuberculous tenosynovitis. Median nerve compression leading to carpal tunnel syndrome may also occur in these patients. This report discusses the imaging findings on MRI of a patient who presented with wrist swelling and was confirmed to have tuberculosis of the wrist on histopathological examination.
Case Report
A 50-year-old Indian gentleman with a known history of noninsulin dependent diabetes mellitus, presented in 2011 with a history of a progressively painful wrist swelling over the past 6 months. The pain increased with time and was localized to the wrist. There was no history of trauma or fall. Synchronously, he also complained of productive cough over this 6 month period which was associated with significant weight loss of 10 kg over the same period. On physical examination, there was a tender swelling on the volar aspect of the right wrist which was warm, firm and associated with restricted movement of the wrist.
Laboratory investigations noted raised erythrocyte sedimentation rate of 102 mm/Hr and C-reactive protein of 74.56 mmol/L. Sputum was negative for acid fast bacilli. Mantoux test was inconclusive.
Plain radiograph of the right wrist showed erosion of the radiocarpal joints with a soft tissue swelling overlying the osteoporotic carpal bones. Chest radiograph revealed a biapical lung consolidation with cavitations on the left lung apex.
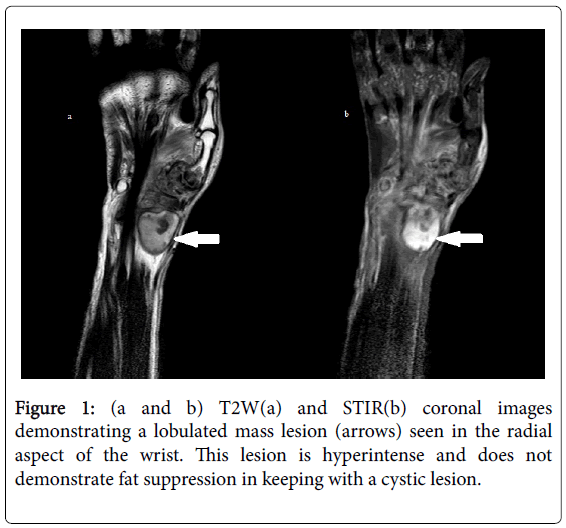
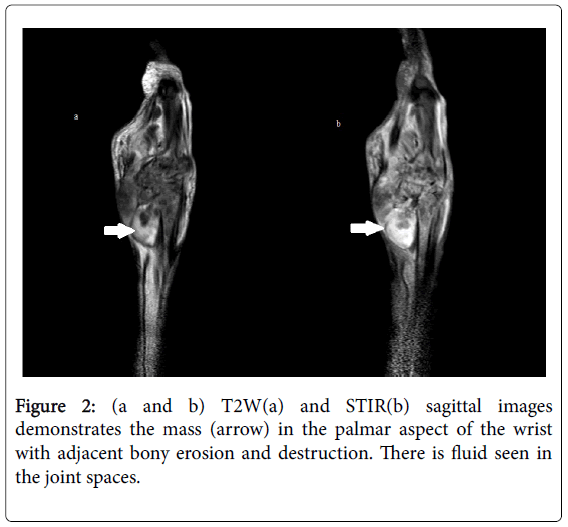
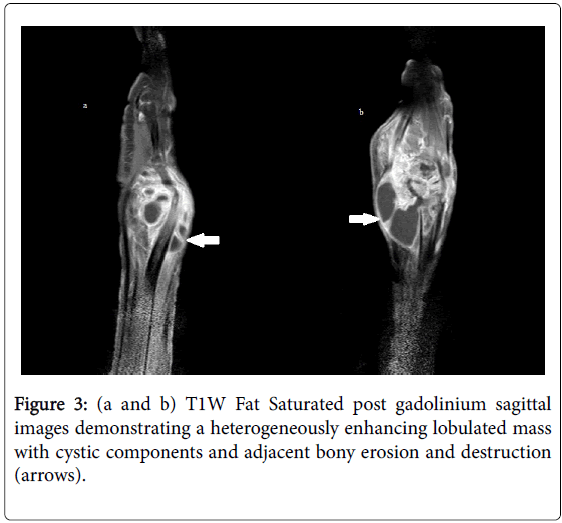
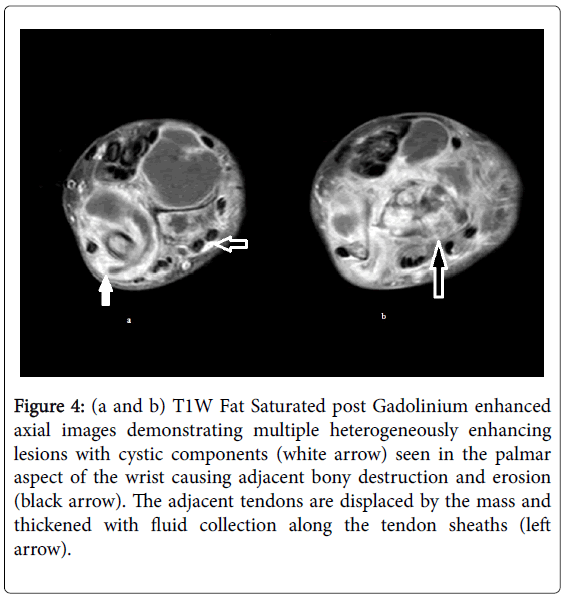
MRI of the right wrist was performed. This demonstrated heterogeneously enhancing lobulated masses, on T1-weighted axial images, occupying the right wrist involving the tendons, bones and joints with surrounding increased synovial fluid (Figure 1). There was underlying bony erosion and destruction (Figures 2 and 3) predominantly involving the carpal bones, carpo-metacarpal and radio-ulna-carpal joints. The tenosynovium was also thickened with fluid surrounding the extensor and flexor tendon sheaths. The accompanying median and ulnar nerves however, were intact (Figure 4).
Figure 4: (a and b) T1W Fat Saturated post Gadolinium enhanced axial images demonstrating multiple heterogeneously enhancing lesions with cystic components (white arrow) seen in the palmar aspect of the wrist causing adjacent bony destruction and erosion (black arrow). The adjacent tendons are displaced by the mass and thickened with fluid collection along the tendon sheaths (left arrow).
Surgery was performed under local anesthesia and an incision was made over the swelling followed by extensive drainage, widespread surgical debridement, irrigation and synovectomy. Fibrous tissue was seen attached to the extensor tendons. The margins of these tendons were debrided. Patient was then put on a below-elbow slab for 4 weeks. Two weeks later, patient was allowed intermittent mobilization and subsequently he recovered uneventfully.
Histopathological examination of the tissue revealed a lining of synovial epithelium. The excised tissue also demonstrated vascular proliferation, acute and chronic inflammatory infiltrates and fibrin deposits suggestive of granulomatous synovitis. Synovial fluid was positive for acid fast bacilli.
Patient was initiated on anti-tuberculous therapy of ethambutol, isoniazid, rifampicin and pyrazinamide for 2 months with monthly follow-up review. He was then planned for 10 months of rifampicin and isoniazid. During this time, he also went for regular physiotherapy.
On his last review, 6 months post-surgery, he was asymptomatic with improved range of movement of the right wrist.
Discussion
The primary mode of spread for tuberculosis is by inhalation of infected droplets, resulting in pulmonary disease. Approximately 1% to 3% of patients infected with tuberculosis demonstrate skeletal involvement, which most often manifests as spondylitis, peripheral arthritis, or osteomyelitis [2]. Approximately 50% of patients with musculoskeletal tuberculosis have concomitant pulmonary disease [2]. Being a rare complication, tuberculous tenosynovitis usually results from direct extension from adjacent bone or joint infection, although haematogenous spread from a distant primary focus is a recognized possibility [3].
Tuberculous tenosynovitis mainly targets the volar aspect of the hand and wrist [4]. Foot and ankle involvement are even more rarely reported. It is a slow progressive disease with silent symptoms leading to its late diagnosis. It is commonly misdiagnosed as a non-infectious tenosynovitis or tumour. The incidence of extrapulmonary mycobacterial infection has gradually increased over the past decade because of the increased number of immune-compromised individuals and drug-resistant bacterial strains [3]. Approximately one third of the patients with musculoskeletal tuberculosis have involvement of other viscera such as the lung [3].
There are three histological forms of tuberculous tenosynovitis with regards to its prolonged disease duration, resistance of the individual and microorganism varying virulence. Early on in the disease, there is replacement of the tendon by vascular granulation tissue followed by sheath obliteration by this fibrous tissue. There will be fluid restricted within the sheath and rice bodies may occur due to encasement. Finally, the tendon may consist of a few strands resulting in spontaneous rupture. If fibrous tissue healing fails to occur, extensive caseation and granulation will result in sinus formation and superimposed secondary infection [5].
Radiographic features of tuberculous infection of the wrist include bone erosion or cavitation, localized osteoporosis, gross destruction, and eventually joint ankylosis [6]. These findings are not specific and may deceptively mimic inflammatory arthritis, pigmented villonodular synovitis, gout, or a soft-tissue tumor.
There have been a few reported cases of MRI findings in tuberculous tenosynovitis of the wrist [6]. Prominent synovial thickening around the flexor tendons with fluid collection in the tendon sheath are a recognized MR finding [5,7]. The thickened tenosynovium and synovium usually present as low signal intensity on T1-weighted images. The characteristic hypointense synovium on T2- weighted images that is suggestive of granuloma is seen in approximately 40% of cases [8]. The synovial fluid usually demonstrates intermediate to low signal intensity on T1-weighted images and predominantly high signal intensity on T2- and T2*- weighted images [5,7]. The small low-signal foci or dots scattered in the synovial fluid on T2- and T2*-weighted images may refer to regions of tissue debris, caseous material, or rice bodies, as described in the literature [6,7]. In addition to tuberculous infection, rheumatoid arthritis and seronegative inflammatory arthritis may have a similar appearance and be associated with rice-body formation [2,8].
Post intravenous contrast administration of gadolinium diethylene triamine pentacetate (DTPA) revealed enhancement of the thickened tenosynovium and synovium. This enhancement may represent increased vascularity when tuberculous granulation tissue involves the synovium at the granulomatous stage. With regards to the enhanced thickened tenosynovium, contrast-enhanced MRI has been described to be particularly useful in differentiating the thickened tenosynovium from the fluid and the surrounding structures and in determining the extent of the lesion [8].
The differential diagnoses that needs to be considered in assessing the tuberculous joints and tenosynovitis of the wrist, include rheumatoid arthritis, juvenile rheumatoid arthritis, seronegative inflammatory arthritis, hemophilia, gout, pigmented villonodular synovitis, tumours originating from the synovium such as amyloidosis, synovial chondromatosis, and nontuberculous mycobacterial tenosynovitis such as Mycobacterium marinum infection [2,8]. All the above-mentioned differentials may exhibit similar MRI findings and need to be differentiated from tuberculous infection. On assessing T2- weighted images, a hypointense synovium along with central erosions, bone chips, and rim-enhancing abscesses may differentiate tuberculous arthritis from other types of monoarticular inflammatory arthritis (including rheumatoid arthritis) [8]. MRI appearance, such as T2 low-signal synovial thickening around the flexor and extensor tendons and synovial fluid collection that contains low-signal and nonenhanced foci in the tendon sheath, may aid us in reaching the proper diagnosis. However, surgical debridement of the thickened tenosynovium and laboratory investigations remain the gold standard in confirming the diagnosis at hand.
With regards to the treatment of this disease entity, the American Thoracic Society and Centres for Disease Control have advocated a 6 month regime of isoniazid and rifampicin with pyrazinamide included for the first 2 months, for both pulmonary and extra-pulmonary tuberculosis. A 9-month regimen is equally as effective. However musculoskeletal tuberculosis may necessitate longer duration of treatment as tuberculous tenosynovitis has a tendency for local recurrence, with more than 50% of cases recurring within a year of treatment necessitating close and longer follow up of patients.
Conclusion
Tuberculosis of the tendon sheath of the wrist is a rare entity. Due to its slow progression of disease and numerous differential diagnoses, delayed diagnosis is common resulting in complications. Early radical excision combined with anti-tuberculous multidrug therapy provides good functional results and prevents recurrence.
References
- Benkeddache Y, Gottesman H (1982) Skeletal tuberculosis of the wrist and hand: a study of 27 cases. J Hand Surg Am 7: 593 -600.
- Malaviya AN, Kotwal PP (2003) Arthritis associated with tuberculosis. Best Pract Res Clin Rheumatol 17: 319-343.
- Watts HG, Lifso RM (1996) Current concepts review: tuberculosis of bones and joints. J Bone Joint Surg Am 78: 288 -298.
- Fnini S, Ourab M, Rafai M, Cohen D, Largab A, et al. (1999) An uncommon occupational accident ; tuberculous tenosynovitis of the extensor of the hand. Chir Main 18: 309-312.
- Jaovisidiha S, Chen C, Ryu KN, Siriwongpairat P, PekananP, et al. (1996) Tuberculous tenosynovitis and bursitis: Imaging findings in 21 cases Radiology 201: 507-513.
- Martini M, Benkeddache Y, Medjani Y, Gottesman H (1986) Tuberculosis of the upper limb joints. Int Orthop 10: 17-23.
- Hoffman KL, Bergman AG, Hoffman DK, Harris DP (1996) Tuberculous tenosynovitis of the flexor tendons of the wrist: MR imaging with pathologic correlation. Skeletal Radiol 25:186 -188.
- Sawlani V, Chandra T, Mishra RN, Aggarwal A, Jain UK, et al. (2003) MRI features of tuberculosis of peripheral joints. Clin Radiol 58: 755-762.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 17500
- [From(publication date):
December-2016 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 16463
- PDF downloads : 1037