Tuberculous Spondylitis. Burden of Diagnosis. Case Presentation
Received: 31-May-2018 / Accepted Date: 19-Jun-2018 / Published Date: 25-Jun-2018 DOI: 10.4172/2332-0877.1000369
Abstract
Introduction: Tuberculosis continues to pose a problem of public health worldwide. Mycobacterium tuberculosis infects 1/3 of the world's population and seems to be responsible for 1.4 million deaths annually. In our country, the incidence is 6.5 times higher than in the EU countries. In 2016 there were 12836 cases of pulmonary TB (new and recurrent cases) of which 530 cases were TB MDR/XDR. The screening rate increased to 94% for new cases and 85% for MDR tuberculosis cases. Extrapulmonary tuberculosis remains a challenge by delaying of the diagnosis and the duration of treatment.
Case presentation: We present the case of a 73-year-old patient with no significant pathological history admitted to the National Institute for Infectious Diseases “Prof. Dr. Matei Bals”, Bucharest, in July 2017 (21 days) for myalgia and fever apparently after an episode of a respiratory tract infection. Due to myalgia, the occurrence of muscular atrophy and accelerate weight loss he referred to our hospital where was established the diagnosis of Tuberculous Spondylitis.
Results and methods: The diagnosis was established following numerous clinical and paraclinical investigations approximately 6 weeks after the first presentation to our hospital. As risk factors, the patient was diagnosed by the time of admission with other diseases that he wasn’t aware of as diabetes and renal impairment. Evolution under anti-tuberculosis treatment was arduous due to the development of hepatic toxicity, episodes of acute exacerbation of chronic renal disease and post-antibiotic diarrhoea. The final clinical and paraclinical outcome was favourable.
Discussion: Diagnosis of TB spondylitis requires both multidisciplinary collaborations and diagnosis experience. Anamnesis and understanding of symptoms are also important for proper selecting paraclinical tests panel. To understand these results in view of imposing a nephrotoxic and hepatotoxic treatment in the patient with pre-existing liver and kidney pathology, we returned to understanding the pathophysiology of Tuberculous Spondylitis.
Conclusions: Diagnosing the vertebral location of extrapulmonary tuberculosis requires understanding pathophysiology of this infection. Requesting of paraclinical investigation and performing differential diagnostics can help shorten the time required for diagnosis.
Keywords: Tuberculosis; Mycobacterium tuberculosis; Extrapulmonary tuberculosis; Musculoskeletal tuberculosis
Introduction
Tuberculosis continues to represent a worldwide public health issue both through morbidity and mortality, 1/3 of the population being affected with approximately 1.4 million deaths each year. Related to UE countries, in Romania, the incidence is 6.5 times higher. In 2016, there were 12836 cases of pulmonary TB (new and recurrent cases) of which 530 cases were TB MDR/XDR. The screening rate increased to 94% for new cases and 85% for MDR tuberculosis cases [1,2]. The fact that an official evidence of extrapulmonary TB cases is missing, represents a challenge both through diagnosis difficulty and underestimation.
The case that we are going to present is of a patient diagnosed with tuberculous spondylitis with non-specific onset which, in the beginning, has lead us on wrong pathways. There were necessary repeated hospital admissions, multiple investigations and multidisciplinary evaluations until final diagnosis was established. Extrapulmonary tuberculosis remains a challenge because of the delaying the diagnosis.
Vertebral localization represents 1/3 of the cases of musculoskeletal tuberculosis and is mainly due to BK (Koch Bacillus) hematogenous dissemination in the vertebral system, but also by contiguous or lymphatic dissemination of pleural tuberculosis. The primary site may be pulmonary or extrapulmonary (lymphatic, gastrointestinal, etc.). Tuberculous spondylitis is a subacute or chronic disease that can mimic a fungal or pyogenic infections, other granulomatous diseases or a neoplasia [1,3,4]. The most frequent localization is thoracic region, followed by the lumbar region and involves at least 2 adjacent vertebral bodies. Predisposing factors are: malnutrition, chronic ethanol consumption, diabetes, immunosuppressive treatments, chronic peritoneal dialysis, Tuberculosis history, etc. [1,3,5]. Chronic diseases of our patient discovered during hospital admissions represented the favoring factors and were the base of the challenges encountered during anti-tuberculous treatment.
Case Presentation
A 73-year-old patient, with chronic ethanolism and a history of HTA therapeutically neglected is hospitalized in National Institute for Infectious Diseases “Prof. Dr. Matei Bals”, Bucharest, during July 2017 being on the 21st day of the disease.
The onset was apparent in full state of health condition with fever (39°C) and myalgia. He was hospitalized for 7 days (23.06.2017-30.06.2017) in another hospital where he was diagnosed with Interstitial Pneumonia and received antiviral, antibiotic and steroid anti-inflammatory treatment with symptoms relief. After discharge, lower limb myalgia was accentuated with muscle atrophy and weight loss (about 8 Kg in 3 weeks). The patient was admitted in our hospital.
Materials and Methods
At first admission in our clinic (13.07.2017-21.07.2017) the patient was afebrile with average general condition, pale skin, purple lesions in the chilean region, atrophy of thigh and calf muscles and accused bilateral thighs myalgia with walking difficulty and sensitivity to lumbosacral spine percussion.
Blood tests have shown a significant inflammatory syndrome (ESR-102 mm/1 h, Fibrinogen-820 mg/dl, C reactive protein-115 mg/l), average normocytic normochromic anaemia (Hb-10.8 g/dl), neutrophilia, nitrogen retention syndrome (Creat-1.3 mg/dl, Urea-62 mg/dl), protein electrophoresis - nonspecific inflammation without monoclonal gammopathy, modified glycemic and glycosylated haemoglobin, Coombs direct and indirect negative test; no significant changes in urine test, hemocultures negative.
Pulmonary radiography (13.07.2017): accentuated hila with fibrous changes and calcification on the right side; pleural diaphragmatic adhesions to the right; right horizontal pleurisy. The patient had no history of pleural effusion.
Lumbosacral X-ray front+profile (14.07.2017): Lumbarisation of S1; inferior lumbar vertebrae discartrosis.
Abdominal ultrasound: Hyperrecogenic liver structure-the patient consumes almost daily alcohol.
Ophthalmic consultation and cardiac ultrasound excluded endocarditis.
Neurologic exam raises the suspicion of rheumatic polymyalgia: no muscle deficiency in the upper limbs, proximal limb motor deficit in the lower limbs with myalgia, no changes in sensitivity. EMG is recommended.
EMG (18.07.2017): lower limbs chronic moderate chronic sensorimotor polyneuropathy. Bilateral carpal tunnel syndrome. Without myopathy changes at this time.
Dexamethasone 8 mg/day treatment was started with clinically and biologically favorable outcome by improving the inflammatory syndrome (ESR-68 mm/1 h, Fibrinogen-734 mg/dl, C reactive protein -23.8 mg/l), anaemia with haemoglobin normalization but maintaining nitrogen retention syndrome. The patient received a recommendation to continue treatment with Medrol with decreasing doses from 16 mg/day.
Discharge diagnoses were: Rheumatic polymyalgia probably secondary to the viral episode; Lower limbs chronic moderate chronic sensorimotor polyneuropathy; Diabetes type II newly diagnosed without requiring treatment at this time; Chronic kidney disease; Normocytic normochromic anaemia; High blood pressure; Chronic ethanol consumption.
At 10 days after discharge, the patient presents again in our hospital for recurrence of myalgia with abnormal gait when decreasing the dose of Medrol to 8 mg/day. Physical examination was comparable to the first admission.
Blood test results: Inflammatory syndrome (Fibrinogen-501 mg/dl, ESR-98 mm/1 h, CRP-21.8 mg/l), anaemia (hemoglobin-11.2 g/dl), lymphopenia, accentuated nitrogen retention syndrome (2.3 mg/dl, urea-206 mg/dl), uric acid-12.2 mg/dl, lipase-1259 U/l reaction.
Rheumatology consult is performed. There is a suspicion of chronic renal disease acutisation because of therapeutically neglected gout.
Nephrology consult was requested and the patient was transferred after 3 days to Nephrology Hospital from 02.08.2017-09.08.2017 where he was diagnosed with Chronic Renal Disease, the most likely due to systemic atherosclerosis. Renal function improved under specific hydration and diuretic stimulation (maximum values: creatinine-7.88 mg/dl and urea-208 mg/dl). As myalgia have been accentuated and the patient accused left lumbosacral pain with irradiation on the left calf increased by mobilization, not unexplained by the vascular changes of the left limb, it is decided to perform a Lumbosacral MRI which detects: significant acute inflammatory changes at L4-L5 vertebral hemiplates; circumferential disc protrusion, discreet conflict with L4-L5 roots, interpreted as L4-L5 spondylodiscitis. The patient is re-transferred to our hospital.
During the third admission to INBI (09.08.2017-18.09.2017), the patient's biological re-evaluation identified an increasing anaemia (Hb-9.6 g/dl), maintenance of minimal lymphopenia, maintenance of inflammatory syndrome (CRP-42.8 mg/l), Quantiferon TB-Gold -negative.
The upper digestive endoscopy excludes a local cause of anaemia.
Following the MRI result and neurosurgical evaluation, it is decided to initiate the antibiotic treatment taking into account the etiological staphylococcal possibility (20%-84% of the cases of non-tuberculous spondylitis). The antibiotic treatment with Oxacillin iv (12 g/day)+Ciprofloxacin iv (800 mg/day)+Rifampicin (600 mg/day) was started.
The patient was scheduled for bone biopsy on 21.08.2017.
Lack of favourable evolution under antibiotic treatment for pyogenic etiology at 14 days determinates us to look forward and to reassess the case.
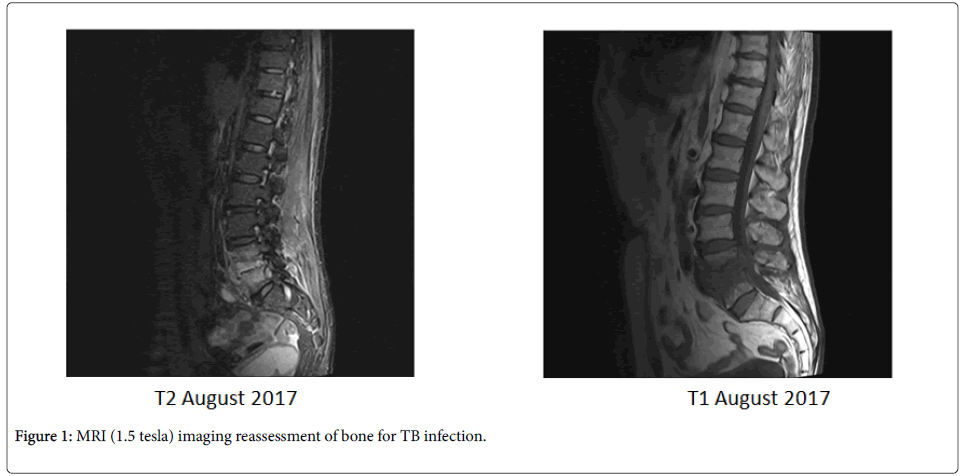
It was decided to perform an MRI (1.5 tesla) reassessment on 25.08.2017: important edema in the L4 and L5 vertebral bodies with the destruction of the vertebral plates. Diffuse edema with discreet subfascial collection and increased volume of straight paravertebral muscles (iliopsoas). The MRI aspect (damage to the vertebral plates, moderate intradiscal collection, and right paravertebral right muscle) indicates a TB infection rather than a pyogenic spondylitis.
The result of bone biopsy was received on 29.08.2017: dense connective tissue, adipose tissue fragment and small disk fragments with minimal lymphocytic infiltration, moderate interstitial fibrosis; in the peripheral side, small area with lipogranuloma appearance. Ziehl-Neelsen staining does not identify acid-alcohol resistant bacilli. BK-PCR from the bone fragment could not be performed (Figure 1).
A biopsy is performed from the achilles region cutaneous lesions-Kaposi's Sarcoma. HIV has been excluded from the first admission.
After re-evaluation of the case, it was decided to initiate anti-tuberculous treatment with Isoniazid-300 mg/day+Rifampicin-600 mg/day+Pyrazinamide-1500 mg/day+Etambutol-1200 mg/day (according to patient's weight). Evolution was initially favourable, but the patient develops diarrhoea, fever and general health alteration on day 10 of treatment.
Clostridium difficile stool tests were positive. Nitrogen retention increased (Creatinine-3.6 mg/dl, Urea-107.2 mg/dl), anaemia (Haemoglobin=7.9 g/dl) and inflammatory syndrome (CRP-346 mg/l). The anti-tuberculous treatment was discontinued and treatment with Vancomycin p.o and hydro-electrolytic rebalancing were initiated with improvement of digestive symptoms and biological test.
The anti-tuberculous treatment is restarted after 7 days while continuing to associate with Vancomycin p.o. Approximately 5 days after the anti-tuberculous treatment was reintroduced, the patient developed toxic hepatitis (ALT-358 U/l, AST-466 U/l, GGT-95 U/l) while renal function kept improving. Anti-tuberculous treatment was discontinued for approximately 14 days until the liver test became normal. The initial anti-tuberculous treatment was reintroduced with Rifampicin-600 mg/day, Etambutol-1200 mg/day and gradually increasing day by day Isoniaside doses from 100 mg/day to 300 mg/day with daily monitoring of liver tests. Last was introduced Pyrazinamide under which nitrate retention increased. It was decided that Pyrazinamide to be aborted and it was replaced with Moxifloxacine 400 mg/day.
Results
The patient is discharged after approximately 6 weeks with good overall status and Isoniazid, Rifampicin, Etambutol and Moxifloxacine regimen. The associated treatment was Amlodipine, Indapamid, Nebivolol, Milurit and Colchicine. It was recommended that the weekly liver, kidney tests and ECG to be performed with QTc monitoring due to treatment with Moxifloxacine.
Re-evaluation in INBI at one month: very good overall condition, inflammatory syndrome remitting with normal renal and hepatic function.
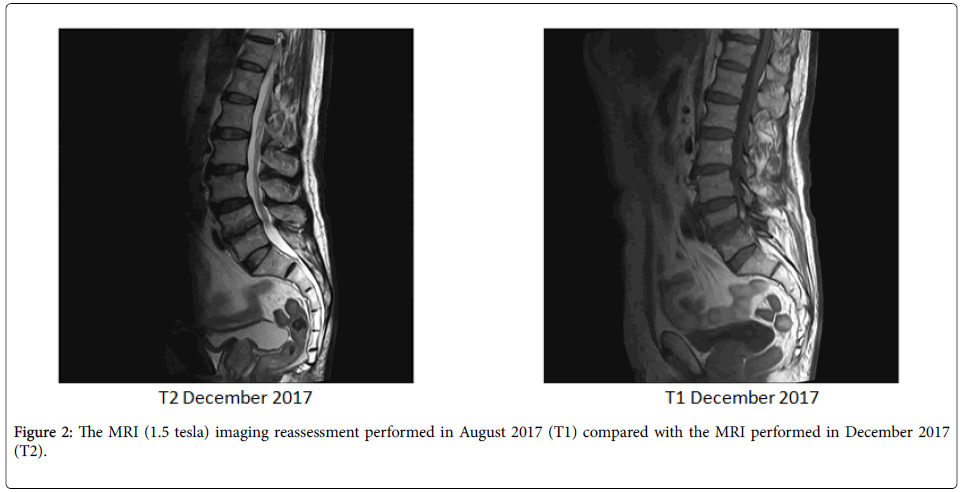
The MRI (1.5 tesla) imaging reassessment performed in August 2017 compared with the MRI performed in December 2017 (3 months after starting the anti-tuberculous treatment) revealed: the disappearance of T2 signal of L4-L5 paradiscal with volume reduction of the edematous-inflammatory changes in spinal vertebrae adjacent to the disc, which, after administration of contrast substance, captures palladium substratum. Epidural or paravertebral abscesses are not highlighted (Figure 2).
The volume of the L4-L5 disc hernia is reduced by maintaining a medial posterior disc protrusion, most likely by the disappearance of the edematous-infectious component. Keep tight L4-L5 canal stenosis. Conclusion: favourable imagistic evolution.
The treatment is continued with Isoniazid and Rifampicin with periodic reassessment of biological samples. MRI reassessment will be performed at 9 months to assess the duration of treatment (12 months or 18 months). It will be re-evaluated periodically for concomitant pathologies (kidney, heart, nutrition and diabetes).
Discussions
To understand these results in view of imposing a nephrotoxic and hepatotoxic treatment in the patient with pre-existing liver and kidney pathology, we returned to understanding the pathophysiology of TB spondylitis.
Tuberculous spondylitis is most commonly due to haematogenic dissemination in the vertebral system. Dissemination occurs via arterial or venous pathways [1,3,5]:
Anterior and posterior spinal artery of each subcondral vertebral region favors the dissemination in the paradiscal region.
Barton's paravertebral venous plexus is an avalvular system that allows free blood to flow in both directions based on intra-abdominal pressure or the chest cavity. Venous system is responsible for lesions in the center of the vertebral body.
Spinal TB initially involves the antero-inferior angle of the vertebral body adjacent to the terminal segment of the vertebral plate (best vascularized in the adult) then spreads to the center of the vertebral body or disc. The most common infection is located: paradiscal, anterior, central and neural arc region of the vertebral body. In the highlight of physiopathology of TB infection, ideally, the biopsy should have been performed from the antero-inferior region of the L4 vertebral body (according to MRI result of our patient). Even if biopsy has not been performed in the proper area, the lymphocyte infiltrate can support BK etiology. Although BK-PCR could not be performed, a negative result could not exclude the infection, as BK infection is known to be paucibacillary.
Spinal TB involves more than one vertebra because of vertebral artery bifurcation that leads to irrigation of two adjacent vertebrae. Bone scintigraphy (18.09.2017) revealed L4-L5 paravertebral collection, “mirror” erosions of the L4-L5 plates with the decrease of height of the vertebral bodies, a pathognomonic sign for tuberculous spondylitis.
Extension from the primary site of the vertebral body is supero-inferior and is done through the anterior or posterior spinal ligament to the vertebral plate of the inferior adjacent vertebra. The lack of proteolytic enzymes of BK, as opposite to pyogenic infections, makes possible the spread of infection in the subligamentous region. Edema in the vertebral body with the destruction of the vertebral plates and without damage of the intervertebral disc described in MRI sustains the theory. In pyogenic spondylodiscitis, the disc is destroyed by bacterial enzymes in a manner similar to the destruction of cartilage in septic arthritis. In over 97% of pyogenic infections, the disc is affected, unlike TB spondylitis where the disc is only affected in the late stages of the disease [2,3]. MRI shows damage of the vertebral plate and vertebral bodies, segments with better vascularization, and the absence of damage to the intervertebral disc since the disc becomes almost avascular in adults. BK has a high affinity for O2, such that, the initial affected segment should be well vascularized. In young patients, the vertebral disc is first involved because it is well vascularized. This is important for the proper selection of the biopsy area for TB spondylitis diagnosis, ideally, in the adult patient, the antero-inferior area of the upper vertebral body [3,5].
Kaposi Sarcoma active lesions along with lymphopenia and persistent anaemic syndrome represent immunodepression signs, respectively of chronic bacillary infection. A cellular immune response is required for controlling the BK infection. Co-stimulated cytokines released by macrophages (IL-1, TNF alpha, IL-6) activate T-CD4 cells which induce the production of IFN-γ. In latent TB, IFN-γ released from lymphocytes can be quantified by Quantiferon TB-Gold test. According to studies, in group aged 65 years or higher with tuberculosis, there are indeterminate results (33.3%) and false negative results (58.3%) [6], as well, steroid therapy leads to a high risk of indeterminate QuantiFERON test [7]. In our patient, the test was negative, but it cannot exclude the diagnosis. Also, in countries where the prevalence of primary infection is high, the interpretation of this test is difficult.
Diagnosis of TB spondylitis requires both multidisciplinary collaborations and diagnosis experience. Anamnesis and understanding of symptoms are also important. The patient declares alcohol consumption, the existence of rheumatism (gout) pathology, non-compliance with cardiologic and rheumatic therapy, only to the anamnestic data reassessment. The risk factors for our patient were mainly related to alcohol consumption, diabetes mellitus and possibly of chronic kidney disease. Understanding the indirect clinical and paraclinical changes, without the possibility of identifying BK in our case, led to late diagnosis in about 6 weeks after the patient was admitted in our hospital. The positive therapeutic trial also supported the diagnosis of TB spondylitis.
Case particularity
It is due to both difficulties of diagnosis and management of anti-tuberculous treatment in elderly patient with pre-existing renal, hepatic, rheumatic and cardiac pathology that develop post-antibiotic diarrhoea, toxic hepatitis and renal failure during post-treatment, resulting in therapy discontinuation which may lead in increasing risk of developing BK resistance to anti-tuberculous treatment.
Conclusions
Turberculous spondylitis remains a challenge through the difficulty of diagnosis. Understanding the pathophysiology of extrapulmonary BK infection is the basis for reducing the duration of diagnosis through targeted assessments.
Negative BK-PCR and negative Quantiferon TB-gold tests were not a diagnostic exclusion factors at our patient, MRI was essential for diagnosis.
The etiology of BK should not be underestimated and more doctors should be specialized in diagnosis and treatment especially of extrapulmonary tuberculosis where symptomatology can lead to multiple differential diagnoses.
References
- Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases 8th Edition.
- National Communicate (2016)-Pneumology Institute “Marius Nastaâ€.
- Rivas-Garcia A, Sarria-Estrada S, Torrents-Odin C, Casas-Gomila L, Franquet E (2013) Imaging findings of Pott’s diseases. Eur Spine J 22: 567-578.
- Safo S, Lieberman G (2009) Pott’s disease: A Radiological Review of Tuberculous Spondylitis. Harvard Medical School, Beth Israel Deaconess Medical Central.
- Ansari S, Amanullah MF, Ahmad K, Rauniyar RK (2013) Pott’s Spine: Diagnostic Imaging modalities and Technology Advancements. N Am J Med Sci 5: 404-411.
- Cho K, Cho E, Kwon S, Im S, Sohn I, et al. (2012) Factors Associated with Indeterminate and False Negative Results of QuantiFERON-TB Gold In-Tube Test in Active Tuberculosis. Tuberc Respir Dis (Seoul) 72: 416-425.
- Helwig U, Müller M, Hedderich J, Schreiber S (2012) Corticosteroids and immunosuppressive therapy influence the result of QuantiFERON TB Gold testing in inflammatory bowel disease patients. J Crohns Colitis 6: 419-424.
Citation: Caruntu FA, Barbu AE, Ciobotaru AC, Radu MN (2018) Tuberculous Spondylitis. Burden of Diagnosis. Case Presentation. J Infect Dis Ther 6: 369. DOI: 10.4172/2332-0877.1000369
Copyright: © 2018 Caruntu FA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3770
- [From(publication date): 0-2018 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 3077
- PDF downloads: 693