Trends and Treatment Outcome of Tuberculosis Patients in Assella Hospital from July 2011-June 2017, Oromia, Ethiopia, Seven Year Retrospective Study
Received: 20-Dec-2017 / Accepted Date: 17-Jan-2018 / Published Date: 23-Jan-2018
Abstract
Background: Tuberculosis (TB) is preventable and completely curable major public health problem in the world. Even though the number of TB death decreased by 22% in the past fifteen years it remains one of the top 10 causes of death and the leading cause from a single infectious agent, ranking above HIV/AIDS. It is the largest killer among communicable diseases in age group of 15 to 49years, when humans are most productive. Ethiopia is among the 22 high TB- burden and among the 27 high MDR-TB burden countries in the world with case detection and treatment outcome vary across regions.
Methods: A retrospective cohort study was conducted by reviewing medical record of tuberculosis patients who were treated in Assella hospital from July 2011 to June 2017. Descriptive statistics, both bivariate and multivariate logistic analysis was done using Stata statistical software. Odds ratio with 95% confidence intervals were calculated and P-value less than 0.05 was considered statistically significant.
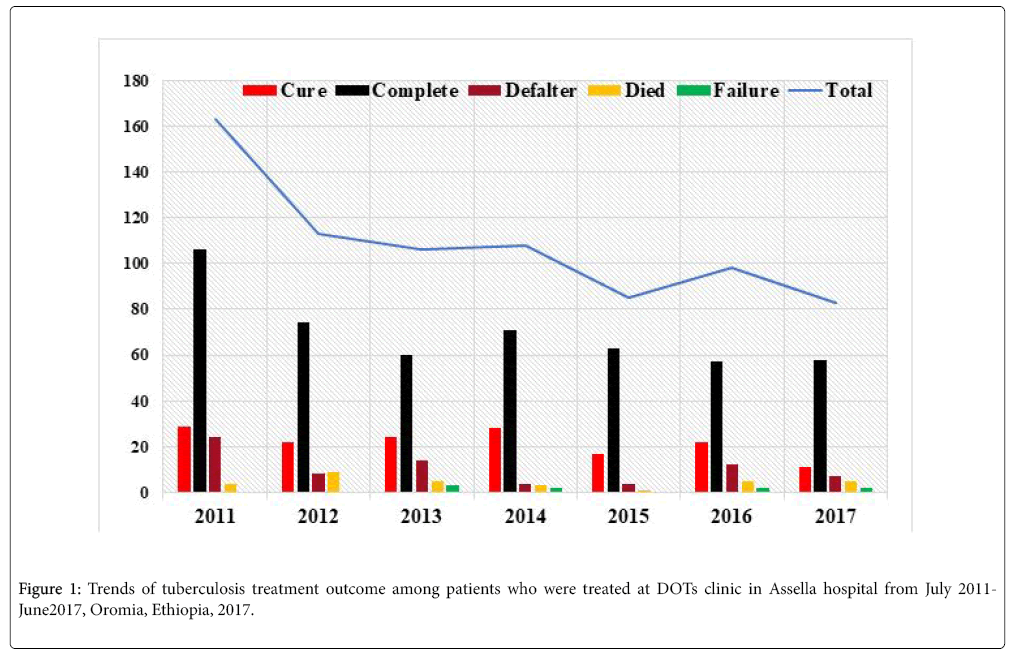
Results: A total of 756 patients were treated in Assella hospital of which 55.7% were male and 87% were from urban. About 60.4% were with age group 15-34 years mean age 30.5 ± 15.7. With some ups and downs the case notification rate decreases through time and the mean treatment success rate was 84.9% with defaulter, death and treatment failure rate of 9.7%, 4.2% and1.2% respectively. Almost all 92% of cases were identified through passive case detection after the patient present with clinical symptoms. Age, contact person, type of TB and year were identified as statistical significant factors for treatment outcome.
Conclusion: The mean treatment success rate was good but case detection rate was decrease trough time so the hospital needs to consider active case detection and improve defaulter tracing mechanism. Significant number of hospital staffs is being infected with TB so concerned health authorities including professionals need to give emphasis on the identified factors and on infection prevention control. Further study is recommended in retrospective design to include other predictors.
Keywords: Trends; Factors; Tuberculosis; Treatment outcome
Introduction
Tuberculosis (TB) is preventable and completely curable major public health problem in the world. Even though the number of TB death decreased by 22% in the past fifteen years it remains one of the top 10 causes of death and the leading cause from a single infectious agent, ranking above HIV/AIDS [1,2]. According to 2016 World Health organization (WHO) global TB report, it was estimated that 10.4 million TB cases of which 56% were men, 34% women and 10% children [3]. It is the cause 1.4 million deaths with additional 0.4 million deaths of TB among people living with HIV (PLWHIV) [3,4]. Tuberculosis is the largest killer among communicable diseases in age group of 15 to 49years, when humans are most productive and the leading cause of death among people living with HIV [2-5].
Currently, only two thirds of the global TB incident cases are notified to the national control programs and reported to WHO but with the existence of diagnostic and treatment gaps TB treatment averted 49 million deaths globally in the past fifteen years [3-5]. One of the agenda in the sustainable development goals is “End TB” Strategy with target of 95% reduction in TB deaths and 90% reduction in TB incidence but currently, the Region, and the whole world, is achieving only 1.5% to 2% annual decline in TB incidence [3]. With present efforts none of the countries in the region will reach the “End TB” targets by 2035 [2,4]. The highest share of the global TB burden nearly half 45.6% was observed in SEAR (South-East Asia Region) [2,6].
Over 95% of new tuberculosis cases and deaths occur in developing countries and WHO estimates that 80% of all TB cases are found in 22 high-burden countries (HBCs) and Ethiopia get the tenth rank in the world [6,7]. In addition, Ethiopia get the fifteenth rank among the 27 high MDR-TB burden countries which is defined as TB bacteria resistant to the most important first line TB drugs, isoniazid and rifampicin [6,8]. In Ethiopia TB kills about 32,000 people every year and treatment success rate was 89% in 2015 [8].
Tuberculosis is a serious infectious disease which can lead to disability and death so people with TB should be diagnosed and treated as early as possible to protect their own health and to prevent infection of people around them [5,9]. Passive case finding is usually practiced in our country that Health workers diagnose TB in people who present themselves to a healthcare facility after developing sign and symptoms of the disease [8,9].
A DOTs (Directly Observed Treatment Short Course) is a global Strategy launched by WHO in 1994 for prevention and control Tuberculosis [9]. The strategy has five key components of which the most important one is direct observation of treatment mean that health professionals must watch the patient taking each dose to ensure correct treatment and notice any problem rapidly to take action [5-7,9]. Prevention and control of TB depend on DOTs strategy, which is measured by case notification and treatment success rate developed by WHO and almost all countries had adopted the strategy, which have considerable progress towards global targets [5,9]. Ethiopia, adopt the strategy since 1992 as pilot in Oromia region at Arsi and Bale zones [9] and currently almost all public, private and non-governmental health facilities implement the strategy [7] but case detection and treatment outcome vary across different regions of Ethiopia [6,10-24]. So the result of this study will help other similar setting in developing countries to prevent and control the disease burden and achieve the sustainable development goal of end TB strategy by 2035 [3].
In spite of service provision with DOTs strategy in Assella teaching and referral Hospital, trend and treatment outcome of TB patients were not studied so far and this study is aim to show trends and identify factors associated with TB treatment outcome in the past seven years which helps to improve performance of DOTs services by availing useful evidence for different stakeholder’s work on disease prevention and control program [13].
Materials and Methods
Study setting and design
Assella hospital is one of the hospitals in Ethiopia found in Oromia regional state 125km far from Addis Ababa the capital city of Ethiopia. Currently the Hospital is within Arsi University and beside health care services provision the hospital involved in teaching of medical and other health science students. Facility based retrospective cohort study was conducted by collecting data with structured check list. Data of patients who were treated in the hospital from July 2011-June 2017 was collected by trained data collector.
Statistical analysis
The collected data was reviewed and checked for completeness and coded to enter into SPSS version 21 and exported to Stata version 12 for further cleaning and analysis. Descriptive statistics was done to describe findings. Initially bivariate binary logistic regression analysis was done then independent variables with P value less than 0.2 were considered as candidate for multivariate analysis and multivariate binary logistic regression analysis was estimated to identify predictors of TB treatment outcome. All the statistical tests were done at 5% level of significance and AOR along with 95% CI was reported. Confounders and interaction effect was checked by likelihood ratio test. The overall model goodness of fit was checked by Hosmer- Lemeshow and the prediction power by ROC (Receiver-Operating Characteristic).
Inclusion and exclusion criteria
Even though the hospital give service for diagnosis and referral for TB patients to the nearest health facilities including health centers in the town this study is on those patients who were treated in the hospital DOTs clinic since the study aim to see treatment outcome. Therefore, all types of TB cases which were treated from July 2011-June 2017 were included but patients who were transferred were excluded since information on treatment outcome was not available.
Ethics statements
To conduct this study Ethical clearance was obtained from institutional review board of Arsi University collage of health sciences. After getting permission from Medical director information was taken from DOTs clinic. Since the study was retrospective cohort patients consent was not obtained. However, patient information is handled secretly to maintain confidentiality and no unique identification was taken in the data base.
Diagnosis and treatment of tuberculosis
In Assella Hospital TB diagnosis is through routine sputum acid fasts staining, radiological and histological examinations but culture facilities were available. Patients who present with clinical symptoms of pulmonary Tuberculosis including cough lasting for two or more weeks, fever, and night sweat, shortness of breath and sputum production were examined through bacteriological analysis of two morning sputum samples by Zeihel-Nielsen staining, to see the presence of Acid fast bacilli (AFB). Then based on the national recommendation of smear result, clinical investigations and chest radiography results the physician decided to treat patients as TB case or not. Any person suspected of having extra-pulmonary TB (on the basis of clinical investigation, radiographic and histopathology findings or response to anti-TB treatment) were also treated as EPTB case. The risk management strategies in the hospital are so poor with low ventilation, minimum use of personal protective equipment’s which result to be infected.
Case definition
Case definition and treatment outcome were defined based on the standard definitions of the National Tuberculosis and leprosy control program (NTLCP) guideline of Ethiopia for the diagnosis and treatment of TB case [9].
Smear-positive pulmonary TB (PTB+): A patient with at least two initial sputum smear examinations positive for acid-fast bacilli (AFB) by direct microscopy, or one initial smear examination positive for AFB by direct microscopy and culture positive, or one initial smear examination positive for AFB by direct microscope and radiographic abnormalities consistent with active TB as determined by a clinician.
Smear-negative pulmonary TB (PTB−): A patient with symptoms suggestive of TB with at least three AFB negative sputum smear examinations, radiographic abnormalities consistent with active pulmonary TB, no response to a course of broad spectrum antibiotics and a decision by clinician to treat with a full course of anti-TB chemotherapy.
Extra pulmonary TB (EPTB): A patient has TB in organs other than the lungs, proven by one culture-positive specimen from an extrapulmonary site or histo-pathological evidence from a biopsy, or based on strong clinical evidence consistent with active EPTB and the decision by a physician to treat with a full course of anti-TB therapy.
Short course treatment regimen: Is given for two phases with first line fixed combination therapy. The intensive phase treatment lasts for two months with Ethambutol (E), Isoniazid (H), Rifampicin (R) and Pyrazinamide (Z) followed 4 months continuation phase with Isoniazid and Rifampicin since 2011.
Treatment outcome was evaluated according to NTLCP adopted from the WHO with the following categories.
Cured: Finishing treatment with negative bacteriology result at the end of treatment.
Treatment completed: Finishing treatment without bacteriology result at the end of treatment.
Failure: Remaining smear positive at 5th months despite correct intake of medication.
Defaulter: Patients who interrupted treatment for two consecutive months after registration. Default includes patients who have interrupted treatment and also patients who have died or transferred out and whose outcomes are unknown to the treatment staff.
Died: Patients who died from any cause during the course of treatment.
Transfer-out: Patients whose treatment results are unknown due to transfer to another health facility.
Successful treatment: A patient who was cured or completed treatment.
In line with WHO criteria, TB treatment outcomes were categorized in to:
Successful treatment outcome: If TB patients were cured (i.e., negative smear microscopy at the end of treatment and on at least one previous follow-up test) or treatment completed with resolution of symptoms.
Unsuccessful treatment outcome: If treatment of TB patients resulted in treatment failure (i.e., remaining smear positive after 5 months of treatment), default (i.e., patients who interrupted their treatment for two consecutive months or more after registration), or death.
Results
Socio-demographic and clinical characteristic
A total of 756 tuberculosis patients were treated in Assella hospital of which 421 (55.7%) were male and 658 (87%) were from urban setting. More than half 264 (60.4%) were within age group of 15-34years with mean age of 30.5 (SD ± 15.7). From the total 201 (26.6%) were PTB+, 249 (32.9%) PTB- and the rest 306 (40.5%) were EPTB cases. In the hospital all TB cases were tested for HIV and the co-infection rate was 153 (20.2%). When we see the seven-year treatment outcome the mean treatment success rate was 642 (84.9) whereas, 32 (4.2%) of cases were died, 73 (9.7%) defaulter and 9 (1.2%) were treatment failure (Table 1).
| Variables | Frequency (%) |
|---|---|
| Type of TB | |
| PTB+ | 201 (26.6) |
| PTB- | 249 (32.9) |
| EPTB | 306 (40.5) |
| Patient category | |
| New | 644 (85.2) |
| Transferred in | 35 (4.6) |
| Repeat | 24 (3.2) |
| Lost follow up | 4 (0.5) |
| Others | 49 (6.5) |
| HIV Sero-status | |
| Positive | 153 (20.2) |
| Negative | 603 (79.8) |
| ART started (n=153) | |
| Yes | 69 (45.1) |
| No | 84 (54.9) |
| MDR-TB screened (n=280) | |
| Yes | 38 (13.6) |
| No | 242 (86.4) |
| MDR Test Result (n=38) | |
| No Resistance | 22 (7.9) |
| RR | 9 (3.2) |
| MDR | 5 (1.8) |
| XDR | 2 (0.7) |
| Work place (n=280) | |
| Health facility | 19 (6.8) |
| Non-health facility | 261 (93.2) |
| Specific Profession (n=19) | |
| Medical students | 7 (36.8) |
| Other health professionals | 8 (42.1) |
| Cleaner | 1 (5.3) |
| Supportive staffs | 3 (15.8) |
| TB screening initiation (n=280) | |
| Self | 257 (91.8) |
| Referred | 17 (6.1) |
| Contact Screening | 6 (2.1) |
| Sex | |
| Male | 421 (55.7) |
| Female | 335 (44.3) |
| Residence | |
| Urban | 658 (87.0) |
| Rural | 98 (13.0) |
| Age Group | |
| 0-14 | 56 (7.4) |
| 15-24 | 268 (35.4) |
| 25-34 | 192 (24.5) |
| 35-44 | 94 (12.4) |
| 45-54 | 65 (8.6) |
| 55-64 | 43 (5.7) |
| >64 | 38 (5.0) |
| Base-line weight | |
| 0-7.9 | 8 (1.1) |
| 8-14.9 | 6 (0.8) |
| 15-19.9 | 17 (2.2) |
| 20-29.9 | 10 (1.3) |
| 30-39.9 | 66 (8.7) |
| 40-54.9 | 415 (54.9) |
| 55-70.9 | 214 (28.3) |
| > 71 | 20 (2.6) |
| Contact person | |
| Yes | 723 (95.6) |
| No | 33 (4.4) |
| Time of Registration | |
| July2010-June2011 | 163 (21.6) |
| July2011-June2012 | 113 (14.9) |
| July2012-June2013 | 106 (14.0) |
| July2013-June2014 | 108 (14.3) |
| July2014-June2015 | 85 (11.2) |
| July2015-June2016 | 98 (13.0) |
| July2016-June2017 | 83 (11.0) |
Table 1: Demographic and clinical characteristics of patients with tuberculosis treated in Assella referral and teaching hospital from July 2011- June 2017, Oromia, Ethiopia, 2017.
In Assella hospital notification of TB cases occurred in health facilities was started since July 2014 which is a good indicator for TB infection prevention and control. From the total 280 patients 19 (6.8%) were occurred in the hospital staff and when we see the specific professions of affected cases; 7 (36.8%) were medical students, 8 (42.1%) other health professionals, 1 (5.3%) cleaner and 3 (15.8%) supportive staffs. From the total 280 cases 38 patients were suspected and screened for MDR/TB and the test result shows that 22 (57.9%) with no resistance, 9 (23.7%) rifampicin resistance (RR) and 7 (18.4%) MDR cases (Table 2).
| Types of TB | TB treatment outcome | Total | P-value | ||||
|---|---|---|---|---|---|---|---|
| Successful | Unsuccessful | ||||||
| Cured (%) | Completed | Death | Defaulter | Failure | |||
| Pulmonary Positive | 153 (76.1) | 10 (5.0) | 9 (4.5) | 23 (11.4) | 6 (3.0) | 201 (26.6) | 0.001 |
| Pulmonary Negative | 0 | 210 (84.3) | 12 (4.8) | 24 (9.6) | 3 (1.2) | 249 (32.9) | |
| Extra-Pulmonary | 0 | 269 (87.9) | 11 (3.6) | 26 (8.5) | 0 | 306 (40.5) | |
| All types of TB | 153 (20.2) | 489 (64.7) | 32 (4.2) | 73 (9.7) | 9 (1.2) | 756 (100) | |
| 642 (84.9%) | 114 (15.1%) | ||||||
Table 2: Tuberculosis treatment outcome among all types of TB cases treated at DOTs clinic in Assella hospital from July 2011- June2017, Oromia, Ethiopia, 2017.
Trends and treatment outcome
With some ups and down the case notification rate in Assella hospital is decline through time this might be as a result of expansion of health facilities that implement the DOTs strategy so that most patients were referred to the nearest facility for treatment (Figure 1) with these trends of TB cases in the hospital it declines through time that yields to have decline treatment outcome (Figures 2-4).
Factors associated with TB treatment outcome
In multivariate binary logistic regression analysis having a contact person, patient age, and types of TB and treatment year were identified as factors for TB treatment outcome. Patients who did not have contact person were 3.8 times (AOR=3.76;95%CI:1.625-8.712) more likely to have unsuccessful treatment outcome than those patients who have had contact person. Types of tuberculosis was identified as a statistical significant factor for treatment outcome that patient with pulmonary negative were 34% [AOR=0.66; 95%CI: 0.3891.127] and with EPTB 44% [AOR=0.56; 95%CI: 0.334-0.953] less likely to have unsuccessful treatment outcome as compared with PTB+ patients. Patient with age ranges from 15-24 and 25-34 were 69% [AOR=0.31; 95CI:0.133-0.702] and 67% [AOR=0.33; 95%CI:0.141-0.786] less likely to have unsuccessful treatment outcome as compared with patient with age range from 0-14years old. Even though it is not statistically significant HIV positive patients were more likely to have unsuccessful treatment outcome than HIV negative patients (Table 3).
| Variables | Categories | Treatment Success | COR [95%CI] | AOR [95%CL] | |
|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||
| Sex | Male | 357 (55.6) | 64 (56.1) | 1 | |
| Female | 285 (44.4) | 50 (43.9) | 1.022 [0.684-1.526] | ||
| Residence | Urban | 559 (87.1) | 99 (86.8) | 1 | |
| Rural | 83 (12.9) | 15 (13.2) | 1.02 [0.566-1.841] | ||
| Age Group | 0-14 | 48 (7.5) | 8 (7.0) | 1 | 1 |
| 15-24 | 233 (36.3) | 35 (30.7) | 0.41 [0.147-1.141] | 0.43 [0.148-1.257] | |
| 25-34 | 167 (26.0) | 25 (21.9) | 0.37 [0.168-0.809] | 0.31 [0.133-0.702]* | |
| 35-44 | 76 (11.8) | 18 (15.8) | 0.370.162-832] | 0.33 [0.141-0.786]* | |
| 45-54 | 52 (8.1) | 13 (11.4) | 0.58 [0.244-1.386] | 0.58 [0.227-1.486] | |
| 55-64 | 39 (6.1) | 4 (3.5) | 0.61 [0.243-1.552] | 056 [0.210-1.471] | |
| >64 | 27 (4.2) | 11 (9.6) | 0.25 [0.072-0.874] | 0.24 [0.068-0.865] | |
| Contact person | Yes | 621 (96.7) | 102 (85.9) | 1 | 1 |
| No | 21 (3.3) | 12 (10.5) | 3.48 [1.661-7.288] | 3.76 [1.625-8.712]* | |
| HIV status | Positive | 128 (19.9) | 25 (21.9) | 1.13 [0.695-1.830] | 1.06 [0.621-1.821] |
| Negative | 514 (80.1) | 89 (78.1) | 1 | 1 | |
| Types of TB | P/positive | 163 (25.4) | 38 (33.3) | 1 | 1 |
| P/negative | 210 (32.7) | 39 (34.2) | 1.70 [1.036-2.774] | 0.66 [0.389-1.127] | |
| EPTB | 269 (41.9) | 37 (32.5) | 1.35 [0.832-2.192] | 0.56 [0.334-0.953]* | |
| TB category | New | 552 (86.0) | 92 (80.7) | 1 | |
| Repeat | 16 (2.5) | 8 (7.0) | 3.00 [1.248-7.210] | ||
| Lost follow up | 2 (0.3) | 2 (1.8) | 6.00 [0.835-43.125] | ||
| Transferred in | 29 (4.5) | 6 (5.3) | 1.24 [0.502-3.073] | ||
| Others | 43 (6.7) | 6 (5.3) | 0.84 [0.346-2.023] | ||
| Treatment year | July2010-June2011 | 135 (21.0) | 28 (24.6) | 1 | 1 |
| July2011-June2012 | 96 (15.0) | 17 (14.9) | 0.85 [0.443-1.647] | 0.84 [0.427-1.637] | |
| July2012-June2013 | 84 (13.1) | 22 (19.3) | 1.26 [0.678-2.350] | 1.25 [0.663-2.363] | |
| July2013-June2014 | 99 (15.4) | 9 (7.9) | 0.44 [0.198-0.970] | 0.39 [0.172-0.889]* | |
| July2014-June2015 | 80 (12.5) | 5 (4.4) | 0.30 [0.112-0.812] | 0.28 [0.103-0.770]* | |
| July2015-June2016 | 79 (12.3) | 19 (16.7) | 1.16 [0.608-2.211] | 0.80 [0.385-1.654] | |
| July2016-June2017 | 69 (10.7) | 14 (12.3) | 0.98 [0.484-1.978] | 0.85 [0.403-1.774] | |
| Base line Wt | 0-14.9kg | 11 (1.7) | 3 (2.6) | 2.46 [0.353-17.082] | |
| 15-19.9 kg | 16 (2.5) | 1 (0.9) | 0.56 [0.046-6.806] | ||
| 20-29.9 kg | 8 (1.2) | 2 (1.8)) | 2.25 [0.267-18.925] | ||
| 30-39.9 kg | 54 (8.4) | 12 (10.5) | 2.00 [0.408-9.799] | ||
| 40-54 kg | 354 (55.2) | 69 (60.5) | 1.75 [0.398-7.733] | ||
| 55-69.9 kg | 181 (28.2) | 25 (21.9) | 1.24 [0.272-5.681] | ||
| ≥ 70 kg | 18 (2.8) | 2 (1.8) | 1 | ||
Table 3: Socio demographic and clinical factors associated with TB treatment outcome of patients treated in Asellareferal and teaching hospital from July 2011-June 2017,Oromia, Ethiopia 2017.
Discussion
Demographic and clinical characteristics
Facility based retrospective study was conducted to identify factors associated with poor treatment outcome which is one of the major indicators for evaluation and performance of TB program. Globally, gender inequalities have been reported in TB case notification and TB is more common in males than females [1]. In this study 55.7% of patients were male which is in line with study in Tigray 54.3% [20] and Arsi zone 54.3 [11] but a beat lower than studies in Gambella 60.4% [14], Metema Hospital 60% [10], Mizan Aman General Hospital by Wegderese et al. 58% [19] and by Fiseha T et al. 57.4% [17]. The reason for this discrepancy might be due to higher proportion of males being exposed to the infection or underutilization of the DOTS service by females.
Tuberculosis is the largest killer among communicable diseases in age group of 15 to 49years, when humans are most productive [2-5]. In this study 72.3% of the study participants were with age range of 15–44 years and different studies conducted elsewhere support this evidence [21-23]. Since TB affects the most productive age group that might create challenges to the social and economic development of the community in the study area and as well to the nation at large. Majority of patients were diagnosed with EPTB 40.5% which is a bit higher than the first Ethiopian national population based TB prevalence survey 38.4% [23]. On contrary, PTB- was most prevalent in different studies; 51.1% by Wegderese et al. in southwest Ethiopia [19], 43.8% in Gambella hospital by Asebe G et al. [14], Gonder university 53.3% by Biruk M et al. [15], Metema by Jemal M et al. 55.4 [10] and Mizan Aman by Fiseha T et al. 52.3 [17].
In the study 20.2% and 64.7% of TB patients attending DOTs were cured and complete treatment, respectively which gives the overall treatment success rate of 84.9%, which is lower than the national target 89% [8], studies in North Ethiopia Tigray region 89% [20] and 95.6% in Southwest Ethiopia in Mizan-Aman general hospital by Wegderese et al. [19]. Meanwhile the treatment success rate is similar with 85.2% study conducted in Dilla university referral hospital [18] but finding is higher than other studies in Metema Hospital 65.3% [10], Gonder University by Biruk M et al. 60.1% [15] and Gambella hospital 70.8 [14].
The overall unsuccessful TB treatment outcome rate was 15.1%, with 9.7%, 4.2% and 1.2% default, death and treatment failure rates respectively which is higher than study in Tigray region [20] and southwest Ethiopia [19] but lower than other studies conducted in different parts of the world [10,14,15,21,22,24]. This discrepancy might be due to the difference in study time and period, sample size, study settings and variation at individual, community and health related factors that affect treatment outcome.
For unsuccessful TB treatment outcome defaulter rate accounts for majority of cases which is a bit lower than study in Ethiopia and Sudan with defaulter rate of 11.1% and 13.7% [18,25] but higher than other studies in different parts of our country [10,17,19]. The discrepancy might be follow up and defaulter tracing mechanisms difference between health facilities and in addition, this study consider patient as defaulter if their treatment outcome was not evaluated. During the study period 4.2% of TB patients were die which is almost similar with studies conducted in Metema, Gambella and Dilla [10,14,18] but higher than studies in southwest Ethiopia [17,19] On other hand the current death rate is lower than other studies conducted in different parts of the world; Malawi 5% [26], Uganda 36% [27]. The treatment failure rate in this study was 1.2% which is higher than studies in different parts of the world [10,14,18,19].
Factors associated with TB treatment out come
Even though different studies identified place of residence [11,18], sex [10,11,19,20], and TB categories [15,17] as factor for TB treatment outcome, this study fail to give statistical evidence. In this study as age increase the treatment outcome rate decreases and those patients with age group above 64 years old were lower treatment success rate than patients with age below 14 years. The lower treatment success rate among old patient could be associated with decreased immunity and associated co morbidities. Even if the result is not statistically significant HIV positive patients were more likely to have unsuccessful TB treatment outcomes than HIV negative patients and different studies identified HIV confection as factor for TB treatment outcome [3,10,14-17,20].
This study revealed that patients with PTB- and EPTB had lower treatment success rate as compared with patients with PTB+ which is in line with finding of studies in Ethiopia [15,18] but other study in Northwest Ethiopia revealed patients with PTB+ and PTB- were lower treatment success rate than EPTB [10]. This difference could be due high rate of HIV co-infection in these groups, which might decrease the treatment success by increase mortality and morbidity in addition, PTB+ patients are expected to strictly follow to complete their treatment.
This study identifies contact person as a statistical significant factor for TB treatment outcome and patients who have no contact person were more likely to have unsuccessful treatment outcome. Even though there is no study consider this variable as factor this might be as a result of close follow up, adherent to the treatment and easy to trace if the patient interrupts treatment. Other variable identified as factor for treatment outcome in this study was year with some ups and downs the overall treatment success rate was improved through time but it returned back in the last two years. Similarly, studies in Addis Ababa and in Southern Ethiopia and support this evidence [18,28].
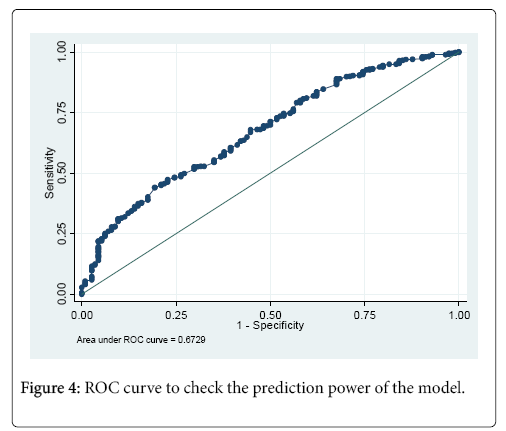
The overall goodness of the final model was checked by Hosmer- Lemeshow test to check model adequacy and the test statistic result was statistically insignificance (P-value= 0.1550) reveals that the model fit the data well and the actual observed values were statistically the same with the expected values. The prediction power of the model was checked by ROC and the area under the curve was 0.6729 which indicate the model having these predictors has good power to predict TB treatment outcome [29] (Figure 4).
Logistic model for RX_sucess_Rate_2, goodness-of-fit test
• Number of observations=756
• Number of covariate patterns=209
• Pearson chi2(192)=211.88
• Prob > chi2=0.1550
Logistic model for RX_sucess_Rate_2
• Number of observations=756
• Area under ROC curve=0.6729
Conclusion
The hospital implements the DOTs strategy as per the NTLCP and the mean treatment success rate during the study time was good. The study identifies; patients age, contact person, types of TB and time as statistical significant factors for TB treatment outcome. Higher rate of defaulter and treatment failure was observed so the hospital need to improve defaulter tracing mechanism and health professionals work on DOTs clinic need to take contact person for all patients. Most cases were identified through passive case detection therefore, the hospital need to consider active café finding with different strategies. Since the study was based on secondary data most important variables were not included so other study is recommended in community based survey and for the future the registration book need to be revised to include most important predictors based on evidences from different studies. Since significant numbers of cases were occurred in the hospital staffs concerned health authorities need to give emphasis and professionals who have direct contact with patient particularly with PTB+ need to consider infection prevention control mechanisms.
Acknowledgment
The author would like to acknowledge Arsi University, College of Health Science, Assella Hospitals, data collectors and study participants.
References
- WHO (2014) The End TB strategy, Global strategy and targets for tuberculosis prevention, care and control after 2015. Sixty seventh world Health Assembly. World Health Organisation, Geneva.
- WHO (2015) Global tuberculosis report. World Health Organisation, Geneva.
- WHO (2017) Bending the curve - ending TB: Annual report 2017. World Health Organisation, Geneva.
- WHO (2016) Global actions and investments fall far short of those needed to end the global TB epidemic. Global Tuberculosis Report 2016. World Health Organisation, Geneva.
- WHO (2009) Treatment of tuberculosis guidelines. World Health Organisation, Geneva.
- CDC (2017) Global HIV and TB activities in Ethiopia. Centre for Disease Control and Prevention, Ethioia.
- Federal Ministry of Health (2013) TB Research Advisory Committee(TRAC). Road map forTuberculosis Operational Research in Ethiopia. Addis Ababa, Ethiopia.
- Reves R, Angelo S (2016) As Ethiopia moves toward tuberculosis elimination, success requires higher investment.Center for Strategic and International Studies, US.
- Federal Ministry of Health Ethiopia (2008) Tuberculosis, leprosy and TB/HIV prevention and control programme.
- Jemal M, Tarekegne D, Atanaw T, Ebabu A, Endris M, et al. (2015) Treatment outcomes of tuberculosis patients in Metema Hospital, Northwest Ethiopia: A Four Years Retrospective Study. Mycobact Dis 5: 190.
- Hamusse SD, Demissie M, Lindtjorn B (2014) Trends in TB case notification over fifteen years: the case notification of 25 Districts of Arsi Zone of Oromia Regional State, Central Ethiopia. BMC Public Health 14:304.
- Dememew ZG, Habte D, Melese M, Hamusse SD, Nigussie G, et al. (2016) Trends in tuberculosis case notification and treatment outcomes after interventions in 10 zones of Ethiopia. Int J Tuberc Lung Dis 20: 1192–1198.
- Dangisso MH, Datiko DG, Lindtjørn B (2015) Trends of tuberculosis case notification and treatment outcomes in the Sidama Zone, Southern Ethiopia: Ten-year retrospective trend analysis in urban-rural settings. PLoS ONE 9: e114225.
- Asebe G, Dissasa H, Teklu T, Gebreegizeabhe G, Tafese K, et al. (2015) Treatment outcome of tuberculosis patients at Gambella Hospital, Southwest Ethiopia: Three-year retrospective study. J Infect Dis Ther 3: 211.
- Biruk M, Yimam B, Abrha H, Biruk S, Amdie F Z (2016) Treatment outcomes of tuberculosis and associated factors in an Ethiopian University Hospital. Adv Public Health 2016: 8504629.
- Jennifer HO, Fox GJ, Marais BJ (2016) Passive case finding for tuberculosis is not enough. Int J Mycobact 5: 374 -378.
- Fiseha T, Gebru T, Gutema H, Debela Y (2015) Trends of tuberculosis and treatment outcomes at MizanAman General Hospital, Southwest Ethiopia: A four year retrospective study. J Bioengineer & Biomedical Sci 5: 138.
- Gebrezgabiher G, Romha G, Ejeta E, Asebe G, Zemene E, et al. (2016) Treatment outcome of tuberculosis patients under directly observed treatment short course and factors affecting outcome in Southern Ethiopia:Afive-year retrospective study. PLoSONE11:e0150560.
- Wegderese S, Abera A, Gebru T, Fiseha T (2014) Trends of tuberculosis treatment outcomes at Mizan-Aman General Hospital, Southwest Ethiopia: A retrospective study. Int J Immunol 2: 15.
- Brehe G, Enqusilassie F, Assefa A (2012) Treatmnet outcome of smear-positive pulmonary tuberculosis patients in Tigray Region, Northern Ethiopia. BMC Public Health 12:537.
- Biadglegne F, Anagaw B. Debebe T, Anagaw B, Tesfaye W, et al. (2013) A retrospective study on the outcomes of tuberculosis treatment in FelegeHiwot Referral Hospital, Northwest Ethiopia. Int J Med MedSci 5: 85-91.
- Esmael A, Tsegaye G, Wubie M, Abera H, Endris M (2014) Treatment outcomes of tuberculosis patients in DebreMarkos referral hospital, North West Ethiopia (June 2008-August 2013): A five-year retrospective study. Int J Pharm Sci Res 5: 1500-1505.
- Federal Democratic Republic of Ethiopia Ministry of Health (2011) The First Ethiopian National Population Based Tuberculosis Prevalence Survey. Ethiopian Health and Nutrtion Research Institute, Addis Ababa.
- Tessema B, Muche A, Bekele A, Reissig D, Emmrich F, et al. (2009) Treatment outcome of tuberculosis patients at Gondar University Teaching Hospital, Northwest Ethiopia. A five-year retrospective study. BMC Public Health 9: 371.
- Elbssir K, Ali FF, Nasir SN, Rayyan AA (2016) Assessment Of treatment outcome of patients with tuberculosis, at treatment centers in Khartoum Locality Sudan 2015. Eur J Pharma Med Res 3: 73-75.
- Tweya H, Feldacker C, Phiri S, Smith AB, Fenner L, et al. (2013) Comparison of treatment outcomes of new smearpositive pulmonary tuberculosis patients by HIV and antiretroviral status in a TB/HIV clinic, Malawi. PLoS ONE 8: e56248.
- Kirenga BJ, Levin J, Ayakaka I, Worodria W, Reilly N, et al. (2014) Treatment outcomes of new tuberculosis patients hospitalized in Kampala, Uganda: A prospective cohort study. PLoS ONE 9: e90614.
- Getahun B, Amenia G, Medhina G, Biadgilign S (2012) Treatment outcome of tuberculosis patients under directly observed treatment in Addis Ababa, Ethiopia. Braz J Infect Dis 17:521–528.
- David W Hosmer, Stanley Lemeshow (2000) Applied logistic regression. Wiley series in Probability and Statistics, US.
Citation: Fisseha HZ (2018) Trends and Treatment Outcome of Tuberculosis Patients in Assella Hospital from July 2011-June 2017, Oromia, Ethiopia, Seven Year Retrospective Study. J Tuberc Ther 3: 112.
Copyright: © 2018 Fisseha HZ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 3647
- [From(publication date): 0-2018 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 2955
- PDF downloads: 692