Case Report Open Access
Treatment of Afferent Loop Obstruction by Percutaneous Trans-Hepatic Biliary and Intestinal Drainage
Jun Tie1,2*, Zhao Yiming2, Liu Jiangtao2 and Liu Yingdi2
1Xijing Hospital of Digestive Diseases, Xijing Hospital, Fourth Military Medical University, Xi'an, Shaanxi, 710032, China
2Department of Gastroenterology, Hai Nan Branch of Chinese PLA General Hospital, Sanya, Hainan, 572000, China
- *Corresponding Author:
- Jun Tie
Xijing Hospital of Digestive Diseases
Xijing Hospital, Fourth Military Medical University
Xi'an, Shaanxi, 710032, China
Tel: 86 18629507963
E-mail: tiejun7776@163.com
Received date: February 06, 2015; Accepted date: February 25, 2015; Published date: March 05, 2015
Citation: Tie J, Zhao Yiming Z, Jiangtao L, Yingdi L (2015) Treatment of Afferent Loop Obstruction by Percutaneous Trans-Hepatic Biliary and Intestinal Drainage. J Palliat Care Med 5:213. doi: 10.4172/2165-7386.1000213
Copyright: © 2015 Tie J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
We presented a rare case of chronic afferent loop obstruction after radical resection of gastric carcinoma. A 44- year-old man was admitted because of “upper abdominal distension and abdominal pain for 3 months, skin and sclera jaundice for 2 weeks”. Abdominal CT revealed dilatation of the intrahepatic bile duct and common bile duct, a large, abdominal cystic lesion, as well as left adrenal gland metastasis. MRCP revealed that the cystic lesion was an expansion of loops. Thus, the diagnosis of afferent loop (A-loop) obstruction was made. Subsequently, the patient underwent percutaneous transhepatic cholangial drainage (PTCD). The patient’s abdominal pain was significantly reduced, and the jaundice subsided. We should consider the possibility of the occurrence of the left adrenal metastasis and abdominal lymph node metastasis led to a chronic obstruction of A-loop. The chronic obstruction gradually developed into a complete blockage, further causing biliary obstruction and resulting in the occurrence of severe jaundice and abdominal pain. Here we not only reported a case of chronic afferent loop obstruction following radical resection of gastric carcinoma, but also analyzed the characteristic features of CT imaging and treatment. This case report is a good reference to similar gastrointestinal malignancy.
Keywords
Percutaneous trans hepatic cholangial drainage; Afferent loop obstruction
Case Report
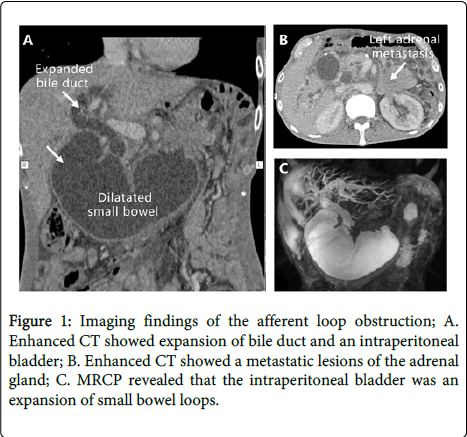
A 44-year-old man presented with 1-month progressive jaundice, as well as 3-month upper abdominal distension and abdominal pain. He had undergone an “extended radical resection for gastric carcinoma (total gastrectomy, Roux-en-Y anastomosis, distal pancreatectomy, and splenectomy and cholecystectomy)" due to gastric cancer three years ago. Physical examination revealed poor vitality, severe jaundice of the skin and sclera, a soft and movable mass in the upper abdomen. Laboratory examinations showed red blood cell (RBC) 3.0 × 109/L, hemoglobin (HB) 76 g/L, total bilirubin (TBIL) 187.7 µmol/L, albumin (ALB) 26.8 g/L, direct bilirubin (DBIL) 161.5 µmol/L, alkaline phosphatase (ALP) 99 IU/L. The results of tumor markers were as follows: carbohydrate antigen 19-9 (CA199) 80.82 ng/ml, carcinoembryonic antigen (CEA) 5.8 ng/ml. Abdominal CT revealed dilatation of the intrahepatic bile duct and common bile duct, a large, abdominal cystic lesion (Figure 1A), as well as left adrenal gland metastasis (Figure 1B).
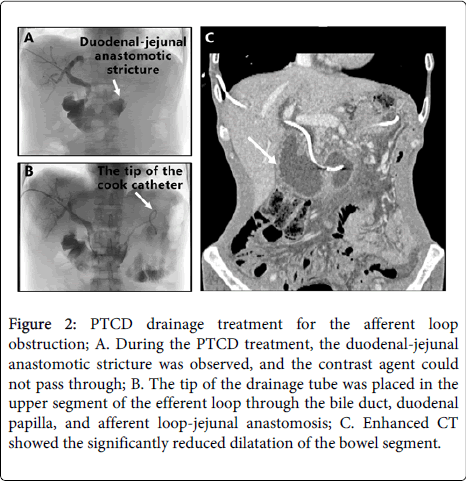
The patient was diagnosed at first with malignant obstructive jaundice. However, what is the reason for biliary obstruction? To investigate the site and cause of bile duct obstruction, we performed Magnetic Resonance Cholangiopancreatography (MRCP) examination. MRCP revealed that the cystic lesion was an expansion of small bowel loops (Figure 1C). Thus, the diagnosis of afferent loop (A-loop) obstruction was made. Subsequently, the patient underwent percutaneous transhepatic cholangial drainage (PTCD). The duodenal-jejunal anastomotic stricture (Figure 2A) was observed. Taken together, an accurate diagnosis for this case requires familiarity not only with upper abdominal cross-sectional anatomy but also with operative variations in gastrojejunostomy construction.
Figure 2: PTCD drainage treatment for the afferent loop obstruction; A. During the PTCD treatment, the duodenal-jejunal anastomotic stricture was observed, and the contrast agent could not pass through; B. The tip of the drainage tube was placed in the upper segment of the efferent loop through the bile duct, duodenal papilla, and afferent loop-jejunal anastomosis; C. Enhanced CT showed the significantly reduced dilatation of the bowel segment.
To alleviate the pressure of the intestinal tract and bile duct, and prevent cholangitis and bowel necrosis, ultrasound-guided percutaneous transhepatic biliary drainage was performed under local anesthesia. After pierced into the right intrahepatic bile duct, the guide wire was then advanced into the proximal aspect of the obstruction, and followed by a 5 French cabra catheter. The guide wire was adjusted to pass through the narrow section, and an internal-external 8.5-F drainage catheter (Dawson-Mueller drainage catheter; Cook) was inserted. The drainage tube tip was placed in the upper segment of the efferent loop through the bile duct and the A-loop-jejunal anastomosis (Figure 2B). There were no procedural complications. He was treated with Transmentil and Glutathione (GSH) after PTCD. Because of deterioration of the general condition, he was also treated with parenteral nutrition (aminoacid solution, vitamins, glucose, electrolytes, lipids) for a total caloric contribution of 1,500 kcal/daily. The abdominal pain was significantly reduced the same day after operation. The jaundice rapidly disappeared, and clinical conditions quickly improved. After five postoperative days, the follow-up CT scan showed that the dilatation of the bile duct and duodenal A-loop was significantly reduced compared to that before operation (Figure 2C). A-loop obstruction did not recur during three months of follow-up.
The patient presented with 3-month of upper abdominal distension and abdominal pain, as well as 1-month of progressive jaundice. Abdominal CT revealed left adrenal gland metastasis (Figure 1B). PTCD showed the duodenal-jejunal anastomotic stricture (Figure 2A), both CT and PTCD reveal an intestine jejuno-jejunostomy lesion. Therefore, we deducted that the stricture and intestine lesion is secondary to the adrenal metastasis.
It might be a partial obstruction in the early stage of metastasis, when upper abdominal distension and abdominal pain was the main symptoms. With the growing oppression of the left adrenal gland lump, and obstruction of intestine metastatic lesion, the chronic obstruction gradually developed into a complete blockage, causing intestine conducts bile, pancreatic juices, as well as intestinal secretions gathering, dilatation of the afferent loop, which resulted in the occurrence of severe jaundice and abdominal pain.
Discussion
Afferent loop obstruction often occurs after a subtotal gastrectomy with Billroth II anastomosis, especially in patients with the duodenal jejunal curve inclining extremely to the left side [1]. The anastomosis can cause distortion in the afferent section. In such cases, the mesentery of the efferent section located in front of the afferent section can stretch tightly to form a rope belt and compress the afferent section. This type of obstruction is a closed loop obstruction, which can easily lead to strangulation, bowel necrosis, and perforation. It often requires emergency surgery once diagnosed.
To prevent these complications, in recent years, side-to-side anastomosis (Braun anastomosis), that is, Roux-en-Y anastomosis, was performed between the afferent and efferent jejuna in Billroth II subtotal gastrectomy. Roux-en-Y anastomosis avoids anastomosis at the crossing site of the afferent and efferent loops and reduces such complications as afferent loop obstruction, so A-loop obstruction is very rarely following Roux-en-Y reconstruction [2]. In the radical resection of gastric carcinoma in this patient, Roux-en-Y anastomosis of radical gastrectomy was performed. However, due to the occurrence of the left adrenal metastasis, the invasion and compression of the growing metastatic lesion onto the opening of the afferent loop led to a chronic obstruction. It might be a partial obstruction in the early stage of metastasis, when upper abdominal distension and abdominal pain was the main symptoms. With the growing oppression of the left adrenal gland lump, and obstruction of intestine metastatic lesion, the chronic obstruction gradually developed into a complete blockage, causing intestine conducts bile, pancreatic juices, as well as intestinal secretions gathering, dilatation of the afferent loop, which resulted in the occurrence of severe jaundice and abdominal pain.
If timely treatment is not provided, further development may lead to necrosis and perforation in the bowel segment of the afferent loop, as well as other fatal complications, such as liver failure. The treatments for malignant A-loop obstruction include surgery, endoscopic treatment and PTCD [3]. However, such patients, especially after radical resection of gastric carcinoma (as in this case), are usually in poor physical condition, with severe anemia, severe jaundice, hypoproteinemia, malnutrition, and physical exhaustion, so surgical treatment is risky. In the present case, we chose PTCD because the patient was too sick to undergo surgery and the peroral approach [4] could not be used because of the patient’s altered upper gastrointestinal tract anatomy. Therefore, PTCD [5,6] can be considered a safe and effective treatment for patients with malignant A-loop obstruction.
References
- Kim DJ, Lee JH, Kim W (2013) Afferent loop obstruction following laparoscopic distal gastrectomy with Billroth-II gastrojejunostomy. J Korean Surg Soc 84: 281-286.
- Aoki M, Saka M, Morita S, Fukagawa T, Katai H (2010) Afferent loop obstruction after distal gastrectomy with Roux-en-Y reconstruction. World J Surg 34: 2389-2392.
- Chevallier P, Novellas S, Motamedi JP, Gugenheim J, Brunner P, et al. (2006) Percutaneous jejunostomy and stent placement for treatment of malignant Roux-en-Y obstruction: a case report. Clin Imaging 30: 283-286.
- De Martino C, Caiazzo P, Albano M, Pastore M, Tramutoli PR, et al. (2012) Acute afferent loop obstruction treated by endoscopic decompression. Case report and review of literature. Ann Ital Chir 83: 555-558.
- Hosokawa I, Kato A, Shimizu H, Furukawa K, Miyazaki M (2012) Percutaneous transhepatic metallic stent insertion for malignant afferent loop obstruction following pancreaticoduodenectomy: a case report. J Med Case Rep 6: 198.
- Yoshida H, Mamada Y, Taniai N, Mizuguchi Y, Kakinuma D, et al. (2008) Afferent loop obstruction treated by percutaneous transhepatic insertion of an expandable metallic stent. Hepatogastroenterology 55: 1767-1769.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14980
- [From(publication date):
March-2015 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 10433
- PDF downloads : 4547