Treatment by Cardiopulmonary Resuscitation (CPR) for Cardiac Arrest Patients Following Guidelines
Received: 01-Feb-2023 / Manuscript No. JPCM-23-88432 / Editor assigned: 07-Feb-2023 / PreQC No. JPCM-23-88432 (PQ) / Reviewed: 21-Feb-2023 / QC No. JPCM-23-88432 / Revised: 05-Apr-2023 / Manuscript No. JPCM-23-88432 (R) / Published Date: 03-May-2023
Abstract
Cardiovascular Disease (CAD) is leading a death. Cardiac arrest means heart beach stop. To date, Cardiopulmonary Resuscitation (CPR) is an efficient method for cardiac arrest patients. CPR is carried out by chest compression followed by artificial ventilation. It helps pump blood around the person’s body when the heart cannot work. The European Resuscitation Council (ERC), or the American Heart Association (AHA), created guidelines for CPR. CPR treatment is used for both Out-Hospital Cardiac Arrest Patients (OHCA) and In-Hospital Cardiac Arrest patients (IHCA). Furthermore Heart attacks are typically treated as a public health concern in hospitals. Data show that 38 million people are affected by OHCA and that between 3% and 8% of hospital patients survive and are discharged. The COVID-19 epidemic is currently used as proof. Patients with COVID-19 have emitted dangerous aerosols that should not be inhaled by medical personnel (HCWs). Guidelines for COVID-19 cardiac arrest patients were developed by the European Resuscitation Council (ERC) or the American Heart Association (AHA). Safety for Healthcare Workers (HCWs) is the focus of this guideline. Automated External Defibrillators (AEDs) are used only for CPR, according to research published recently. AEDs are medical devices that assist in rhythm analysis and provide an electrical shock to cardiac arrest patients.
Keywords: Cardiopulmonary resuscitation; Outside cardiac arrest of hospital cardiac arrest; Inside of the hospital cardiac arrest patients; Extracorporeal cardiopulmonary resuscitation; Cardiac arrest; Automated external defibrillator; Chest compression fraction; Corona virus; Neurological outcomes
Keywords
Cardiopulmonary resuscitation; Outside cardiac arrest of hospital cardiac arrest; Inside of the hospital cardiac arrest patients; Extracorporeal cardiopulmonary resuscitation; Cardiac arrest; Automated external defibrillator; Chest compression fraction; Corona virus; Neurological outcomes
Introduction
Recent studies have revealed serious issues with cardiac arrest as a cause of death. About 17.3 million people worldwide perish from cardiac arrest, according to figures from the WHO (global health agency). It is anticipated that this number would surpass 23.6 million in the year 2030. Nearly half of deaths are caused by cardiovascular disease. Due to the high prevalence of instances and the significant social and financial consequences, sudden cardiovascular arrest is one of the toughest issues in modern medicine [1]. Cardiac arrest can occur outside of the hospital (outside cardiac arrest) or inside the hospital (Inside Cardiac Arrest) (IHCA). A number of cases have been reported each year. Cardiac arrest, on the other hand, can occur in or out of the hospital. Out of Hospital Cardiac Arrest (OHCA) is a common occurrence with a low survival rate worldwide [2].
Although the guidelines for in hospital and out of hospital cardiac arrest are nearly identical, there are significant differences between the conditions that must be considered. In both cases, Cardiac Pulmonary Resuscitation is the treatment of choice (CPR). This technique is a life saving medical procedure that is primarily used to treat cardiac arrest patients. Its primary goal is to resuscitate the heart following CPR. Instant CPR with chest compressions, artificial breathing, and defibrillation is quite likely to significantly increase the patient's chance of survival when they encounter cardiac arrest. Currently, medical staff provides traditional CPR using a manual technique. External chest compression is used, then artificial ventilation to pump blood throughout the victim's body. Blood is pumped around the patient's body with the use of CPR [3].
Both In Hospital and Out of Hospital Cardiac Arrests (IHCA and OHCA) are treated using Cardiopulmonary Resuscitation (CPR), according to guidelines developed by the European Resuscitation Council (ERC) or the American Heart Association (AHA). In addition to these recommendations, the development and extension of new scientific evidence in this area can benefit from researchers' assessments of the literature in the field as well as CPR's knowledge networks and working groups. Additionally, the majority of scientific material is now available online thanks to the development of Information and Communication Technologies (ICT). This form of research, however, ignores other facets of the scientific community, such as the organization of cooperative partnerships in academic institutions and research organizations [4,5].
Early implementation of higher quality resuscitation and faster access to ECPR are attributed to higher post-IHCA survival rates (extracorporeal cardiopulmonary resuscitation). Furthermore, in studies where ECPR was used, the length of conventional Cardiopulmonary Resuscitation (CPR) appears to have a negative influence on the survival rate. When the length of the low-flow period is taken into account, the survival differences between OHCA and IHCA treated with ECPR disappear. As a result, increasing access to ECPR appears likely to reduce CPR time and improve survival after CA. ECPR has been shown to be effective in cardiac catheterization rooms, emergency departments, and pre-hospital settings in a number of studies [6].
Material and Methods
Currently, Cardiopulmonary Resuscitation (CPR) is used for COVID-19 patients with better outcomes, but at the expense of Health Care Workers (HCW), as COVID-19 patients produce aerosols (HCW). The American Heart Association (AHA), the UK resuscitation council, and many other international societies have released interim updates and updated guidelines for resuscitation during the COVID-19 pandemic [7].
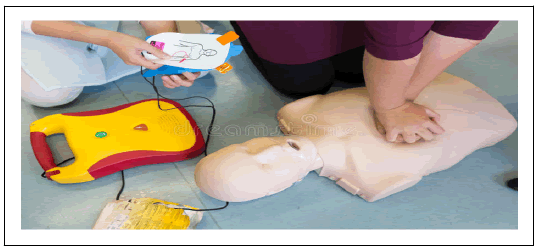
A medical device called an AED is used to defibrillate patients who have experienced cardiac arrest and treat them. An electrical shock from an AED can be used to correct CA patients' irregular heartbeats. An AED device can guarantee 90%-95% survival in 10 minutes, according to a recent study. The survival probability is 5%-10% if defibrillation is performed after 10 minutes. AEDs are also used to determine whether or not certain cardiac rhythms are shockable. An electrical shock is administered by a shockable AED to return everything to normal. On the other side, people who cannot be shocked are at a lesser risk of defibrillation [8,9].
Methodology and guidelines
Several articles on CPR and cardiac arrest have been published on Google scholar and in various journals. In this review article, we analyse and compare the outcomes of cardiac arrest patients and COVID-19 patients for both Inside and Outside of Hospital Cardiac Arrest (IHCA) and CPR treatment according to guidelines [10].
Guidelines
The European Resuscitation Council (ERC) or the American Heart Association (AHA) developed resuscitation guidelines for both Inside of Hospital Cardiac Arrest (IHCA) and Outside of Cardiac Patients (OHCA). In Europe and beyond, the ERC has established the benchmark for resuscitation protocols and training. AHA is also committed to fighting stroke and heart disease [11,12].
CPR guideline and treatment
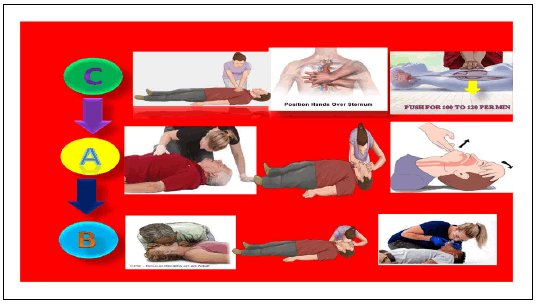
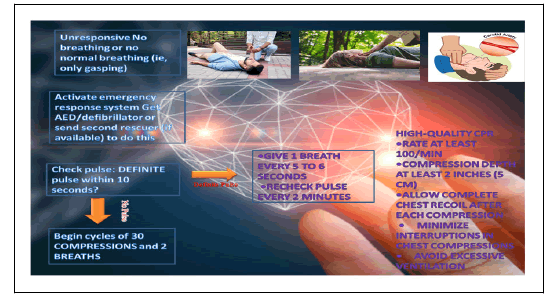
Mainly guidelines are performed by the European Resuscitation Council (ERC), or the American Heart Association (AHA). Figure 1 is shown a systematic representation of guidelines and treatment for both Inside of Hospital Cardiac Arrest (IHCA) and Outside of Cardiac Patients (OHCA). In these guidelines perform C-A-B, not A-B-C. This C is describing chest compression, A is describing Airway, and B is describing breathing [13].
The first step in CPR treatment is chest compression for adults between 5 cm (2 inch) and 6 cm (2.4 inch) deep and at a rate of at least 100 to 200 per minute. For children, compress the chest by 4 cm (1.5 inches). Blood flow is being reduced by chest compression. After performing chest compression, use the head tit chin-lift maneuver to open the person's mouth for airway. Place your palm on the person's head and gently lean back. Then, gently lift the chin forward with the other hand to open the airway. Rescue for patient breathing can be mouth-to-mouth breathing or nose-to-mouth-to-nose breathing. Currently suggested for breathing using a bag mask [14,15].
Results and Discussion
After the airway treatment, pinch the nostrils shut and cover the person's mouth with your making seal and give two rescue breaths give the first breath then see if the chest does not rise repeat the head tilt, chin lift maneuver, and give them a second breath describe in Figure 1. In one cycle, give two responses in the same manner. It must be done with caution and without using excessive force or failing to provide adequate ventilation. To restore blood flow, chest compressions are resumed [16]. Apply an Automated External Defibrillator (AED) as soon as one is available and follow the prompts. After the first shock, continue chest compressions for two minutes before administering the second shock. If you haven't been trained to use an AED, and called local emergency number Figures 1 and 2 [17].
Cardiac arrest epidemiology and treatment
Epidemiology of in-side hospital cardiac patients: The American heart association and National Cardiac Arrest (NCA) databases have published patient data on in-hospital cardiac arrest patients with rates of IHCA ranging from 1.2 to 9-10 per 1000 admissions. The GWTGR registry reports a 17% survival rate following CPR treatment. IHCA patients generally have greater 30-day survival rates than OHCA patients (24% vs. 17%) and (50.2% vs. 47.8%]. The CPC scores showed that the IHCA patients had superior long-term functional survival, but a multivariable analysis found that the site of the cardiac arrest was not a reliable predictor of functional outcome [18].
Treatment of in-side hospital cardiac patients
In-hospital cardiac arrest patients made guidelines by the European Resuscitation Council (ERC) or the American Heart Association (AHA). Cardiac arrest is first proportional to a witnessed cardiac arrest and after patients commensurate with ECG-monitoring of cardiac arrest. Then we started ≤ 1 min and then measured rhythm analysis. The treatment recommendation has not changed significantly. Use chest compression in the pre-hospital stage and defibrillation in patients with In Hospital Cardiac Arrest (IHCA) to continue progression. According to research, defibrillation should use different shocks (>1 min after the initial shock) rather than stacked shocks, as recommended in 2005. Defibrillation treatment improved the survival rate of VT/VF arrest, reflecting broader cardiac arrest strategies such as minimizing interruption chest compression for IHCA patients with persistent arrhythmias [19].
The International liaison committee on resuscitation considers airway patency during In Hospital Cardiac Arrest Patients (ICHA) to be a specific knowledge (ILCOR). Choosing an optimal airway device based on that consideration minimizes interruptions in chest compression. Many studies have recently shown that using a prehospital device such as a Bag-mask, ventilation, and Supraglottic Airway (SGA) is beneficial for IHCA patients. This entire device will be helpful in future AIRWAY-3 trials. Lura survey air management 96% survival rate in hospitals by using pre-hospital devices. According to the guideline, cardiac arrest patients are 90 mm/Hg or less than 100 mm/Hg, and temperature management is 32°C to 36°C. Furthermore, many studies are shown IHCA at a 96% survival rate after clinical evidence of CPR and reduced ROSC and good neurological outcomes [20].
Epidemiology of outside cardiac arrest
According to statistics on heart disease and stroke from the American heart association, 3,56,000 people have an Out of Hospital Cardiac Arrest each year (OHCA). According to emergency medical service, data from the ROC rescuing outcomes partnership treated 3, 47,322 people between 2010 and 2015. Home residence accounted for about 73.9% of adult OHCA cases, according to CARES data from 2020, followed by public locations (15%), nursing homes (10.9%), and laypeople in 37% of cases. The survival rate for Out of Hospital Cardiac Arrest (OHCA) ranges from 6 to 11%, while the incidence ranges from 5 to 15 per 10,000. Last year, CPR therapy and better care were used to reduce death and morbidity.
Treatment out-sides of hospital cardiac arrest patients
According to AHA guidelines, the first step for Out of Hospital Cardiac Arrest (OHCA) patients is Chest Compression (CC). The preferred chest compression fraction CCF is the total time of chest compression. The return of spontaneous circulation is most likely represented by the chest compression fraction. When the cardiac below which is several CC can restore after the 30 s. Wik found that the patients with ventricular fabrication and ambulance response intervals longer than 5 min had better outcomes with CPR before defibrillation was attempted. Based on Emergency Cardiac Care (ECC) Guidelines bougouinet reviewed 13,000 OHCA diagnosed in Paris between 2011 to 2018, with 525 benefits from intuition ECPR, with 389 being in hospital 136 out of hospitals. There is not available for airway equipment in pre-hospital steps. At that time used mouth to mouth and mouth to nose technique for oxygen and ventilation. Airway management by using equipment to avoid infection transmission various types of air way equipment and this characteristics is describe in Table 1.
| Equipment | Characteristics | |
|---|---|---|
| Moth to moth ventilation | Pre-hospital places not available of oxygen masks often use mouth-to-mouth ventilation or mouth-to-nose ventilation |  |
| Spontaneous breath | During this technique, secular spontaneously breathing patients assisting to him. In this, oxygenation is maintained by a face mask, nasal cannula or no re-breathing facemask. This facemask allows continuous positive pressure and ventilation. This method is found to decrease rate of incubation and mortality | 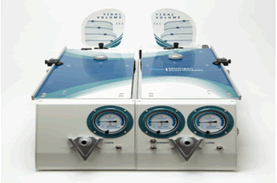 |
| Bag mask ventilation | BMV is a strand method of airway management. The mask is applied to the patient mouth to nose with a proper tight seal being formed between the patient's mouth and the show to improve oxygenation and ventilation |  |
| Oropharyngeal | The use oropharyngeal airway device is used for unresponsive or unconscious patients who have depressed airway flux |  |
| Nasopharynged | The nasopharyngeal airway is usually better for tolerance-conscious patients. It is also beneficial for patients with trauma |  |
| Supra-glottic airway devices | SGA device is useful for an untreated person. That device is use for environmental setup. SGAdevice provides a proper manner of oxygenation and ventilation | 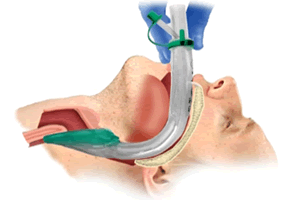 |
| Extra-glottic airway devices | This extragalactic device has extra advantages as compared to the SGA device. This device is used to seal orphan esophageal ballons to seal by pharyngeal tubes and quickly provide oxygenation and ventilation | 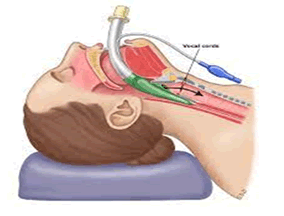 |
Table 1: Device use for out of hospital cardiac arrest patients.
COVID-19 cardiac arrest and CPR treatment outcomes
Currently, with COVID-19 about 20% of patients have cardiac arrest a larger number of patients require resuscitative effort. Many international societies like an International Liaison Committee on Resuscitation (ILCOR), the American heart association, and modification by the European Resuscitation Council (ERC) for COVID-19 guidelines.
• According to these guidelines COVID-19 patients released aerosols which are harmful to Health Care Workers (HCWs), so worker requires Personal Protective Equipment (PPE).
• Health Care Workers (HCWs) place a cloth towel over the person's mouth and nose before performing chest compressions.
• Use Automated External defibrillators (ADE) shown in Figure 3.
Chest compression requires for COVID-19
Chest compression performs for COVID-19 patients based on the guideline by mainly guidelines performed by the European Resuscitation Council (ERC) or the American Heart Association (AHA). According to that guideline barrier protection must be required. This used plastic sheet was to fully cover patients before chest compression and use three protective masks and Faceshield and gloves there is shown in Figure 3. Then started chest compression in COVID-19 patients. After every two or three cycles or 1 min to avoid poor quality compression due to fatigue but single rescuer.
Airway treatment for COVID-19 patients
COVID-19 patients generate harm full aerosols which is harm full to Health Care Workers (HCWs). Thus whenever difficulty in mask ventilation and delay in incubation is anticipated is highly considered along with the HEPA filter. To maintain ventilation.
Breathing for COVID-19 patients: Cardiac arrest in COVID-19 patients due to Respiratory Failure Syndrome (ARDS), myocardial injury, ventricular arrhythmia, shock, and drugs. Most common causes using non-shakable rhythm during cardiac arrest. However, oxygen requires a reputation for survival and that can be achieved by placing an oxygen mask. One can also consider nasal oxygen (5 L/min) through a nasal canned no current evidence that it generates viral aerosols (Figures 3-5).
Neurological outcomes: The heart rate cannulation time, ECPR optimize the organ perfusion of patients suffering from refractor CA due to Ventricular Fibrillation and Trychardia (VT/VF) by achieving hemodynamic stability, ECPR makes it possible to halt the evolution of ischemic lesion without necessary obtaining Return of Spontaneous Circulation (ROSC). It, therefore, provides time to correct serve metabolic disturbance that develops during prolonged CPR and makes possible underlying etiologies that can perpetuate refractory VF//TV. These stabilization strategies are dissociated with improved survival and satisfactory neurological outcomes in patients with refractory CA. Moreover ECPR is stabilize the patients at a constant temperature.
ECPR can improve survival after prolonged CPR but the avoidance of those who would have otherwise survived with conventional CPR alone should be a concern. The recent studies on patients with OHCA benefiting from conventional CPR have shown that 99% of surviving patients with a satisfactory neurological state underwent ROSC within a maximum of 28 to 29 min. Moreover other investigators showed that chest compression while moving in-hospital CA patients performing stretcher equipped with the wing method can produce high-quality chest compression.
According to that clinical practice, it seems reasonable to recommend the immediate transport of a patient with cardiac arrest who doesn't respond to first resuscitation measures European recommendation's first resuscitation time is 10 min. the ECPR has important implications for the implantation protocols. Implication for pre-hospital resuscitation technique, recommendations suggest 30 min of CPR before implementation of ECMO for refractory OHCA. However many studies have shown survival benefits of ECPR may extend beyond 60 min. Baudouin reported 13,000 cases of OHCA in Paris in which 12, 396 patients treated with conventional CPR 8.6% (1061) survived to discharge from the hospital compared with 8.4% of the 523 ECPR patients.
Machinery outcomes for cardiac arrest patients: Recent studies are shown poor outcomes of the CPR technique after cardiac arrest as Emergency Medical Service (EMS) requires a piece of new technological machinery for increased survival rate.
Currently, C-A-B is used for CPR treatment for both Out of Hospital Cardiac Arrest (OHCA) and In Hospital Cardiac Arrest (IHCA). Chest compression is normally used stopped for accurate shock advice analysis in automatic external defibrillators. By removing the CPR artifacts we improved the defibrillation success rate of the causes of AED application during the chest compression because of the variety of ECG arrhythmias and the variability of ECG wave from distinguishing between shockable and non-shockable arrhythmia during CPR challenging. The Table 2 is shown a systematic representation of different devices used for shakable and non-shockable rhythms without interrupting CPR and AED (Table 2).
| Device name | Use | Picture |
|---|---|---|
| Chest compression | SVM modal use for analyzing that in corporate two startedies. An adaptive LMS filter for suppress CPR artifacts and shock advice algorithms (SAA) SAA modal use for both shakable and non-shakable decision algorithm. | 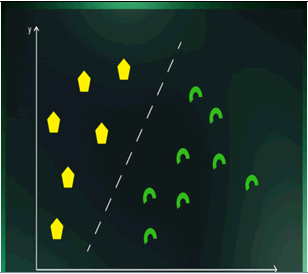 |
| CNN | CNN modal use for deep learning alogorithm for accurtly dictating shakable rhythm or defibrillator during chest compression provide by Load Distributing Band (LDB) device. LBD is mechanized chest compression used for OHCA patients. This method Recursive Least Squares (RLS) filter to remove chest compression artifacts from ECG and CNN-based algorithm classified filtered ECG into shakable or non-shakable rhythm. | |
| Rhythms, annotation external defibrilation | BP-NN modal used to distinguish between various ECG signals, even extreme CPR artifacts. | |
| Shockable rhythms | Shakable rythms are those heart rhythms that are faster than normal heart rhythms and can be treat with defibrillation shock. |  |
| Ventricular Fibrillation (VF) | In this type of rhythm, the heart rate is too high and goes up to 500 bpm. It is a dangerous cardiac disturbance; if no shock is delivered within a few minutes, this may result in hypoxic brain damage and death. |  |
| Ventricular tachycardia | In this type of rhythm, the heart rate is higher than normal, in the range of 150 bpm-250 bpm. Defibrillation can reduce such heart rate to normal. | 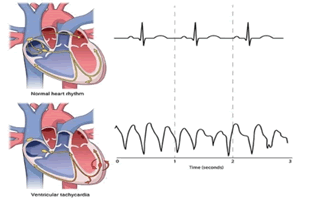 |
| Non-shockable rhythms | Non-shockable rhythms are those rhythms that cannot be treated with defibrillation shocks. These types of rhythms vary from normal to very dangerous. The AED does not provide defibrillation if it detects non-shockable rhythms. | 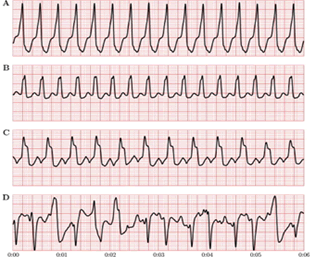 |
| Asystole (ASYS) | This is a flatline rhythm meaning there is no heartbeat or electrical activity. The heart is not functioning, and defibrillation does not work; hence, less than 2% of people with Asystole survive. | 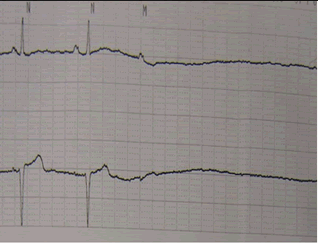 |
| Pulseless Electrical Activity (PEA) | This is a life-threatening and unshockable cardiac rhythm. Despite the presence of coordinated cardiac electrical activity in this rhythm, there is no perceptible pulse. | 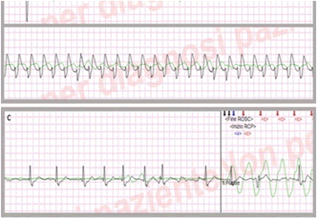 |
Table 2: Systematic representation of AED devices.
Cardiac arrest remains a leading cause of mortality and morbidity. Several studies have shown Emergency Cardiac arrest (ECC) uses CPR treatment for both IHCA and OHCA. For the treatment of CPR made, guidelines by the American Heart Agency (AHA) and resuscitation created by the European Resuscitation Council (ERC). Based on their policies, CPR treatment performed in several steps is a “C-A-B” Chest compression, airway and breathing. Chest compression of 100 to 200 per minute is reduced blood flow. After performing chest compression, open the mouth of the patient for airway. After completing this step, the next step is breathing. During the breathing, step rescue for patients can be mouth to mouthbreathing or nose-to-mouth breathing; currently, use a bag mask. After performing this step check a chest to ensure it doesn’t rise repeat the process. For OHCA patients who are not trained in this technique, call the emergency number, and the operator may be able to give you instructions.
The current situation is COVID-19 patients released aerosol, which is harmful to the patient and increases the chance of spreading infection of COVID-19. However, the American heart association and ILCOR made guidelines for COVID-19. According to the guidelines, patients must be fully covered by transparent plastics before chest compression and use equipment for air or breathing. Health Care Workers (HCWs) use a three-layer mask and must require Personal Protective Equipment (PPE) kit. After performing CPR wash your hands with sanitizers and hand wash. CPR treatment for OHCA and IHCA patients has reasonable survival rates and perpetuates refractory VF/TV. These stabilization strategies are associated with improved patient survival and satisfactory neurological outcomes. Currently, studies are shown to use Automated External Defibrillator (AED) devices with good results.
Conclusion
Cardiac Arrest (CA) is a leading death and a major public issue. To date, CPR treatment is used for cardiac arrest patients. CPR, with chest compression and artificial ventilation, along with defibrillation, is a method to reduce blood flow and improve the patient's survival. The European Resuscitation Council (ERC) and American Heart Agency (AHA) created the resuscitation guideline for COVID and non-COVID patients. The research studies show AED device helps diagnose, and CPR treatment is beneficial and innominate to death. The desirable benefits of its use will be an adequate reduction, promoting survival and good neurological outcomes.
References
- Grasner JT, Bossaert L (2013) Epidemiology and management of cardiac arrest: What registries are revealing. Best Pract Res Clin Anaesthesiol 27: 293-306.
[Crossref] [Google Scholar] [PubMed]
- Kempster K, Howell S, Bernard S, Smith K, Cameron P, et al. (2021). Out-of-hospital cardiac arrest outcomes in emergency departments. Resuscitation 166: 21-30.
[Crossref] [Google Scholar] [PubMed]
- Meaney PA, Bobrow BJ, Mancini ME, Christenson J, De Caen AR, et al. (2013) Cardiopulmonary resuscitation quality: Improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation 128: 417-435.
- Carrick RT, Park JG, McGinnes HL, Lundquist C, Brown KD, et al. (2020) Clinical predictive models of sudden cardiac arrest: A survey of the current science and analysis of model performances. J Am Heart Assoc 9: 17625.
[Crossref] [Google Scholar] [PubMed]
- Ravishankar MN (2013) Public ICT innovations: A strategic ambiguity perspective. J Inf Technol 28: 316-332.
[Crossref] [Google Scholar] [PubMed]
- Davis PM, Walters WH (2011) The impact of free access to the scientific literature: A review of recent research. J Med Libr Assoc 99.
[Crossref] [Google Scholar] [PubMed]
- Montoya FG, Alcayde A, Banos R, Manzano-Agugliaro F (2018) A fast method for identifying worldwide scientific collaborations using the Scopus database. Telemat Inform 35: 168-185.
[Crossref] [Google Scholar] [PubMed]
- Shen A X, Lee MK, Cheung CM, Chen H (2010) Gender differences in intentional social action: We-intention to engage in social network-facilitated team collaboration. J Inf Technol 25: 152-169.
[Crossref] [Google Scholar] [PubMed]
- Le Guen M, Nicolas-Robin A, Carreira S, Raux M, Leprince P, et al. (2011) Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit Care 15: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Lee JJ, Han SJ, Kim HS, Hong KS, Choi HH, et al. (2016) Out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal membrane oxygenation: Focus on survival rate and neurologic outcome. Scand J Trauma Resusc Emerg Med 24: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Danial P, Hajage D, Nguyen LS, Mastroianni C, Demondion P, et al. (2018) Percutaneous versus surgical femoro-femoral veno-arterial ECMO: A propensity score matched study. Intensive Care Med 44: 2153-2161.
[Crossref] [Google Scholar] [PubMed]
- Bellezzo JM, Shinar Z, Davis DP, Jaski BE, Chillcott S, et al. (2012) Emergency physician-initiated extracorporeal cardiopulmonary resuscitation. Resuscitation 83: 966-970.
[Crossref] [Google Scholar] [PubMed]
- Lamhaut L, Hutin A, Puymirat E, Jouan J, Raphalen JH, et al. (2017) A pre-hospital Extracorporeal Cardio Pulmonary Resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: An observational study and propensity analysis. Resuscitation 117: 109-117.
[Crossref] [Google Scholar] [PubMed]
- Megarbane B, Leprince P, Deye N, Resiere D, Guerrier G, et al. (2007) Emergency feasibility in medical intensive care unit of extracorporeal life support for refractory cardiac arrest. Intensive Care Med 33: 758-764.
[Crossref] [Google Scholar] [PubMed]
- Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, et al. (2020) Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: From the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation 141: 933-943.
[Crossref] [Google Scholar] [PubMed]
- Fabbri A, Marchesini G, Spada M, Iervese T, Dente M, et al. (2006) Monitoring intervention programmes for out-of-hospital cardiac arrest in a mixed urban and rural setting. Resuscitation 71: 180-187.
[Crossref] [Google Scholar] [PubMed]
- Andersson A, Arctaedius I, Cronberg T, Levin H, Nielsen N, et al. (2022) In-hospital versus out-of-hospital cardiac arrest: Characteristics and outcomes in patients admitted to intensive care after return of spontaneous circulation. Resuscitation 176: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Kleinman ME, Perkins GD, Bhanji F, Billi JE, Bray JE, et al. (2018) ILCOR scientific knowledge gaps and clinical research priorities for cardiopulmonary resuscitation and emergency cardiovascular care: A consensus statement. Resuscitation 137: 802-819.
[Crossref] [Google Scholar] [PubMed]
- Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, et al. (2015) Part 1: Executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132: 315-367.
[Crossref] [Google Scholar] [PubMed]
- Escutnaire J, Genin M, Babykina E, Dumont C, Javaudin F, et al. (2018) Traumatic cardiac arrest is associated with lower survival rate vs. medical cardiac arrest-Results from the French national registry. Resuscitation 131: 48-54.
[Crossref] [Google Scholar] [PubMed]
Citation: Dave DP (2023) Treatment by Cardiopulmonary Resuscitation (CPR) for Cardiac Arrest Patients Following Guidelines. J Palliat Care Med 13: 532.
Copyright: © 2023 Dave PD. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2044
- [From(publication date): 0-2023 - Nov 28, 2025]
- Breakdown by view type
- HTML page views: 1670
- PDF downloads: 374