Transmission of Enigmatic Mundinia Parasites
Received: 06-Jun-2022 / Manuscript No. JIDT-22-65986 / Editor assigned: 10-Jun-2022 / PreQC No. JIDT-22-65986 (PQ) / Reviewed: 24-Jun-2022 / QC No. JIDT-22-65986 / Revised: 30-Jun-2022 / Manuscript No. JIDT-22-65986 (R) / Published Date: 07-Jul-2022 DOI: 10.4172/2332-0877.1000507
Abstract
Mundinia, the recently established Leishmania subgenus, includes five species, three of which are pathogenic to humans. Although Mundinia represents the oldest branch of the genus Leishmania, most species have escaped the attention of scientists and have only been discovered in the last 20 years. Their transmission ecology is enigmatic, with unknown identity of reservoir hosts and insect vectors. This mini-review summarizes the history of Mundinia discovery and the current knowledge about the reservoirs and vectors with emphasis on the role of biting midges (Diptera: Ceratopogonidae) in their transmission.
Keywords: Mundinia; L. macropodum; L. enriettii; L. orientalis; L. martiniquensis; Culicoides sonorensis
Introduction
Leishmania (Kinetoplastida: Trypanosomatidae) are digenetic parasites circulating between mammal or reptile vertebrate hosts and insect vectors. They are currently divided into four subgenera. The most important and abundant human parasites belong to subgenera Viannia and Leishmania, the third subgenus Sauroleishmania includes reptile parasites [1]. The fourth subgenus Mundinia was established in 2016 by Espinosa, et al. for five species previously known as the L. enriettii complex. It is the most ancient group, diverging at the base of a phylogenetic tree of the Leishmania genus [1].
Literature Review
Mundinia is an exceptional and enigmatic subgenus in several aspects:
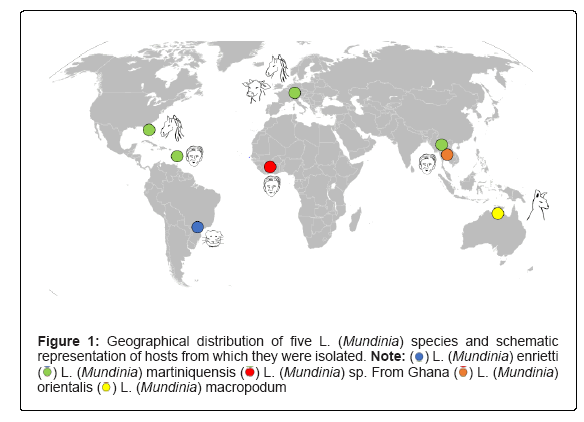
Worldwide geographical distribution
The five species are distributed on all continents except Antarctica (Figure 1): L. enriettii occurs in Brazil, L. sp. strain GH5, not yet formally described, in Africa (Ghana), L. orientalis in southeast Asia and L. macropodum in Australia, representing the only Leishmania species known from that continent. The fifth species, L. martiniquensis, has been reported from areas as distant as the island of Martinique, Florida, central Europe and southeast Asia. This wide distribution of the subgenus has been attributed to its ancient origin and is explained by the formation of individual species from a common ancestor after the breakup of Gondwana [2]. However, in the case of L. martiniquensis, the recent introduction and anthropogenic spread must be considered, as the infection is only known from humans and domestic animals.
The hidden way of life
Despite their ancient origins, three species (L. macropodum, L. orientalis and the unnamed African species) have escaped scientific knowledge and have only been discovered in the last 20 years. The remaining two species have been known for a long time, but were reported very sporadically. This is particularly true for the Brazilian L. enriettii. It was first isolated in 1948 from domestic guinea pigs, then detected 20 years later in 1967 and after another long gap again in 1994, each time in domestic guinea pigs [3,4]. However, as a species non-pathogenic to humans, L. enriettii has become a popular model organism for experimental studies. Leishmania martiniquensis was first described in 1995 in an HIV-infected man in Martinique and was initially misidentified as a monoxenous “lower” trypanosomatid. Two years later, the same parasite was also reported in Martinique in an immunocompetent patient [5,6]. In 2014, Pothirat, et al. showed that autochthonous infections in cattle or horses sporadically reported from Florida, Switzerland and Germany and occasionally causing human infections in south-east Asia, belong to the same Mundinia species [7-11]. In the same year the name L. martiniquensis was established [12]. In Thailand, L. martiniquensis is not the only species of the subgenus Mundinia, the other being L. orientalis, formally described in 2018 [13]. In older literature, all Thai isolates were confused and referred to as “L. siamensis”. This name was first used by Sukmee, et al. for the sequence of their isolate submitted in GenBank and then introduced into the scientific literature by Müller, et al. [9,14]. As the name “L. siamensis” has never been formally described, it is not a valid name and should no longer be used.
In horses and cattle, L. martiniquensis causes skin lesion while in humans, a wide spectrum of manifestations ranging from cutaneous and diffuse cutaneous to visceral forms has been reported [5,6,8-10,14,15]. Similarly, L. orientalis is also responsible for both diffuse cutaneous and visceral leishmaniasis [16]. The African Mundinia species was hidden among human cutaneous leishmaniasis cases in the Volta region of Ghana caused by L. major. However, in 2009 the parasite was identified as a new Leishmania species, in 2015 the strain was isolated and according to phylogenetic analysis placed into the subgenus Mundinia [17,18]. Australia was traditionally considered a continent where Leishmania species were not endemic until 2004, when a case of autochthonous cutaneous leishmaniasis was described in red kangaroos (Marcopus rufus) in Australia's Northern Territory [19].
Unknown reservoirs
No reservoir wild hosts have been identified for any species of the subgenus Mundinia. Leishmania enriettii has only been found in domestic guinea pigs, but experimental infections of wild guinea pigs (and several other species of wild mammals) have failed [3]. In the case of L. macropodum, all Australian causes of CL have been diagnosed in captive animals-red kangaroos (Macropus rufus), the northern wallaroo (M. robustus woodwardi), the black wallaroo (M. bernardus) and the agile wallaby (M. agilis agilis) [19,20]. All records have been restricted to the rural Darwin area in the Northern Territory with a humid tropical climate, where only agile wallabies are native, but further epidemiological studies are needed to determine their possible role as reservoirs of L. macropodum [20]. The autochthonous cases of L. martiniquensis in horses and cattle in central Europe and Florida are truly enigmatic, the animal reservoirs are completely unknown and have yet to be identified, and the same is true for human-infecting species in Thailand and Ghana. In Thailand, Leishmania DNA has been found in Rattus rattus, making this rodent species suspected of serving as a reservoir, but the capacity of black rats to harbour the parasite long-term and their infectiousness to sand flies has not yet been proven [21]. Experimental studies on the genera Arvicanthis and Mastomys have been done but did not demonstrate a reservoir role of these rodents for the Ghanaian Mundinia species [22]. Mundinia have probably evolved a well-balanced relationship with their reservoir hosts over a long evolutionary history and cause only asymptomatic unapparent infections, which are thus difficult to detect.
Unique vectors
Although species identity for vectors of any Mundinia species is not confirmed yet, the findings so far are fascinating. For many years, there was a widely accepted paradigm that Leishmania species pathogenic to humans are transmitted exclusively by phlebotomine sand flies of the genus Phlebotomus in the Old World and Lutzomyia in the New World [23,24]. But most Leishmania of the subgenus Mundinia have never been found in sand flies, with exception of PCR detection of Mundinia DNA in Thai Sergentomyia (Neophlebotomus) gemmea and S. iyengari [25,26]. However, molecular findings cannot be considered as a proof of the vector identification. Without microscopy, it is not possible to distinguish late mature infections from early ones which are non-specific and may be lost with defecation in refractory vectors [27]. The paradigm of exclusive transmission of Leishmania by sand flies has been seriously challenged by discoveries related to the subgenus Mundinia published in the last decade.
In areas of Australian L. macropodum distribution, the extensive field survey revealed DNA of the parasites in 6% females of three species of biting midges of the genus Forcipomyia (Diptera: Ceratopogonidae) while no Leishmania-positive specimens were detected among nearly 2000 sand fly females collected. Importantly, heavy late stage infections and presence of metacyclic forms in biting midges were confirmed also microscopically [28]. Consequent laboratory experiments have revealed susceptibility of North American C. sonorensis to infection with L. enriettii, L. macropodum and L. orientalis [29,30].
Discussion
Altogether, these studies had showed that biting midges satisfy most of Killick-Kendrick’s criteria of vector competence [31]. However, the most important criterion was still missing, namely the demonstrations of transmission by the vector bite. This has changed with the recent publication of Becvar, et al [32]. These authors compared the development of all 5 Mundinia species in biting midges and sand flies and demonstrated experimental transmissions of three Mundinia species, L. martiniquensis, L. orientalis and L. sp. from Ghana by biting midges C. sonorensis to BALB/c mice. The parallel experiments with the same parasite lines and epidemiologically relevant sand fly species resulted in limited infections and no transmission to mice. This study therefore provides the strong evidence that biting midges may play a role in the transmission of Mundinia parasites and further field-based studies are necessary to identify particular vector species in areas of pathogen transmission. Besides Australian Forcipomyia species, another good candidate emerged in 2021, when L. martiniquensis DNA was detected in wild caught C. mahasarakhamense near the home of a leishmaniasis patient in Lamphun province, northern Thailand [33,34].
Conclusion
Finally, the reduced repertoire of enzymes modifying LPG side chains, a molecule important for Leishmania and Viannia development in the sand fly, is also indicative of non-standard Mundinia vectors. The identification of vectors and reservoir hosts of Mundinia parasites is a significant challenge and is also of importance in the context of the unique geographical distribution of L. martiniquensis, which is the only species of the Leishmania genus occurring in Central Europe.
References
- Espinosa OA, Serrano MG, Camargo EP, Teixeira MMG, Shaw JJ (2018) An appraisal of the taxonomy and nomenclature of trypanosomatids presently classified as Leishmania and Endotrypanum. Parasitology 145:430-442.
[Crossref] [Google Scholar] [PubMed]
- Barratt J, Kaufer A, Peters B, Craig D, Lawrence A, et al. (2017) Isolation of Novel Trypanosomatid, Zelonia australiensis sp. nov. (Kinetoplastida: Trypanosomatidae) provides support for a gondwanan origin of dixenous parasitism in the Leishmaniinae. PLoS Negl Trop Dis 11:e0005215.
[Crossref] [Google Scholar] [PubMed]
- Muniz J, Medina H (1948) Cutaneous leishmaniasis of the guinea pig, Leishmania enriettii n. sp. Hospital (Rio J) 33:7-25.
[PubMed]
- Machado MI, Milder RV, Pacheco RS, Silva M, Braga RR, et al. Naturally acquired infections with Leishmania enriettii Muniz and Medina 1948 in guinea-pigs from Sao Paulo, Brazil. Parasitology 109:135-138.
[Crossref] [Google Scholar] [PubMed]
- Dedet JP, Roche B, Pratlong F, Cales-Quist D, Jouannelle J, et al. (1995) Diffuse cutaneous infection caused by a presumed monoxenous trypanosomatid in a patient infected with HIV. Trans R Soc Trop Med Hyg 89:644-646.
[Crossref] [Google Scholar] [PubMed]
- Boisseau-Garsaud AM, Cales-Quist D, Desbois N, Jouannelle J, Jouannelle A, et al. (2000) A new case of cutaneous infection by a presumed monoxenous trypanosomatid in the island of Martinique (French West Indies). Trans R Soc Trop Med Hyg 94:51-52.
[Crossref] [Google Scholar] [PubMed]
- Pothirat T, Tantiworawit A, Chaiwarith R, Jariyapan N, Wannasan A, et al. (2014) First isolation of Leishmania from Northern Thailand: Case report, identification as Leishmania martiniquensis and phylogenetic position within the Leishmania enriettii complex. PLoS Negl Trop Dis 8:e3339.
[Crossref] [Google Scholar] [PubMed]
- Reuss SM, Dunbar MD, Mays MBC, Owen JL, Mallicote MF, et al. (2012) Autochthonous Leishmania siamensis in horse, Florida, USA. Emerg Infect Dis 18:1545-1547.
[Crossref] [Google Scholar] [PubMed]
- Müller N, Welle M, Lobsiger L, Stoffel MH, Boghenbor KK, et al. (2009) Occurrence of Leishmania sp. in cutaneous lesions of horses in Central Europe. Vet Parasitol 166:346-351.
[Crossref] [Google Scholar] [PubMed]
- Lobsiger L, Müller N, Schweizer T, Frey CF, Wiederkehr D, et al. (2010) An autochthonous case of cutaneous bovine leishmaniasis in Switzerland. Vet Parasitol 169:408-414.
[Crossref] [Google Scholar] [PubMed]
- Leelayoova S, Siripattanapipong S, Manomat J, Piyaraj P, Tan-Ariya P, et al. (2017) Leishmaniasis in Thailand: A review of causative agents and situations. Am J Trop Med Hyg 96:534-542.
[Crossref] [Google Scholar] [PubMed]
- Desbois N, Pratlong F, Quist D, Dedet JP (2014) Leishmania (Leishmania) martiniquensis n. sp. (Kinetoplastida: Trypanosomatidae), description of the parasite responsible for cutaneous leishmaniasis in Martinique Island (French West Indies). Parasite 21:12.
[Crossref] [Google Scholar] [PubMed]
- Jariyapan N, Daroontum T, Jaiwong K, Chanmol W, Intakhan N, et al. (2018) Leishmania (Mundinia) orientalis n. sp. (Trypanosomatidae), a parasite from Thailand responsible for localised cutaneous leishmaniasis. Parasit Vectors 11:351.
[Crossref] [Google Scholar] [PubMed]
- Sukmee T, Siripattanapipong S, Mungthin M, Worapong J, Rangsin R, et al. (2008) A suspected new species of Leishmania, the causative agent of visceral leishmaniasis in a Thai patient. Int J Parasitol 38:617-622.
[Crossref] [Google Scholar] [PubMed]
- Liautaud B, Vignier N, Miossec C, Plumelle Y, Kone M, et al. (2015) First case of visceral leishmaniasis caused by Leishmania martiniquensis. Am J Trop Med Hyg 92:317-319.
[Crossref] [Google Scholar] [PubMed]
- Bualert L, Charungkiattikul W, Thongsuksai P, Mungthin M, Siripattanapipong S, et al. (2012) Autochthonous disseminated dermal and visceral leishmaniasis in an AIDS patient, Southern Thailand, caused by Leishmania siamensis. Am J Trop Med Hyg 86:821-824.
[Crossref] [Google Scholar] [PubMed]
- Villinski JT, Klena JD, Abbassy M, Hoel DF, Puplampu N, et al. (2008) Evidence for a new species of Leishmania associated with a focal disease outbreak in Ghana. Diagn Microbiol Infect Dis 60:323-327.
[Crossref] [Google Scholar] [PubMed]
- Kwakye-Nuako G, Mosore MT, Duplessis C, Bates MD, Puplampu N, et al. (2015) First isolation of a new species of Leishmania responsible for human cutaneous leishmaniasis in Ghana and classification in the Leishmania enriettii complex. Int J Parasitol 45:679-684.
[Crossref] [Google Scholar] [PubMed]
- Rose K, Curtis J, Baldwin T, Mathis A, Kumar B, et al. (2014) Cutaneous leishmaniasis in red Kangaroos: isolation and characterisation of the causative organisms. Int J Parasitol 34:655-664.
[Crossref] [Google Scholar] [PubMed]
- Dougall A, Shilton C, Choy JL, Alexander B, Walton S (2009) New reports of Australian cutaneous leishmaniasis in Northern Australian macropods. Epidemiol Infect 137:1516-1520.
[Crossref] [Google Scholar] [PubMed]
- Jungudomjaroen S, Phumee A, Chusri S, Kraivichian K, Jariyapan N, et al. (2015) Detection of Leishmania martiniquensis DNA in various clinical samples by quantitative PCR. Trop Biomed 32:736-744.
[Google Scholar] [PubMed]
- Sadlova J, Vojtkova B, Becvar T, Lestinova T, Spitzova T, et al. (2019) Host competence of the African rodents Arvicanthis neumanni, A. niloticus and Mastomys natalensis for Leishmania donovani from Ethiopia and L. ( Mundinia) sp. from Ghana. Int J Parasitol Parasites Wildl 11:40-45.
[Crossref] [Google Scholar] [PubMed]
- Killick-Kendrick R (1990) Phlebotomine vectors of the leishmaniases: A review. Med Vet Entomol 4:1-24.
[Crossref] [Google Scholar] [PubMed]
- Maroli M, Feliciangeli MD, Bichaud L, Charrel RN, Gradoni L (2013) Phlebotomine sandflies and the spreading of leishmaniases and other diseases of public health concern. Med Vet Entomol 27:123-147.
[Crossref] [Google Scholar] [PubMed]
- Kanjanopas K, Siripattanapipong S, Ninsaeng U, Hitakarun A, Jitkaew S, et al. (2013) Sergentomyia (Neophlebotomus) gemmea, a potential vector of Leishmania siamensis in southern Thailand. BMC Infect Dis 13:333.
[Crossref] [Google Scholar] [PubMed]
- Siripattanapipong S, Leelayoova S, Ninsaeng U, Mungthin M (2018) Detection of DNA of Leishmania siamensis in Sergentomyia (Neophlebotomus) iyengari (Diptera: Psychodidae) and molecular identification of blood meals of sand flies in an affected area, Southern Thailand. J Med Entomol 55:1277-1283.
[Crossref] [Google Scholar] [PubMed]
- Seblova V, Sadlova J, Carpenter S, Volf P (2014) Speculations on biting midges and other bloodsucking arthropods as alternative vectors of Leishmania. Parasit Vectors 7:222.
[Crossref] [Google Scholar] [PubMed]
- Dougall AM, Alexander B, Holt DC, Harris T, Sultan AH, et al. (2011) Evidence incriminating midges (Diptera: Ceratopogonidae) as potential vectors of Leishmania in Australia. Int J Parasitol 41:571-579.
[Crossref] [Google Scholar] [PubMed]
- Seblova V, Sadlova J, Vojtkova B, Votypka J, Carpenter S, et al. (2015) The biting midge Culicoides sonorensis (Diptera: Ceratopogonidae) is capable of developing late stage infections of Leishmania enriettii. PLoS Negl Trop Dis 9:e0004060.
[Crossref] [Google Scholar] [PubMed]
- Chanmol W, Jariyapan N, Somboon P, Bates MD, Bates PA (2019) Development of Leishmania orientalis in the sand fly Lutzomyia longipalpis (Diptera: Psychodidae) and the biting midge Culicoides soronensis (Diptera: Ceratopogonidae). Acta Trop 199:105157.
[Crossref] [Google Scholar] [PubMed]
- Killick-Kendrick R (1999) The biology and control of phlebotomine sand flies. Clin Dermatol 17:279-289.
[Crossref] [Google Scholar] [PubMed]
- Becvar T, Vojtkova B, Siriyasatien P, Votypka J, Modry D, et al. (2021) Experimental transmission of Leishmania (Mundinia) parasites by biting midges (Diptera: Ceratopogonidae). PLoS Pathog 17:e1009654.
[Crossref] [Google Scholar] [PubMed]
- Sunantaraporn S, Thepparat A, Phumee A, Sor-Suwan S, Boonserm R, et al. (2021) Culicoides Latreille (Diptera: Ceratopogonidae) as potential vectors for Leishmania martiniquensis and Trypanosoma sp. in northern Thailand. PLoS Negl Trop Dis 15:e0010014.
[Crossref] [Google Scholar] [PubMed]
- Butenko A, Kostygov AY, Sádlová J, Kleschenko Y, Bečvář T, et al. (2019) Comparative genomics of Leishmania (Mundinia). BMC Genomics 20:726.
[Crossref] [Google Scholar] [PubMed]
Citation: Sadlova J, Becvar T, Volf P (2022) Transmission of Enigmatic <em>Mundinia</em> Parasites. J Infect Dis Ther 10: 507. DOI: 10.4172/2332-0877.1000507
Copyright: © 2022 Sadlova J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1671
- [From(publication date): 0-2022 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 1443
- PDF downloads: 228

 L. (Mundinia) enrietti
L. (Mundinia) enrietti  L. (Mundinia) martiniquensis
L. (Mundinia) martiniquensis  L. (Mundinia) sp. From Ghana
L. (Mundinia) sp. From Ghana  L. (Mundinia) orientalis
L. (Mundinia) orientalis  L. (Mundinia) macropodum
L. (Mundinia) macropodum