Research Article Open Access
Translating Falls Prevention Knowledge for Community-Dwelling People Living With Dementia: Design Protocol for a Mixed-Method Intervention
Claudia Meyer1*, Keith Hill2, Sophie Hill3 and Briony Dow4
1Claudia Meyer: National Ageing Research Institute, Parkville, Victoria, Australia
2School of Physiotherapy and Exercise Science, Faculty of HealthSciences, Curtin University, Perth, Western Australia, Australia
3Centre for Health Communication and Participation, School ofPublic Health and Human Biosciences, La Trobe University, Bundoora, Victoria, Australia
4National Ageing Research Institute, Royal Melbourne Hospital, Victoria, Australia
- Corresponding Author:
- Claudia Meyer
PhD candidate, Centre for Health
Communication and Participation
School of Public Health andHuman Biosciences
La Trobe University, Bundoora
Victoria, 3086, Australia
Tel: 61431100752
E-mail: c.meyer@nari.unimelb.edu.au
Received date: January 23, 2015; Accepted date: March 24, 2015; Published date: April 02, 2015
Citation: Meyer C, Hill K, Hill S, Dow B (2015) Translating Falls Prevention Knowledge for Community-Dwelling People Living With Dementia: Design Protocol for a Mixed-Method Intervention. J Alzheimers Dis Parkinsonism 5:185. doi:
Copyright: © 2015 Meyer C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Alzheimers Disease & Parkinsonism
Abstract
Background: There are a growing number of older people living with dementia (PLWD) across the globe, and this population has a higher rate of falls than cognitively intact older people. Strong research evidence does not yet exist for preventing falls in community-dwelling PLWD, but best practice guidelines suggest using similar strategies to those used for cognitively intact older adults. This study will use a knowledge translation theoretical framework, supported by several behaviour change theories, to seek to understand the complex phenomenon of moving falls prevention research evidence into practice for PLWD. Methods: A mixed-method design will be employed, with two components investigating falls prevention knowledge translation. Study 1 for PLWD and their caregivers will consist of an initial interview and data collectionabout falls risk, self-efficacy and carer burden. Goal setting will be used to develop a collaborative plan of action, which will be followed by monthly home visits over 6 months to implement the targeted falls prevention strategies according to the readiness by PLWD and their caregiver to change behaviour. Subsequent assessments will be conducted at 6- and 12-months.Study 2 for staff of community care agencies will consist of four action research sessions over 6 months to implement change in practice, related to translating falls prevention knowledge. Discussion: Data will be analysed qualitatively and quantitatively, using a variety of appropriate methods. Drawing together all of the qualitative and quantitative data from various data collection points, a discussion aid, including a set of algorithms for each falls risk factor, will be developed. This study offers the opportunity to explore how falls prevention strategies can be best adopted by PLWD and their caregivers, taking into account their individual needs, preferences and abilities. Community care health professionals have a key role in the translation of falls prevention knowledge. This study will consider the factors influencing this process for PLWD and their caregivers.
Keywords
Methodology; Falls prevention; Dementia; Caregivers; Knowledge translation; Mixed methods
Abbreviations
PLWD: People living with dementia; CG: Caregiver; CBPR: Community based participatory research; FROP-Com: Falls Risk for Older Persons – Community; ADCS: Alzheimer’s Disease Co-operative Study Activities of Daily Living Inventory; DSRS: Dementia Severity Rating Scale; CHAMPS: Community Healthy Activities Model Program for Seniors Institute for Health & Aging Activities Questionnaire for Older Adults; OFDG: Ottawa Family Decision Guide
Background
The global population continues to age, with projections that the number of people over 60 years will rise from 11% to 22% between 2000 and 2050, with a concomitant increase in the number of people living with dementia (PLWD) [1]. Should preventive or treatment options for dementia not be realised, the number of older PLWDacross the world will double by 2030 (from 35.6 million) and triple by 2050 [1]. Dementia is a term used to describe over 100 different diseases, characterised by progressive degeneration in brain function. Impairments in language, memory, perception and personality have profound consequences on individuals, families and society [2].
Despite themarked impact of dementia on an individual, PLWD express the desire to remain living independently in the community [3]. Within Australia, approximately 70% of PLWD reside in the community, either independently or with the assistance of informal caregivers [2]. Informal caregivers provide assistance to PLWD for everyday activities [2], the need for which increases as the disease progresses. Formal community care services support 77% of this population;with community care health professionals in a unique position to advocate a human rights approach to care and offer choice through delivery of equitable and non-discriminatory services [4]. Informal caregivers are an important resource for seeking and implementing health information [5]. Together with the person with dementia, health professionals and informal caregivers have the capacity to address the important health issue of preventing falls.
Approximately 70-80% of PLWD fall at least once each year, twice the rate of cognitively intact older people [6]. They are at greater risk of sustaining a fracture, including hip fracture, following falls, and often have poor outcomes [7]. A number of falls prevention strategies, such as medication review and home safety modifications, for older people in the community have been shown to be effective in reducing falls [8]. Yet a previously successful falls prevention program [9] implemented for PLWD showed less than convincing results suggesting that an alternative approach for PLWD may be required. A recent systematic review highlighted the need for involvement of health professionals as a resource for support and information; the inclusion of the caregiving dyad in program delivery; and a focus on individual needs and preferences [10].
Strong research evidence for effective falls prevention strategies for PLWD does not yet exist. Preliminary work is underway to understand the differing falls prevention needs of PLWD [6,11]. While this work is important, the higher rate of falls and injurious falls in this population makes itimperative to address the prevention of falls using the current best available evidence. Best practice guidelines recommend the implementation of similar strategies for PLWD as have been shown to be effective for cognitively intact older adults [8]. However, the common characteristics of memory loss and impairments in judgement and problem solving with dementia make it unclear whether PLWD can adopt falls prevention strategies in the same way as cognitively intact older persons [11-13]. A strong theoretical framework is required to explore thecomplexity of engagementof PLWD and their caregivers in falls prevention strategies.
The primary aim of this exploratory study is twofold:
• To explore the translation of falls prevention knowledge (falls risk reduction strategies) for PLWD and their caregivers, within the context of readiness to change behaviour; and
• To understand the translation of falls prevention knowledge for PLWD and their caregivers from the perspective of community care staff, and develop a discussion aid to assist community care staff to manage falls within this population.
To meet this aim, the following objectives will be addressed:
• Identify the existing evidence within the literature for best practice falls prevention, dementia care and falls prevention for community-dwelling people living with dementia.
• Identify perceptions of PLWD and their caregiver of the causes and consequences of falls; the importance and meaning attributed to falls and falls prevention; and the provision of falls prevention information.
• Identify the context for the PLWD and their caregiver, including the current level of dementia severity; function; activity level; self-efficacy; and caregiver burden.
• Identify individual risk factors for falls for the person living with dementia, and readiness to change behaviour for these risk factors.
• Present options, facilitate decision-making and support behaviour change to address individual risk factors for the person living with dementia.
• Evaluate change in falls rate; falls risk; self-efficacy for the person living with dementia; and carer burden; and engagement of caregiver.
• Examine factors associated withpositive change in readiness to change behaviour.
• Explore change in knowledge and understanding of falls prevention; causes and consequences of falls; and the factors related to adopting falls prevention strategies for PLWD and their caregivers.
• To identify barriers and facilitators for community care staff to implement falls prevention best practice for PLWD and their caregivers.
• Design a discussion tool for use by community care health professionals to address individual falls risk factors for PLWD and their caregivers.
Conceptual framework
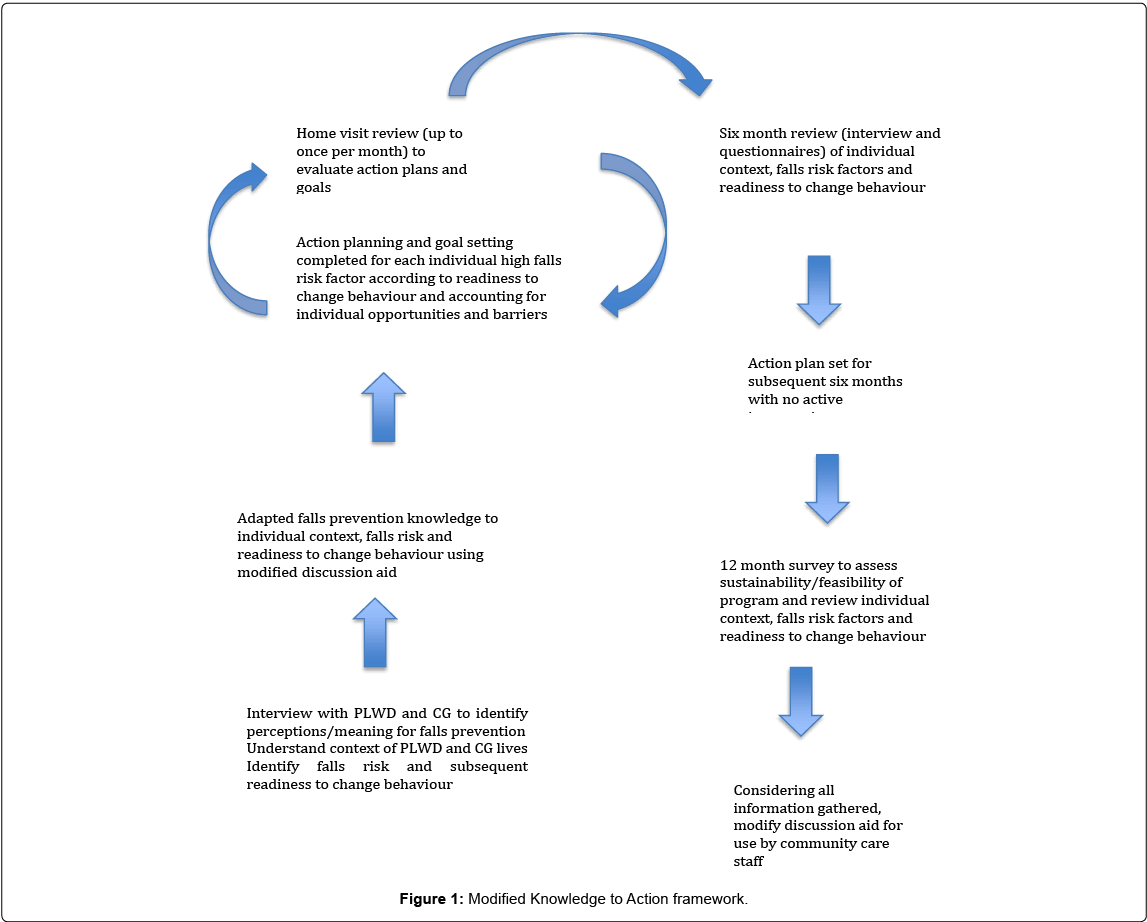
The last several years has seen an international call for a prioritisation of translational research, forgood research to be clearly understood, reach those who most need it, and be deemed useful and valuable by research end-users [14]. In this study, a knowledge translation theoretical framework, supported by several behavioural theories, is drawn upon to understand the complex phenomenon of translating falls prevention knowledge for PLWD. The Knowledge to Action framework [15] will beused as an over-arching framework. This framework characterises knowledge translation as a complex and dynamic process, commencing with knowledge creation and followed by action cycles in which attempts are made to utilise and implement knowledge, allowing key players to be included in a cyclical, collaborative process [15] (Figure 1). More commonly, this framework has been applied to move research evidence into clinical practice, and used to plan and evaluate knowledge translation strategies [16]. However, the authors believe it also has value in guiding individual behaviour change. The Knowledge to Action framework will be applied in a novel way; for improvements in clinical practice of community care professionals (Table 1) and for changing behaviours among individual PLWD and their caregivers (Table 2). To apply this framework in these complex environments, the researcher will place herself as a “knowledge broker”, as someone who is able to bring people together, help them build relationships, uncover need, and share ideas and evidence [14], in this case with the goal of communicating falls prevention knowledge.Several other theories will also be drawn upon to effectively apply the Knowledge to Action Framework.
| Knowledge to Action Framework component | Action research process for community care professionals |
|---|---|
| Identify the problem | Informal discussions with community care management and review of the literature |
| Adapt knowledge to local context | First action research session to understand the context for community care health professionals; and their role within the organisation (care managers, assessment officers, and direct care workers) |
| Identifying barriers to knowledge use | Subsequent action research sessions to identify the barriers and strengths within individuals and the organisation from which to develop a plan of action/change |
| Select, tailor, implement intervention | After three action research sessions, the community care professionals decide upon an action plan to implement over a 3-4 month period to address specific concerns regarding falls prevention for PLWD |
| Monitor knowledge use | Monitor progress of the action plan via email as needed |
| Evaluate outcomes/sustain knowledge use | The final action research session will encourage community care professionals to reflect on their action plan over the last 3-4 months, the challenges and the successes with a focus on how these changes can be sustained. |
Table 1: Components of the Knowledge to Action Framework for the intervention with community care professionals.
| Knowledge to Action Framework component | Intervention with PLWD and their caregiver |
|---|---|
| Identify the problem | A gap in the research was identified via the systematic review |
| Adapt knowledge to local context | Local context will be identified through an interview with PWD and caregiver – to understand falls and falls prevention from their perspective, in the context of their lives and their homes |
| Identifying barriers to knowledge use | Through the initial interview and questionnaires to understand falls risk, functional capacity, dementia severity, activity level, self-efficacy, caregiver burden. |
| Select, tailor, implement intervention | High falls risk factors will be identified through the FROP-Com questionnaire, with each risk factor being identified for participant’s readiness to change a given behavior using Prochaska’s stages of change model. |
| Monitor knowledge use | Up to six home visits will be conducted over 6 months, utilizing strategies to move participants through the stages of change for each high falls risk factor. Goal setting is used at each visit. |
| Evaluate outcomes | Evaluation of individual goals is conducted at each home visit. At 6 months an interview is conducted; a repeat of baseline questionnaires; a review of adherence to strategies; and an action plan for the following 6 months established. |
| Sustain knowledge use | Participants do not have any active intervention between 6 and 12 months of the intervention. A survey will be conducted at 12 months to establish feasibility and sustainability of the intervention, and factors influencing these. |
Table 2: Components of the Knowledge to Action Framework for the intervention with PLWD and their caregiver.
Achieving behaviour change is a considerable challenge in the falls prevention area [5] and likely to be an even greater challengewith PLWD. To understand the readiness for PLWD and their caregiver to change behaviourtheTrans theoretical Model of Behaviour Change will be applied [17]. This model will be adapted for use by caregivers and the person living with dementia for individually identified falls risk factors, with the dyad beingassessed as being in one of four stages of change for adopting new behaviours for each falls risk factor (pre-contemplation, contemplation, preparation through to action).
Goal setting theory is used to drive the action plans for PLWD and their caregivers for each selected falls risk factor, with the intention of moving individuals progressively through the stages of behaviour change. The goals are intended to be directive; energise; encourage persistence; discover new strategies and draw upon existing knowledge and prior learning [18]. Social cognitive theory of self-efficacy [19] has relevance here with task-specific confidence affecting the type of goal set; commitment to the goal; and the ability to find and use strategies to achieve the goal [18].
Knowledge translation within a community care setting is dependent upon capturing the tacit and explicit wisdom within individuals and their broader organisation, engaging the end-users, to customise a feasible and sustainable plan of action [14]. Communitybased participatory research (CBPR) is a valuable methodto be used for the translation of knowledge among community care health professionals, encouraging collaborative, equitable partnerships, capacity building and a focus on local relevance [20].
Methods
Design
This study will use a mixed-method design, drawing on the theories and frameworks discusses above,with two components investigating fall prevention knowledge translation for: (i) PLWD and their caregivers (Study 1); and (ii) staff of community care agencies providing support to PLWD and their caregivers (Study 2).
Setting
For Study 1 the setting will be the home of the person living with dementia, throughout metropolitan Melbourne and regional Victoria.
For Study 2 the setting will be a convenient location for community care staff.
Participants: Selection and Recruitment
This study will recruit 40 PLWD and their caregivers (Study 1) and up to eight staff from community care agencies in each CBPR group (Study 2).
Inclusion criteria include:
• Aged over 18 years with reasonable proficiency in spoken and written English (Study 1 and 2)
• A diagnosis of dementia (any type) made by a medical doctor (Study 1)
• Presence of an informal caregiver(unpaid, other than carer pension), who provides assistance with core activities of daily living (not required to be co-habiting, but must visit at least two days per week) (Study 1)
• An interest in falls prevention and a willingness to participate in the action research process(Study 2)
For Study 1, PLWD and their caregiverswill be recruited through participating community care agencies. Case managers and assessment officers will discuss the study with potential participants and determine their initial interest. In addition community events and support groups; snowballing techniques; personal and professional contacts; newspaper/newsletter advertisements; and known volunteer databases will be used for recruitment.
Participants in Study 2 will be staff working in community care agenciesthat provide support and care for PLWD and their caregivers. Agencies selected to participate will have an interest in falls prevention and a willingness to participate in the action research process. Recruitment will be through interested community care agencies known to the study team in metropolitan Melbourne and regional Victoria. Participation by individual staff in agencies agreeing to be involved will be encouraged from a diverse range of staff (professional backgrounds, current role and years of experience), with management approaching all staff to ascertain interest.
Ethics
Ethics approval has been granted by the LaTrobe University Human Ethics Committee (HREC 12-017).Prior to participation, participants in Study 1 and 2 will be given a Participant Information and asked to sign a Consent Form.
Informed consent will be gained from the PLWD if deemed competent, or alternatively,from the person responsible.The principal researcher (CM, an experienced allied health clinician), in accordance with recommendations from the Dementia Collaborative Research Centre(http://www.dementia.unsw.edu.au/), will judge competence. The researcher will determine whether the person with dementia:
• Understands the nature of the research and their participation in the research;
• Appreciates the consequence of their participation;
• Shows the ability to consider alternatives including the option to not participate; and
• Shows the ability to make a reasoned choice.
PLWD have varying levels of ability to retain information and make informed decisions (often fluctuating within the one individual). To continue to ensure that PLWD fully understand the nature of the research, acknowledging that dementia is an illness of progressive cognitive decline, those who initially sign their own consent form will be asked to sign again after three months.
Assessment and outcome measures
The following outcome measures will be collected at the baseline assessment with PLWD and their caregivers:
• Demographic details including age; gender; ethnicity; education level; marital status; living/caring arrangements; type, duration and severity of dementia; current health problems; and services used;
Falls risk assessment using the Falls Risk for Older Person – Community (FROP-Com) questionnaire [21], giving a total falls risk score based on falls history (retrospective recall of falls in past 12 months), medications, medical conditions, sensory loss and communication, feet and footwear, cognitive status, continence, nutritional conditions, environment, functional behaviour, function, balance, and gait/physical activity. The questionnaire is administered in written or verbal format, taking approximately 20 minutes to complete.
Functional status assessed using the Alzheimer’s Disease Cooperative Study (ADCS) Activities of Daily Living Inventory [22], including instrumental activities of daily living. The responses are given by the informal caregiver, someone who spends at least 2 days per week with the person with dementia. It takes approximately 15 minutes to administer.
Dementia severity assessed with the Dementia Severity Rating Scale (DSRS) [23], a multiple-choice questionnaire to assess the mildest to the most severe level of Alzheimer’s disease and other dementias. It takes five minutes, assessing the major functional and cognitive domains.
Activity level assessed with the CHAMPS Activities Questionnaire for Older Adults [24]. This questionnaire collects information on various forms of physical activity, their frequency and duration. It was specifically designed for older adults and has been shown to be sensitive to change over time. It takes approximately 20 minutes to administer, with the caregiver able to verify answers.
Self-efficacy will be measured for the caregiver using the Generalized Self-Efficacy Scale [25], a scale designed to give a general sense of perceived self-efficacy in order to predict coping with daily stressors and adaptation following stressful events. Falls self-efficacy will be measured for the person living with dementia using the Iconographical Falls Efficacy Scale (Icon-FES) [26] - a scale used to measure fear of falling, using pictures to describe a range of activities and situations. It is scored on a 4-point scale from “not at all concerned” to “very concerned”. Both questionnaires take approximately 5 minutes to complete.
Caregiver burden will be assessed with the Zarit Carer Burden Interview [27], a 29-item questionnaire covering most frequently reported areas of concern including caregiver health, psychological well-being, finances, social life and the relationship between the caregiver and the person they are caring for.
A repeat of outcome measures 2 – 7 will beundertaken for PLWD and their caregivers at the six and 12-month assessments (Table 3).
| Outcome measures used | Whom completes outcome measures | When outcome measures are applied | ||||
|---|---|---|---|---|---|---|
| PLWD | CG | Baseline | Sessions 2-4 | 6 months | 12 months | |
| Demographic details | â?? | â?? | â?? | |||
| Falls risk for older people - community | â?? | â?? | â?? | â?? | ||
| Activities of Daily Living Inventory | â?? | â?? | â?? | â?? | ||
| Dementia Severity Rating Scale | â?? | â?? | â?? | â?? | ||
| CHAMPS Activities Questionnaire for Older Adults | â?? | â?? | â?? | â?? | ||
| Iconographical Falls Efficacy Scale | â?? | â?? | â?? | â?? | ||
| Generalized Self Efficacy Scale | â?? | â?? | â?? | â?? | ||
| Zarit Carer Burden Interview | â?? | â?? | â?? | â?? | ||
| Readiness to change behaviour questionnaire | â?? | â?? | â?? | |||
| Therapeutic Engagement Index | â?? | â?? | â?? | â?? | â?? | â?? |
| Ottawa Decision Aid | â?? | â?? | â?? | |||
Table 3: Outcome measures for PLWD and their caregiver (CG).
The following measures will be used during each subsequent home visit with PLWD and their caregivers to guide intervention:
Readiness to change behaviour questionnaire [17]. As there is currently no readiness to change behaviour classification for falls risk factors, the behavioural change categories were adapted from the transtheoretical model [17] and from another behavioural change study for older adults [28]. As rated by the researcher (based on clinical interaction during home visits), this is a single item, four-category response question.
• 1 = precontemplation indicated lack of knowledge regarding the risk factor, belief that nothing could be done or unwillingness to change
• 2 = contemplation indicated an acknowledgement of the risk factor for falls, were beginning to think about options for change, but not yet ready to take action
• 3 = preparation indicated participants were actively planning to take action for a risk factor in the coming month
• 4 = action indicated that participants were currently taking action regarding a risk factor
• 5 = maintenance indicated that participants were able to sustain the action over the second six months of the intervention
The Therapeutic Engagement Index [29] is a 14-item scale used by health professionals to assess the extent to which informal caregivers are engaged with an intervention, and will be administered at each visit. It consists of three inter-related components of openness, connectedness and involvement. Caregiver engagement scores are summed for each session and then across all sessions for a total score.
A modified version of the Ottawa Family Decision Guide (OFDG) [30] will be used to guide the intervention. It is a user-friendly tool offering a way of discussing the options for addressing falls risk factors, while accounting for the PLWD and their caregiver’s perspective of their knowledge, values, support and certainty surrounding their decision. This tool allows goal setting to occur at the conclusion of the decision making process, to assist with determining a prioritised course of action.
Intervention study design
Study 1 – Intervention with PLWD and their caregivers: Underpinning the intervention phase is the Knowledge to Action framework, with each component broadly addressed over twelve months (Table 2) [15]. In addition, goal setting and development of an action plan will address the cyclical (but often non-sequential) processfor each falls risk factor.
The intervention will consist of an initial interview and data collection session, followed by up to monthly home visits by the researcher over the subsequent 6 months, with follow-up assessments at 6 months and 12 months.
The first visit for the PLWD and their caregiver includes:
• A short semi-structured interview conducted together (audiotaped), with the option of speaking separately given to both the person living with dementia and their caregiver. Proactive communication will be used, allowing sufficient time to answer questions, check meaning and interpretation of comments.Interview questions will explore:
• causes and consequences of falls
• personal importance and meaning of falls and falls prevention, relative to other health problems
• falls prevention information they have been provided with in the past, including the usefulness of this information
• Questionnaires and assessments will be administered for the PLWD (falls risk, activity level, falls self-efficacy) and caregiver (dementia severity, activities of daily living for PLWD, carer burden, self-efficacy) (see Assessment and outcome measures). These will allow a profile to be developed and allow development of targeted falls prevention strategies for consideration for implementation.
The intervention will commence at the second home visit, conducted within 2-3 weeks of the first. This lag between visitswill allow the person with dementia and their caregiver to process the information discussed; consider any additional questions they may have; and take participant burden into account. It will also allow the researcher to review the interview data and assessment results, and to develop a plan for an individually tailored intervention to discuss with the person living with dementia and their caregiver.
The second home visit will include:
• Presentation of options for falls risk reductionthrough use of a discussion aid, based upon the falls risk assessment and intrapersonal and external factors identified in the interview. Changing behaviours for falls risk reduction may involve raising awareness, discussion of pros and cons of behaviour change, use of communication strategies and techniques relevant to the person living with dementia, extrinsic falls prevention strategies such as home modifications, referral to services, and/ or access to resources/information;
• Setting of goals/action plans according to the readiness to change behaviour and preferences of the person living with dementia and their caregiver for identified areas of falls risk; and
• Provision of a monthly falls diary on which to record any falls or near falls (including circumstances and consequences). Participants will be asked to send back the monthly diary in a reply-paid envelope, with the researcher making a phone call if the diary is not received within two weeks of the end of the month.
Subsequent home visits (up to four visits (monthly) in accordance with usual community care management practice) will include:
• Revisiting goals and action plans, and progress towards these, for identified falls risk factors
• Reinforcement and feedback of existing strategies and consideration of any new or additional strategies required
• A review of readiness to change behaviour and caregiver engagement for addressing an additional falls risk factor Adherence to agreed falls prevention strategies - adherence will be calculated as a proportion, the percentage of strategies in use compared with the total recommended strategies [31].
Two final home visits will be conducted in Study 1, at six months, and then 12 months post baseline assessment. The 6-month visit will include completion of another short semi-structured interview (similar to the baseline interview) and a repeat of baseline questionnaires. The interview will again involve the person living with dementia and the caregiver, and will ascertain the knowledge and understanding of falls prevention and their perceptions of involvement in care during the intervention, including the difficulties and opportunities they faced in changing falls prevention behaviours. This visit will also review the goals achieved, adherence to strategies and the plan for the following six months.
Between the 6-month and the 12-month visits there will be no active intervention. Falls data will continue to be collected over the 6-12 month period, with participants asked to keep sending in the monthly diary.
The 12-month visit will include:
o A repeat of the self-efficacy and falls risk questionnaires
o A review of goals achieved and adherence to recommended strategies
o A brief survey to considersustained participation with the recommended interventions.
Study 2 - Action research process with community care staff: A range of community care agency staff, including organisational managers, care managers, assessment officers, associated health professionals and direct care workers (up to eight participants in each group) will be invited to participate in an action research group. Four sessions (audiotaped with permission) of 1.5 hours sessions will be undertaken over a 6-month period.
Session 1: An explanation of the project and the purpose of action research will be provided; a ‘falls prevention knowledge’ survey undertaken; information about current evidence for falls prevention among PLWD will be shared by the researcher; and discussion commenced regarding challenges and opportunities that exist for preventing falls in PLWD through community care agencies.
Session 2 and 3 (notes of previous session provided to participants) will consist of progressively deeper exploration of context-specific issues and opportunities; and a decision made by end of session 3 for an acceptable, feasible and useful action/s for practice change to facilitate the translation of falls prevention for PLWD and their caregivers. The group will then aim to implement the identified actions over 3-4 months, monitoring and reviewing the process over that time.
Session 4: A process evaluation will be undertaken to identify the benefits and challenges and outcomes of implementing the action; the entire action research process; and sustainability of strategies to prevent falls in PLWD. A repeat of the ‘falls prevention knowledge’ survey will be undertaken.
Data analysis (Table 4)
| Research objective | Methods/tools used | Statistical analysis used |
|---|---|---|
| 1. Identify perceptions of PLWD and their caregivers of the causes and consequences of falls; the importance and meaning attributed to falls and falls prevention; and the provision of falls prevention information | Semi-structured interviews § Reflective journal § |
Thematic analysis using grounded theory approach |
| 2. Identify the context for the PLWD and their caregiver to understand the current level of dementia severity; function; activity level; self-efficacy; and caregiver burden. | Questionnaires: Demographic characteristics of CG and PLWD DSRS § (CG rated for PLWD) ADCS § (CG rated for PLWD) CHAMPS § (PLWD) Icon-FES § (PLWD) Generalised Self Efficacy Scale § (CG) Zarit Carer Burden Interview § (CG) |
Used to inform intervention phase, but not statistically analysed |
| 3. Identify individual risk factors for falls for the PLWD, and readiness to change behaviour for these risk factors | FROP-Com § (PLWD) Readiness to change behaviour questionnaire § |
Used to inform intervention phase, but not statistically analysed |
| 4. Present options, facilitate decision making and support behaviour change to address individual risk factors | Modified Ottawa decision aid Φ Goal setting and action plans Φ Readiness to change behaviour questionnaire Φ |
Used to inform intervention phase, but not statistically analysed |
| 5. Evaluate change in falls rate; falls risk; self-efficacy; carer burden; and engagement of the caregiver | Falls calendars recording a fall event FROP-Com ∞ â?¯ Generalised Self Efficacy Scale ∞ â?¯ (CG) Zarit Carer Burden Interview ∞ â?¯ (CG) Therapeutic Engagement Index Φ |
Calculate rate of falls per 1000 days Analysis of change over three time points using one-way ANOVA measures for each of these measures (F; df; p) Post-hoc pairwise comparisons between time-points (mean difference, 95% CI) |
| 6. Examine factors associated with readiness to change behaviour | Demographic characteristics of CG and PLWD § DSRS §∞ â?¯ (CG rated for PLWD) ADCS §∞ â?¯ (CG rated for PLWD) Generalised Self Efficacy Scale §∞ â?¯ (CG) Zarit Carer Burden Interview §∞ â?¯ (CG) Iconographical Falls Efficacy Scale (PLWD) §∞ â?¯ CHAMPS (PLWD) §∞ â?¯ Readiness to change behaviour questionnaire Φ Treatment measures considered:
|
The association between baseline characteristics and initial readiness to change a falls risk factor measured using multiple logistic regression analysis (adjusted odds ratio, 95% CI) Categorical identification of number of strategies used and goals successfully met (yes/no) (mean, 95% CI) Adherence calculated as a proportion measure, the percentage of strategies in use compared with total recommended strategies. Caregiver engagement scores are summed for each session and then across all sessions for a total score (mean, 95% CI) One-way ANOVA used to examine differences between treatment measures and readiness to change behaviour [F, df, p]. Post hoc pairwise comparisons between levels of behaviour change scale (mean difference, 95%CI) Chi square analysis for describing change in readiness from initial to final session |
| 7. Explore change in knowledge and understanding of falls prevention; causes and consequences of falls; and the factors related to adopting falls prevention strategies for PLWD and their caregivers | Semi-structured interview at 6 months ∞ Survey at 12 months â?¯ Falls calendar notes Φ Reflective journal Φ Case notes, goal setting and action plans recorded at each home visit Φ |
Thematic analysis of 6-month interview data, falls calendar notes, case notes, reflective journal and 12-month survey data |
| 8. Facilitate community care staff to identify their knowledge and implement falls prevention best practice for PLWD and their caregivers | Knowledge survey Action research process (audio-taped and notes taken) Development of a discussion/decision aid |
Thematic analysis of notes fed back into action research cycle, utilising principles of the Consolidated Framework for Implementation Research (see Trial Status section for more detail) |
Table 4: Linking data analysis to research objectives and methods/tools used.
Study 1: As this is an exploratory study, sample size is based upon achieving data saturation through the qualitative component.
Several analyses will be undertaken:
• Thematic analysis of qualitative data using grounded theory approach. The data will be constantly compared until categories emerge, supported by Nvivo software;
• calculation of falls rate / 1000 days for the 12 months preceding the initial assessment, and two subsequent six month followup periods;
• analysis of change over time (three time points – pre-, 6 months, 12 months) using one-way ANOVA for falls risk, self • analysis of change over time (three time points – pre-, 6 months, 12 months) using one-way ANOVA for falls risk, selfefficacy, carer burden and engagement (F, df, p; and post hoc pairwise comparisons – mean difference, 95% CI);
• logistic regression for the association between baseline characteristics and readiness to change (adjusted odds ratio, 95% CI);
• Chi square analysis to describe readiness to change behaviour between initial and final sessions;
• categorical identification of strategies and goals;
• adherence calculated as a proportion measure; and
• One-way ANOVA to examine differences between treatment measures (eg and readiness to change behaviour [F, df, p]. Post hoc pairwise comparisons between levels of behaviour change scale (mean difference, 95%CI)
Study 2: Formative and summative evaluation of the action research process
Synthesis of the data: At the completion of Study 1, a final discussion aid for addressing individual falls risk factors for PLWD will be developed. This discussion aid will build on the one used during the intervention and will include information gathered from PLWD and their caregivers during this exploratory study;information gathered during Study 2; and the accommodation of best practice dementia care. This discussion aid will assist health professionals to identify readiness to change behaviours; and address falls risk factors using the best available evidence according to the stage of readiness to change behaviour. It is anticipated the discussion aid will include awareness raising; communication strategies and techniques; resources and information; and options for referral.
At the completion of Study 2, the findings of the action research process will be disseminated throughout the participating community care agencies. Community care staff will be invited to attend a presentation and discussion forum of the findings of the action research process, and the study more broadly.
Discussion
The area of translating falls prevention knowledge to PLWD and their caregivers is currently not well understood. While strong Level I and Level II evidence for preventing falls among community-dwelling PLWD does not yet exist, it is imperative that health professionals working in the community develop an understanding of what may be best options to consider, working to reduce falls in this high-risk population.
This study offers the opportunity to explore how falls prevention strategies can be best adopted by PLWD and their caregivers, taking into account their individual needs, preferences and abilities. Health professionals may suggest falls prevention strategies, but it is ultimately at the discretion of the person living with dementia and their caregiver to implement those strategies. The readiness of the dyad to change behaviour regarding falls risk factors is potentially an important component in ensuring the falls prevention message is delivered successfully, acknowledging that people may not be ready for substantial change, but consider smaller gains to be important [32].
This study allows for research to inform current falls prevention practice in the community, building on current practice of care management review of PLWD. Accounting for readiness to change behaviour is a new and novel approach for health professionals and will require a discussion aid to guide their practice. The discussion aid will assist community care staff in identifying falls risk factors and implement best practice strategies for PLWD. It is important, though, that this approach is carefully evaluated to guide replication in practice.
If falls prevention can become an integral part of the care management process, following an individualised plan of care, there are benefitsfor PLWD and potentially to effect change more broadly. There is the potential for a lowered falls rate for PLWD, reducing the injury and distress that this causes them and their families, the need for hospital admission and medical procedures and the likelihood that they will enter residential care. The broader potential societal benefits include the reduced costs of hospitalisation and residential aged care, as a result of falls and falls injury, together with a deeper understanding of personhood for the PLWD.
Competing Interests
The author(s) declare that they have no competing interests’
Authors’ Contributions
All authors participated in the design of the study. CM drafted the manuscript and all authors contributed to and approved the final manuscript
Acknowledgements
The authors thank the two community care agencies involved: Benetas and mecwacare.
References
- Wortmann M (2012) Dementia: a global health priority - highlights from an ADI and World Health Organization report. See comment in PubMed Commons below Alzheimers Res Ther 4: 40.
- (2012) Australian Institute of Health and Welfare: Dementia in Australia. Cat. No. AGE 70. In. Canberra: AIHW
- Dow B, Sparrow P, Moore K, Gaffy E, Yates I (2013) What do older Australians want?Australas J Ageing 32: 236-240.
- (2012) Australian Human Rights Commission: Respect and Choice: A Human Rights approach for ageing and health.
- Suttanon P, Hill KD, Said CM, Byrne KN, Dodd KJ (2012) Factors influencing commencement and adherence to a home-based balance exercise program for reducing risk of falls: perceptions of people with Alzheimer's disease and their caregivers. International Psychogeriatrics 24:1172-1182.
- Shaw FE1 (2007) Prevention of falls in older people with dementia. See comment in PubMed Commons below J Neural Transm 114: 1259-1264.
- Kallin K, Gustafson Y, Sandman P, Karlsson S (2005) Factors Associated With Falls Among Older, Cognitively Impaired People in Geriatric Care Settings: A Population-Based Study. The American Journal of Geriatric Psychiatry 13:501.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, et al. (2012) Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 9.
- Shaw FE, Bond J, Richardson D, Dawson P, Steen IN, et al. (2003) Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. British Medical Journal 326.
- Meyer C, Hill S, Dow B, Synnot A, Hill K (2013) Translating Falls Prevention Knowledge to Community-Dwelling Older PLWD: A Mixed-Method Systematic Review. See comment in PubMed Commons below Gerontologist .
- Taylor ME, Delbaere K, Close JCT, Lord SR (2012) Managing falls in older patients with cognitive impairment. Aging Health 8:573-588.
- Shields CM (2012) Critical Advocacy Research: An approach whose time has come. In: Critical Qualitative Research Reader. edn. Edited by Steinberg SR, Cannella GS. New York: Peter Lang Publishing.
- Moore TF, Hollett J (2003) Giving voice to persons living with dementia: the researcher's opportunities and challenges. See comment in PubMed Commons below NursSci Q 16: 163-167.
- Bennett G (2011) The knowledge translation toolkit: bridging the know-do gap: a resource for researchers. New Dehli, India: SAGE Publications.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, et al. (2006) Lost in knowledge translation: time for a map? ContinEduc Health Prof 26: 13-24.
- Ward V, House A, Hamer S (2009) Developing a framework for transferring knowledge into action: a thematic analysis of the literature. J Health Serv Res Policy 14: 156-164.
- Prochaska JO, DiClemente CC (1983) Stages and processes of self-change of smoking: toward an integrative model of change. J Consult ClinPsychol 51:390-395.
- Locke EA, Latham GP (2006) New directions in goal-setting theory. Current Directions in Psychological Science 15:265-268.
- Bandura A (1977) Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review 84:191-215.
- Israel BA, Eng E, Schulz AJ, Parker EA (2005) Introduction to methods in community-based participatory research for health. In: Methods in community-based participatory research for health. 2ndednSan Francisco
- Russell MA, Hill KD, Blackberry I, Day LM, Dharmage SC (2008) The reliability and predictive accuracy of the falls risk for older people in the community assessment (FROP-Com) tool. Age and Ageing 37:634-639.
- Galasko D, Bennett D, Sano M, Ernesto C, Thomas R, et al. (1997) An inventory to assess activities of daily living for clinical trials in Alzheimer's disease. The Alzheimer's Disease Cooperative Study. Alzheimer Disease & Associated Disorders 11:S33-39.
- Clark CM, Ewbank DC (1996) Performance of the Dementia Severity Rating Scale: A Caregiver Questionnaire for Rating Severity in Alzheimer Disease. Alzheimer Disease & Associated Disorders 10:31-39.
- Stewart A, Mills K, King A, Haskell W, Gillis D, et al. (2000) CHAMPS Physical Activity Questionnaire for Older Adults: outcomes for interventions. Medicine & Science in Sports & Exercise. 3: 1126-41.
- Schwarzer, R, & Jerusalem, M (1995)Generalized Self-Efficacy scale. In J. Weinman, S. Wright, & M. Johnston (eds) Measures in health psychology: A user’s portfolio. Causal and control beliefs, Windsor, UK.
- Delbaere K, Smith ST, Lord SR (2011) Development and initial validation of the Iconographical Falls Efficacy Scale. J Gerontol A BiolSci Med Sci 66: 674-680.
- Zarit SH, Reever KE, Bach-Peterson J (1980) Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 20: 649-655.
- McNulty MC, Johnson J, Poole JL, Winkle M (2003) Using the Trans theoretical model of change to implement home safety modifications with community-dwelling older adults: An exploratory study. Physical & Occupational Therapy in Geriatrics 21:53-66.
- Chee YK, Dennis MP, Gitlin LN (2005) Provider assessment of interactions with dementia caregivers: evaluation and application of the Therapeutic Engagement Index. Clinical Gerontologist 28:43-59.
- Ottawa Decision Support Tutorial
- Chee YK, Gitlin LN, Dennis MP, Hauck WW (2007) Predictors of adherence to a skill-building intervention in dementia caregivers. See comment in PubMed Commons below J GerontolABiolSci Med Sci 62: 673-678.
- Gitlin LN, Rose K (2013) Factors associated with caregiver readiness to use nonpharmacologic strategies to manage dementia-related behavioral symptoms. International Journal of Geriatric Psychiatry 29: 93-102
Relevant Topics
- Advanced Parkinson Treatment
- Advances in Alzheimers Therapy
- Alzheimers Medicine
- Alzheimers Products & Market Analysis
- Alzheimers Symptoms
- Degenerative Disorders
- Diagnostic Alzheimer
- Parkinson
- Parkinsonism Diagnosis
- Parkinsonism Gene Therapy
- Parkinsonism Stages and Treatment
- Stem cell Treatment Parkinson
Recommended Journals
Article Tools
Article Usage
- Total views: 14697
- [From(publication date):
March-2015 - Nov 22, 2024] - Breakdown by view type
- HTML page views : 10325
- PDF downloads : 4372