Case Report Open Access
Transjugular Liver Biopsy in a Multiple Myeloma Patient with Hepatomegaly, Portal Hypertension and Miliary Liver Lesions: A Case Report
Adrian J. Gonzalez-Aguirre1*, Oscar Lin2, Christina Cho3, Alexander M. Lesokhin3,4 and Majid Maybody11Radiology Department, Interventional Radiology Service, Memorial Sloan Kettering Cancer Center, York Avenue, New York, NY 10065, USA
2Pathology Department, Memorial Sloan Kettering Cancer Center, York Avenue, New York, NY 10065, USA
3Department of Medicine, Memorial Sloan Kettering Cancer Center, York Avenue, New York, NY 10065, USA
4Weill Department of Medicine, Weill Cornell Medical College, East 68th Street, Box 130, New York, NY 10065, USA
- *Corresponding Author:
- Adrian J. Gonzalez-Aguirre
Radiology Department
Interventional Radiology Service
Memorial Sloan Kettering Cancer Center
York Avenue, New York
NY 10065, USA
Tel: 1-646-593-0430
E-mail: gonzala2@mskcc.org;
Received date: January 22, 2016 Accepted date: February 02, 2016 Published date: February 10, 2016
Citation: Gonzalez-Aguirre AJ, Lin O, Cho C, Lesokhin AM, Maybody M (2016) Transjugular Liver Biopsy in a Multiple Myeloma Patient with Hepatomegaly, Portal Hypertension and “Miliary” Liver Lesions: A Case Report. J Gastrointest Dig Syst 6:390. doi:10.4172/2161-069X. 1000390
Copyright: © 2016 Gonzalez-Aguirre AJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
The present report describes a 50-year-old female recently diagnosed with multiple myeloma who presented with hepatosplenomegaly, miliary- type hyper enhancing liver tumors, and esophageal varices. We performed a transjugular liver biopsy when liver biopsy was requested to evaluate the miliary-type liver lesions. This was done to lower the risk of bleeding given the patient’s anemia and probable portal hypertension. This approach was successful in safely providing diagnostic samples for surgical pathology and flow cytometry to assess the nature of focal miliary liver lesions. It also proved portal hypertension.
Keywords
Multiple myeloma; Liver biopsy; Transjugular liver biopsy
Abbreviations
LB: Liver biopsy; TJLB: Transjugular liver biopsy; MM: Multiple myeloma
Introduction
Liver biopsy is a valuable diagnostic tool in the evaluation and management of patients with focal and non-focal liver disease. Liver biopsy has three major roles: 1) for diagnosis, 2) for assessment of prognosis (disease staging), and 3) to assist in making therapeutic decisions [1].
The present report describes a 50-year-old female recently diagnosed with multiple myeloma who presented with hepatosplenomegaly, miliary- type hyper enhancing liver tumors, and esophageal varices.
In a patient with focal liver lesions usually the first approach to obtain tissue diagnosis is a target biopsy, either percutaneously or EUS guided [2]. The purpose of this review is to present an unusual presentation of multiple myeloma and show that a non-target transjugular liver biopsy can offer a safe approach with decrease bleeding risk in this patient with multiple focal lesions.
Case Presentation
This report is compliant with the Health Insurance Portability and Accountability Act. A 50-year-old female with chronic anemia presented with fatigue, weakness, abdominal pain and distension. Initial workup at presentation showed hemoglobin of 5.4 g/dL, white blood cells 6.5 K/mcL and a platelet count of 147 K/mcL. A metabolic panel was notable for a protein gap with total protein 12.6 and albumin 3.2 g/dL, normal calcium at 8.6 mg/dL and normal creatinine of 0.9 mg/dL, , AST 66 U/L, ALT 47 U/L, total bilirubin 1.1 mg/dL, and alkaline phosphatase 130 U/L. LDH was elevated at 513 U/L.
Bone marrow showed 33% IgG kappa-restricted plasma cells, and serum free light chain (FLC) assay detected a kappa LC concentration of 404 mg/L, lambda 1.5 mg/L, and a kappa/lambda ratio of 269.47. Staging workup revealed numerous osteolytic lesions. These were all consistent with a working diagnosis of active multiple myeloma.
In addition, CT of the abdomen obtained for evaluation of the patient’s abdominal pain and distention revealed hepatomegaly (22.5 cm) and innumerable “miliary” enhancing nodules (Figure 1). Splenomegaly, gastroesophageal varices, and ascites were also seen.
A liver biopsy was requested to confirm that these liver findings represented involvement by the patient’s MM. After taking into account the uncommon presentation of the patient, a decision was made to perform a transjugular liver biopsy using a Liver Access and Biopsy Needle Set (Cook Medical, Bloomington, IN USA). The patient was transfused with two units of packed red blood cells before the biopsy.
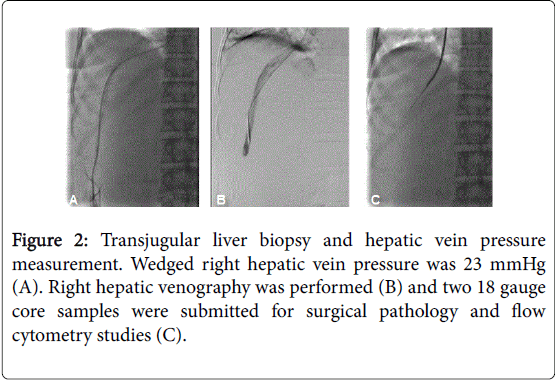
Wedged hepatic vein pressure was 23 mmHg. Two 18 gauge core samples were submitted for surgical pathology and flow cytometry studies (Figure 2).
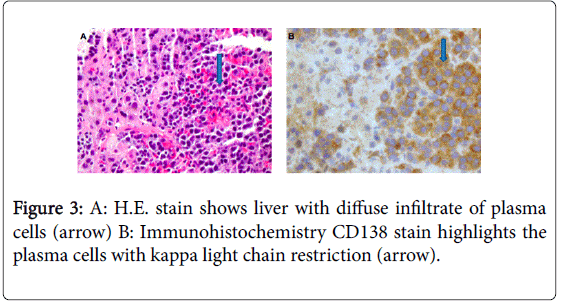
Surgical pathology (Figure 3) showed liver parenchyma with extensive involvement by a plasma cell neoplasm. Immunohistochemistry CD138 stain highlighted the plasma cells with kappa light chain restriction. A Congo stain was negative for amyloid.
Flow cytometry studies revealed an abnormal plasma cell population having abnormal expression of CD19 (absent), CD20, CD45 (absent), CD117 (bright), CD138 (partial) and monoclonal kappa cytoplasmic light chain restriction; with normal expression of CD38; and without CD56 expression.
Discussion
Extramedullary disease (EMD) is present in 15-20% of patients with MM. Of these, 21% involve the liver at the time of diagnosis. Patients with EMD have shorter progression-free and overall survival [3]. Liver involvement in MM can be in the form of light chain deposition disease, plasmacytoma (focal lesions composed of clonal plasma cells), amyloidosis, or a diffuse infiltrative pattern [4]. The clinical presentation of liver involvement in MM can range from asymptomatic to liver failure.
Most patients present with a diffuse form with associated hepatomegaly. Hepatic plasmacytomas are uncommon [5], to our knowledge there are 14 cases reported with focal liver lesions reported in the literature [6-19], of these 10 presented with multiple liver lesions and 4 with solitary lesions. Our patient presented with multiple hypervascular liver lesions (plasmacytomas) and hepatomegaly (diffuse involvement). Frequent tumor-associated causes of portal hypertension include portal vein thrombosis (pre-hepatic) and Budd- Chiari syndrome (post-hepatic), but this case illustrates that hepatic portal hypertension can also develop from infiltration of the sinusoidal and periportal space by hematologic diseases.
Patients with manifestations of portal hypertension have portal involvement on histologic section examination [5], and diagnosis requires histologic confirmation. Of the 14 cases reported in the literature 9 where biopsied under ultrasound guidance, 2 under CT guidance, 1 was biopsied during an exploratory laparoscopy and in 2 reports there is no clear description of the sampling technique used [6-19].
Liver biopsy is considered an overall safe procedure. Pain and vasovagal episodes are the most common minor complications. Bleeding is the most common reported major complication. Death is uncommon but has been reported in 0 to 0.33% [20-22]. In patients with chronic liver disease, the most common severe complication is bleeding, reported in 1.06% of this population. Multivariate analysis of a large cohort of liver biopsies in high-risk patients showed that 90% of patients with bleeding complications had esophageal varices and 60% had platelets less than 60,000, common findings in patients with portal hypertension. Authors from this cohort study suggest that by avoiding percutaneous biopsy in this population there will a 25% reduction in bleeding complications while eliminating only 2.8% of their biopsies (77/2740) [23].
Transjugular biopsy has been used as the standard for liver sampling in high-risk patients, particularly in patients with coagulopathies or thrombocytopenia who require non focal biopsy of the liver parenchyma. Major complications in this group after transjugular liver biopsy have been reported to be 0.5% [24]
Mindful evaluation of patient characteristics and preprocedure risk assessment should be undertaken before selection of the liver sampling method. Our patient presented with focal tumors, but the presence of hepatomegaly and the miliary pattern of enhancing lesions suggested diffuse involvement, and the presence of esophageal varices and splenomegaly raise the possibility of portal hypertension. Transjugular liver biopsy represented the best way to approach this patient, based on three main points: 1) diffuse liver involvement despite focal lesions, 2) access for portal venous pressure gradient measurement, and 3) safety in a patient with significant chronic anemia and possible portal hypertension.
Although transjugular liver biopsy is usually considered for nonfocal processes in high-risk patients, this case shows its applicability in diffuse focal “miliary” lesions when the risk of bleeding from a percutaneous biopsy is high. Physicians performing these procedures should take into consideration the options for liver sampling in order to provide patients with the best diagnostic yield at the lowest possible risk.
References
- Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD; American Association for the Study of Liver Diseases (2009) Liver biopsy. Hepatology 49: 1017-1044.
- Chhieng DC, Jhala D, Jhala N, Eltoum I, Chen VK, et al. (2002) Endoscopic ultrasound-guided fine-needle aspiration biopsy: a study of 103 cases. Cancer 96: 232-239.
- Usmani SZ, Heuck C, Mitchell A, Szymonifka J, Nair B, et al. (2012) Extramedullary disease portends poor prognosis in multiple myeloma and is over-represented in high-risk disease even in the era of novel agents. Haematologica 97: 1761-1767.
- Rahhal FE, Schade RR, Nayak A, Coleman TA (2009) Hepatic failure caused by plasma cell infiltration in multiple myeloma. World J Gastroenterol 15: 2038-2040.
- Perez-Soler R, Esteban R, Allende E, Tornos Salomo C, Julia A, et al. (1985) Liver involvement in multiple myeloma. Am J Hematol 20: 25-29.
- Huang H, Bazerbachi F, Mesa H, Gupta P (2015) Asymptomatic Multiple Myeloma Presenting as a Nodular Hepatic Lesion: A Case Report and Review of the Literature. Ochsner J 15: 457-467.
- Thiruvengadam R, Penetrante RB, Goolsby HJ, Silk YN, Bernstein ZP (1990) Multiple myeloma presenting as space-occupying lesions of the liver. Cancer 65: 2784-2786.
- Nguyen BD, Dash N, Lupetin AR (1992) MR imaging of hepatic plasmacytoma: a case report. Clin Imaging 16: 98-101.
- Caturelli E, Squillante MM, Castelvetere M, Falcone A, Musto P (1993) Myelomatous nodular lesions of the liver: diagnosis by ultrasound-guided fine-needle biopsy. J Clin Ultrasound 21: 133-137.
- Curtis JM, Pellegrini V, Tappin JA (1995) Case report: multiple myeloma--a rare presentation. Clin Radiol 50: 63-64.
- Kelekis NL, Semelka RC, Warshauer DM, Sallah S (1997) Nodular liver involvement in light chain multiple myeloma: appearance on US and MRI. Clin Imaging 21: 207-209.
- Chemlal K, Couvelard A, Grange MJ, Marmuse JP, Charneau C, et al. (1999) Nodular lesions of the liver revealing multiple myeloma. Leuk Lymphoma 33: 389-392.
- Fernandez-Flores A, Fortes J, Smucler A, Orduña M, Pol A (2003) Involvement of the liver by multiple myeloma as nodular lesions: a case diagnosed by fine-needle aspiration and immunocytochemistry. Diagn Cytopathol 29: 280-282.
- Arebi N, Patel B, Aqel NM, Pitcher MC (2004) IgA multiple myeloma presenting as non-obstructive jaundice. Postgrad Med J 80: 489-490.
- del Giglio A, Weinschenker P, Manhani AR, Carbonell AL, Mitteldorf CA (2005) Hepatic plasmacytosis as a manifestation of relapse in multiple myeloma treated with thalidomide. South Med J 98: 238-240.
- Invernizzi R, Maffè GC, Travaglino E, Pagani E, Pieresca C (2007) Nodular lesions of the liver in multiple myeloma. Haematologica 92: e81.
- Wu XN, Zhao XY, Jia JD (2009) Nodular liver lesions involving multiple myeloma: a case report and literature review. World J Gastroenterol 15: 1014-1017.
- Dhakal A, Chandra A (2013) A multiple myeloma patient presenting with multiple hepatic masses. J Med Cases 4: 673-675.
- Pal S, Chattopadhyay B, Chatterjee A, Bhattacharya B (2014) Lambda light chain myeloma presenting as nodular hepatic lesion: a clinical rarity. J Cancer Res Ther 10: 191-193.
- Cadranel JF1 Rufat P, Degos F (2000) Practices of liver biopsy in France: results of a prospective nationwide survey. For the Group of Epidemiology of the French Association for the Study of the Liver (AFEF). Hepatology 32: 477-481.
- van der Poorten D, Kwok A, Lam T, Ridley L, Jones DB, et al. (2006) Twenty-year audit of percutaneous liver biopsy in a major Australian teaching hospital. Intern Med J 36: 692-699.
- Thampanitchawong P, Piratvisuth T (1999) Liver biopsy:complications and risk factors. World J Gastroenterol 5: 301-304.
- Seeff LB, Everson GT, Morgan TR, Curto TM, Lee WM, et al. (2010) Complication rate of percutaneous liver biopsies among persons with advanced chronic liver disease in the HALT-C trial. Clin Gastroenterol Hepatol 8: 877-883.
- Kalambokis G, Manousou P, Vibhakorn S, Marelli L, Cholongitas E, et al. (2007) Transjugular liver biopsy--indications, adequacy, quality of specimens, and complications--a systematic review. J Hepatol 47: 284-294.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12933
- [From(publication date):
February-2016 - Feb 01, 2025] - Breakdown by view type
- HTML page views : 12185
- PDF downloads : 748