Case Report Open Access
Transepitheial High Fluence Crossliniking for Keratoconus
Amin ZY1* and Pinelli R21Ophthalmologist and Refractive Surgeon of Dr Yazan Zahran Eye Clinic, Amman, Jordan
2Scientific Director of Istituto Laser Microchirurgia Oculare, Brescia, Italy
- *Corresponding Author:
- Dr. Zahran Yazan Amin
Ophthalmologist & Refractive Surgeon of Dr Yazan Zahran Eye Clinic
Amman, Jordan, Italy
Tel: 00962796078785
E-mail: yazanr@hotmail.com
Received date: July 26, 2014; Accepted date: August 4, 2014; Published date: August 6, 2014
Citation: Amin ZY, Pinelli R (2014) Transepitheial High Fluence Crossliniking for Keratoconus. Microinflammation 1:105 doi: 10.4172/2381-8727.1000105
Copyright: 2014 Amin ZY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at International Journal of Inflammation, Cancer and Integrative Therapy
Abstract
Purpose: To evaluate the efficacy and safety of Transepitheial crosslinking for halting the progression of keratoconus.
Methods: Uncorrected and corrected visual acuity, simulated keratometry, corneal topography and pachmetry (CSO Italy) data were evaluated at baseline and at 5 months and one year after bilateral Transepithelial crosslinking using Paracel and KCL device Avedro.
Results: The keratometry and UCVA, BCVA at the baseline and after 5 months, one year of follow-up was stable and even improved with time.
Conclusion: The Transepithelial Cross linking can be safely and effectively halt the progression of keratoconus as demonstrated by follow up. Keratoconus is a non-inflammatory conelike ectasia of the cornea, which is usually bilateral and progress over time with consequent central and paracentral thinning of the stroma and irregular astigmatism. The only known treatment for arresting the progression of the keratoconus is Collagen corneal crosslinking the two mainly widespread techniques for Crosslinking is EPI-ON, EPI-OFF. The main advantages of the Transepithelial crosslinking technique over the traditional technique that its pain free with no stromal edema with the possibility to treat both eyes at the same session plus the morphological advantages of reducing the rate of death of keratocytes and the number of endothelial cells. With the improvement of this technique it could be the standard treatment for keratoconic patients.
Case Report
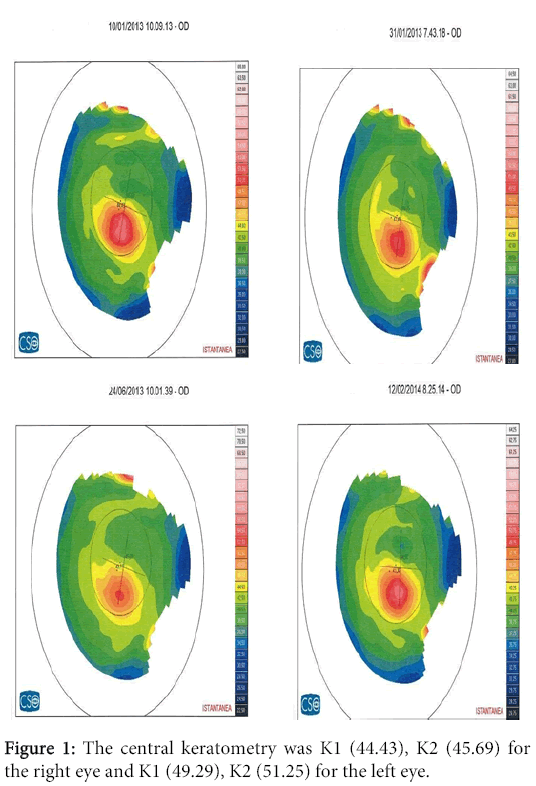
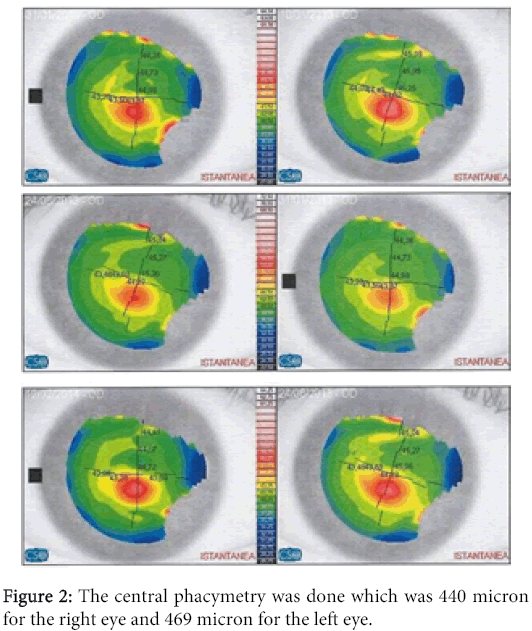
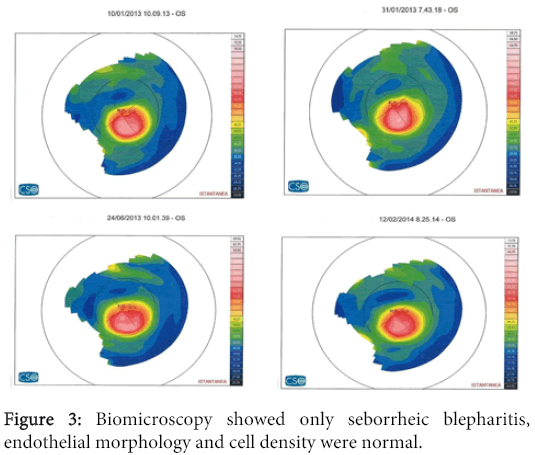
A 28 years old male patient with diagnosed Keratconus and already treated in the left eye with epi-on crosslinking in another clinic. He presented to ILMO seeking treatment in January 2013 at the time of examination his uncorrected visual acuity (UCVA) in the right is 20/32 best corrected (BCVA) to 20/25 with the following refraction (cyl -0.75 axis 70), left eye is 20/63 best corrected (BCVA) to 20/32 with the following refraction (sphere +1.25 cyl -2.5 axis 90). The corneal topography performed and showed inferior steeping with cone like configuration more in the left eye as shown in the following Figures 1-3. The central keratometry was K1 (44.43), K2 (45.69) for the right eye and K1 (49.29), K2 (51.25) for the left eye. The central phacymetry was done which was 440 micron for the right eye and 469 micron for the left eye. Biomicroscopy showed only seborrheic blepharitis, endothelial morphology and cell density were normal; retinal tomography was normal, tonometry was normal. The patient was then booked for TE cross linking which is the usual practice in our institute which take place at the end of January 2013. We perform osmotic crosslinking using Paracel riboflavin developed by Dr. Pinelli and produced by Avedro Watham, together with the KCL device also produced by the same firm. We allow a soaking time of 60" and do high fluence irradiation with 45 mW/cm2 for two minutes and forty seconds. The patient is checked immediately and at the end of the day for any eventual complications [1] which we thus far have never had. He is again checked the next morning and then programmed for sequential follow up except there are subjective necessities for earlier controls. The patient came back for follow-up after 5 months. during this follow-up the UCVA, BCVA of the right eye remained the same with the same refraction but the UCVA, BCVA of the left eye improved to 20/50, 25/25 respectively with the following refraction (+1.25 cyl -1.5 axis 90). The keratometry showed changes in the both eyes as follows OD K1 (43,48) K2 (44,75) OS K1 (47,22) K2 (49,65) the pachmetry remained the same and the cornea was clear. He was booked for another follow-up after one year from the procedure date. After one year the patient came back his UCVA, BVCA for his both eyes as the same last follow-up. The keratometry shows the following changes the OD K1 (44,11) K2 (45,49 ). OS K1(48.44) K2 (50.61) with clear cornea.
Results
The crosslinking is corneal strengthing procedure and the only known procedure that halt the progression of keratoconus its include saturate the cornea with riboflavin (vit b2) then expose the cornea for ultra-violate UVA rays which leads to increase the bonds between the collagen lamellecof the cornea that leads to strengthing the cornea. The crosslinking is done by two ways epithlium-off & epithlium-on (transepithlial route). The epithlium is the main barrier for riboflavin saturation of the cornea which is removed in the epi-off technique which leads to pain, loss of keratocytes, long recovery period. So we need a way which is free from these complications there come the transepithlial way which didn't include removal of the epithlium with same efficacy. In the furture this innovative procedure will become the standard procedure for crosslinking corneas e crosslinking is corneal strengthing procedure and the only known procedure that halt the progression of keratoconus its include saturate the cornea with riboflavin (vit b2) then expose the cornea for ultra-violate UVA rays which leads to increase the bonds between the collagen lamellecof the cornea that leads to strengthing the cornea. The crosslinking is done by two ways epithlium-off & epithlium-on (transepithlial route). The epithlium is the main barrier for riboflavin saturation of the cornea which is removed in the epi-off technique which leads to pain, loss of keratocytes, long recovery period. So we need a way which is free from these complications there come the transepithlial way which didn't include removal of the epithlium with same efficacy. In the furture this innovative procedure will become the standard procedure for crosslinking corneas. From the results of Visual acuity and kertometry of this Case we can see the improvement of the visual acuity plus the decrease and the stabilization of the kertometry of this patient over one year follow up.
Discussion
Corneal collagen cross linking is already a well-established clinical treatment which originally was indicated for ectatic corneal lesions such as keratoconus, pellucid marginal degeneration and ectasia post excimer laser refractive surgery [2,3]. The main streams in the treatment are, the Dresden protocol or epi-off with all the pros and cons [1,3] and the epi-on that has gained wide development in the years [2,4,5-8]. Debate still goes on as to whether the TE is effective and durable compared to the Dresden protocol. In our practice we use the Osmotic TE with paracel and KCL device and the results [6] have thus far been very good. There are also several other surfactant riboflavin solutions [8] on the market but still quite a good number of colleagues doing this procedure are skeptical as to the efficacy of the protocol. There is recent attention to the possible application of the technique to low power refractive errors [7] as well as keratitis. In the light of these and other possible indications we feel that an effort should be made to propose a valid able protocol that can lead to comparison of data in what could be another tool in refractive surgery some time later.
References
- Koller T, Mochen M, Seiler T (2009) Complications and failure after corneal crosslinking. J CataratactRefractSurg 38: 1358-1362.
- Filipello M, Stagni E, O'Brait D (2012) Transepithelial corneal cross linking bilateral study. J cataratact - refractive surgery 38: 283-291.
- Pinelli R (2007) Holcomb C3-R treatment opens new frontiers for keratoconus and corneal ectasia. Eye world 34-36.
- Wollensack G, Spoerl E, Seiler T(2003) Riboflavin/ultraviolet-A and collagen induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 135: 620-627.
- Caporossi A, Baioccchi S, Mazzotta C, Traversi C, Caporossi T, et al. (2006) Parasurgical therapy for keratoconus by riboflavin-ultraviolet type A rays induced crosslinking of corneal collagen: Preliminary refractive results in an Italian study. J Cataract RefractSurg 32: 837-45.
- Mastropasqua l, Nubile M, Calienno R, Lanzini M (2012) crosslinking cornealeeffetuatocontecnicatransepiteliale. Risultaticlinici, topograficiemorfologici.Otticafisiopatologica 97-102.
- Kanellopoulos AJ (2012) Long term results of a prospective randomised bilateral eye comparison trial of higher fluence shorter duration ultraviolet a radiation and riboflavin crosslinking for progressive keratoconus. Clinical Ophthalmol 6: 97-101.
- Kopen C, Wonters K, Mothysen D, Rozema J, Tassignon MJ (2012) Refractive and topografic results ofbenzalkonium chloride-assisted transepithelial crosslinking. J CataratactRefract Surgery 38: 1000-1005.
Relevant Topics
Recommended Journals
- Journal of Lung Cancer Diagnosis & Treatment
- Advances in Cancer Prevention
- Breast Cancer: Current Research
- Cancer Surgery
- Immunology: Current Research
- Current Trend in Gynecologic Oncology
- Journal of Cancer Diagnosis
- Journal of Gastrointestinal Cancer and Stromal Tumors
- Cervical Cancer: Open Access
- Journal of Mucosal Immunology Research
- Journal of Oncology Research and Treatment
- Journal of Orthopedic Oncology
- Journal of Prostate Cancer
- Research and Reviews on Pathogens
Article Tools
Article Usage
- Total views: 14400
- [From(publication date):
September-2014 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 10047
- PDF downloads : 4353