Research Article Open Access
Transcranial Direct Current Stimulation (tDCS) Therapy for Major Depressive Disorder in the HIV Population: A Safe, Effective Noninvasive Promising Treatment as Compared to Conventional Antidepressant Therapy
Saeed Ahmed1*, Mariyah Hussain2, Hooria Manzoor3, Venkatesh Sreeram4, Sara Dar5, Sharmeen Amin6, Rizwan Ahmed7, Mustafa Qureshi8, Satneet Singh9, Archana Rao Adikey10, Swati Sood11, Muhammad Taha Farooq12 and Tazeen Azfar131Nassau University Medical Center, USA
2Foundation University Medical College, Pakistan
3Saint Vincent’s Medical Center Transplant Research Institute, California
4Yale University PET Center, Connecticut
5FMH College of Medicine and Dentistry
6Jinnah Sindh Medical University, Pakistan
7Liaquat Medical and Dentistry College, Pakistan
8Brookdale University Hospital, NY, USA
10King County Hospital, NY, USA
11Dr.Rajendra Prasad Government Medical College, India
12Howard University Hospital, Washington DC, USA
13Baqai Medical University, Pakistan
- Corresponding Author:
- Saeed Ahmed, MD
Nassau University Medical Center, USA
Tel: 93298445854
E-mail: ahmedsaeedmd@gmail.com
Received date: August 25, 2015; Accepted date: September 14, 2015; Published date: September 20, 2015
Citation: Ahmed S, Hussain M, Manzoor H, Sreeram V, Dar S, et al. (2015) Transcranial Direct Current Stimulation (tDCS) Therapy for Major Depressive Disorder in the HIV Population: A Safe, Effective Noninvasive Promising Treatment as Compared to Conventional Antidepressant Therapy. J Addict Res Ther 6:241. doi:10.4172/2155-6105.1000241
Copyright: © 2015 Ahmed S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Major depressive disorder (MDD) is one of the most prevalent psychiatric disorders in the HIV-positive population. For long periods of time, MDD has been treated with conventional antidepressant therapy in these patients. Novel Antidepressant Therapy for Major Depression in HIV-infected adults is associated with various side effects such as sleep disturbance, nervousness, insomnia, weight loss, and sexual dysfunction that could lead to non-adherence to antiretroviral therapy. To uphold compliance and prevent patients from serious adverse effects of antidepressant therapy; emerging noninvasive innovative transcranial direct current stimulation (tDCS) could serve as a better alternative. tDCS has shown promising results; it is an effective, safe therapeutic strategy with an immediate onset of action as compared to conventional SSRI therapy. The application of tDCS is an easy one and the device for conducting this treatment modality is highly portable. Along with its convenient application, subjects who have been treated with tDCS in study settings, found it tolerable with minimum discomfort and without developing chronic and profound adverse effects. The role of transcranial direct current stimulation therapy is not limited to addressing solely the depressive component in the MDD population; however, it could be critical in assisting these patients by combating their co-morbidities of alcoholism and substance abuse by decreasing their cravings. Furthermore, tDCS has proven itself in improving the cognition in this patient population. This paper will further review this innovative treatment option and will also suggest tDCS to be studied in larger clinical trials as it could serve a huge role in developing better understanding of patient experiences regarding its tolerability, safety, and efficacy. Similarly, it will also provide important evidence to clinicians for the development of better practices in this area.
Keywords
Depression; Neurostimulation; HIV; Substance abuse; Public health
Introduction
HIV – A major global burden
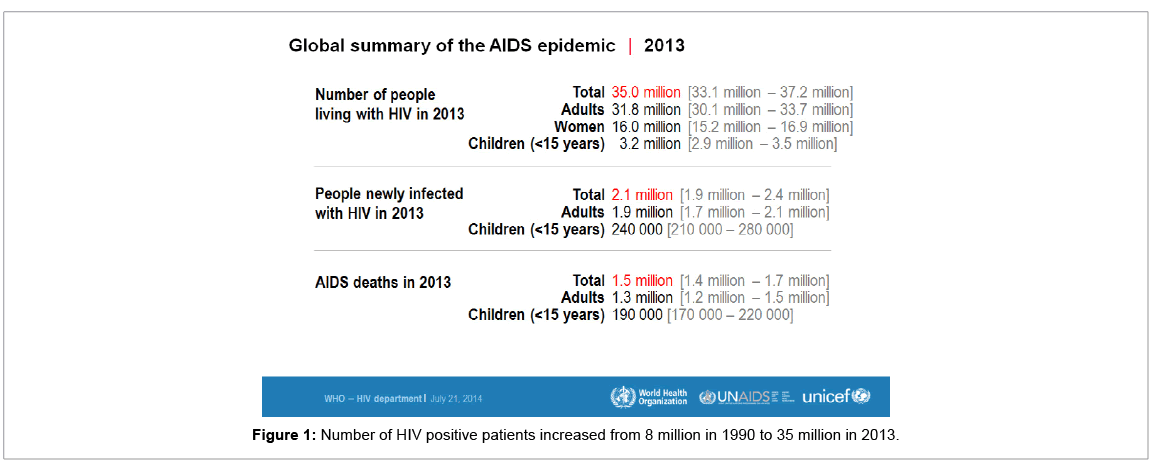
The Global Burden of Disease Study of 2010 [GBD 2010] was a comprehensive study to measure the magnitude of 291 different diseases and injuries from 1980 to 2010 amongst 187 countries. The disabilityadjusted life year [DALYs] was used as a measurement of disease burden. HIV/AIDS disease is the fifth leading cause of global DALY in 2010 and there were 35 [33.2-37.2] million people infected and living with HIV by the end of 2013 [1]. There were approximately1.5 million HIV deaths in 2013.It is the leading cause of DALY in age groups 20- 35 in females and 30-45 in males in contrast to other diseases which are seen in either very young or old age groups. The densely populated areas of HIV fall into four blocks: Eastern and Southern Africa, Central Africa, the Caribbean and Thailand.
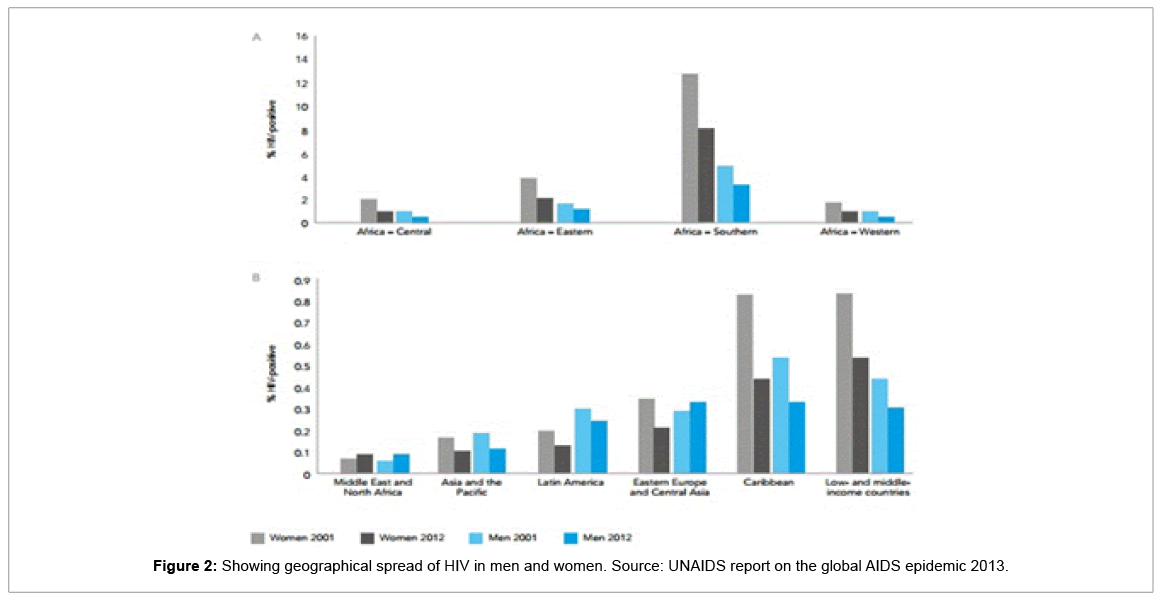
The first case of HIV was presented in 1981 and there have been substantially increased cases since then. The global trends show that HIV continues to rise rather at a fast pace. To understand its increasing trend, prevalence of HIV infection in the past three years is focused here. The number of HIV positive patients increased from 8 million in 1990 to 35 million in 2013 as shown in Figure 1. Out of these 35million HIV positive people, total numbers of adult women reported were 16 million and children reported were 3.2 million. Out of these patients, 1.5 million died due to this life threatening condition. The geographical spread of HIV is summarized in Figure 1. The geographical spread of HIV among men and women is depicted in Figure 2.
Causes of the rising HIV incidence
There are numerous reasons that lie behind this extravagant increase in burden and number of new cases. To name a few, the list includes lack of awareness, lack of prompt cure, and lack of accessibility to antiretroviral therapy. According to reports, only 37% of the total HIV population had access to antiretroviral treatment in 2013 [2,3]. It has also been documented that people in their reproductive age are more prone to get HIV infection than those who are at extremes of ages [3-5], hence presenting the likelihood of passing it on to their children through vertical transmission.
Preventive measures against HIV
Many measures have come under consideration in order to decrease the incidence of HIV which included use of condoms to counter sexual transmission, creating awareness regarding common causes of HIV, and preventive HIV vaccines which are under recent studies. These preventive measures have shown promising results in decreasing the incidence of HIV but there still remain several glitches that need to be handled to significantly decrease this disease [5].
Management of HIV
The treatment of HIV has been a major goal worldwide and several associations have been working on it since the past few years. Several treatment options have been proposed out of which antiretroviral therapy (ART) has consistently delivered most promising results so far. Combination ART reached 12.9 million HIV positive populations in 2013 and was increased by 5.6 million every year since 2010. This assisted significantly in decreasing the HIV burden globally [6].
HIV and depression – A strong association
HIV positive patients have a severely compromised immunity system that causes them to be frequently exposed to superimposed infections. These infections can be promptly dealt with medications. In addition to the superimposed infections, psychiatric disorders in HIV positive patients should also be widely recognized and considered. Major depressive disorder (MDD) is one of the most prevalent psychiatric disorders among HIV-positive population. The rationale behind this seems relatively simple; it emerges from a mental dilemma of suffering a chronic debilitating disease and undergoing its treatment. This might be one factor but several studies have shown that there are other major factors which contribute to MDD in this patient population, including: 1) Social isolation 2) Dealing with recurrent infections 3) Antiretroviral drugs.
Among these factors, anti-retroviral medications are considered to be the most common cause of depression in HIV patients who are receiving the therapy. Antiretroviral drugs have been widely known for causing several mood disorders. Depression is the most commonly recognized adverse effect of these medications. These drugs include interleukins, efavirenz, stavudine, zidovudine, interferons, zalcitabine and vinblastine (Table 1).
| Drugs | Adverse effects | |
|---|---|---|
| 1 | Interleukin | Depression, disorientation, confusion, and comma |
| 2 | Steroids | Mania or depression |
| 3 | Efavirenz (Sustiva) | Decreased concentration, depression, nervousness, nightmares |
| 4 | Zidovudine (Retrovir, AZT) | Mania, depression |
| 5 | Interferon | Neurasthenia fatigue syndrome, depression |
| 6 | Zalcitabine (Hivid) | Depression, cognitive impairment |
| 7 | Vinblastine | Depression, cognitive impairment |
| Source: HIV mental health treatment issues. | ||
Table 1: Antiretroviral drugs for HIV positive patients with their adverse effects.
When management of depression in HIV positive patients came under consideration, several options came under testing but conventional antidepressant therapy showed promising results [6]. However, these novel antidepressants also cause some severe adverse effects, summarized in Table 2, which makes HIV positive patients nonadherent to receive HIV medications. This issue has now grown into a serious dilemma since treating MDD in HIV positive patients further decreases patient’s compliance towards HIV medications [2,7,8]. Therefore, an alternative must be considered to counter MDD in HIV positive patients without causing serious side effects (Table 2).
| Drugs | Adverse effects | |
|---|---|---|
| 1 | SSRIs (Prozac, Paxil, Zoloft) | Increased GI activity, anorgasmia, akathisia, apathy, anxiety, and when toxic, a serotonin syndrome. |
| 2 | Bupropion (Wellbutrin) | Contraindicated in patients with unstable seizure disorder; multiple divided dosing. |
| 3 | Venlafaxine (Effexor) | Initial stimulant side effects may disturb some patients, may increase blood pressure in hypertensive; GI side effects (also common with antiretrovirals) |
| 4 | Trazodone (Desyrel) | May cause sedation in a.m. at 50-100 mg when taken at night; 1/7000 incidence of priapism. |
| 5 | Tricyclics | Weight gain, constipation, orthostatic hypotension, dry mouth, sedation. Can be lethal in overdose. |
| 6 | Hormones (testosterone, DHEA) | Off-label for treating depression, side effects with hormone treatment impact biological functions. |
| Source: HIV mental health treatment issues. | ||
Table 2: Conventional antidepressants to treat MDD in HIV positive patients and their side effects.
Transcranial direct current stimulation (tDCS) therapy
Transcranial Direct Current Stimulation (tDCS) is a new emerging technique that is non invasive. tDCS was introduced a few decades ago and showed promising results back then and hence was considered to be a state of art in 2008 [9,10]. It is a neuromodulatory method that has impact on the firing and excitability of the neuronal circuits of the brain [11,12]. Two electrodes are placed over the scalp to pass low voltage direct current usually 1 to 2 mA [13] which acts either to potentiate neuronal excitability via anodal stimulation or diminish neuronal firing via cathodal stimulation [14-16].
The mechanism of action of tDCS at cellular level is to modulate the resting membrane potential at a sub-threshold level [12]. This modulation leads to the development of modified N-methyl-Daspartate (NMDA) receptors, which are involved in neuroplasticity [17]. Neuroplasticity is the recognition of the compound dynamics of the central nervous system (CNS) connectivity [18]. Its role as the major physiological basis of adaptation of cognition and behavior and nature of a person has been well recognized. Pathological neuroplasticity has been recognized as the basis of many psychiatric disorders [18].
Some of the tDCS induced changes occur rapidly and are hence known as Intra-tDCS changes. Meanwhile, some of the effects occur later either as short-lived or long lasting effects [12] The intra-tDCS changes depend entirely on the activity of sodium and calcium channels and are probably generated by polarity dependent changes in resting membrane potential (RMP) [19]. The after effects are associated with increased protein synthesis in the neuronal circuit along with specific changes in the NMDA receptor [11,12].
Use of tDCS in the treatment of neuropsychiatric disorders
The effects of tDCS can be appreciated on the neuronal circuit involved in the mood associated neuronal networks [20] along with the neuronal circuitry associated with motor control, somatosensory pathways, visual pathways, and pathways associated with cognition [21,22].
Besides a high safety profile, affordability, and a simple approach; due to its effects on neuromodulation, tDCS is now increasingly being used to treat many neuropsychiatric disorders including mania, bipolar disorder, bipolar depression, mixed affective state, positive and negative symptoms of schizophrenia, childhood onset schizophrenia as well as visual and auditory hallucinations of schizophrenia [23-28].
tDCS has also shown to decrease the symptoms of tinnitus and is being widely used for the management of post stroke residual motor deficits, fibromyalgia, epilepsy, and Parkinson’s disease [18,21,22].
Cognitive improvement with the use of tDCS in mentally ill individuals
Cognitive impairment is a core component of many neuropsychiatric disorders and also serves as an epicenter affecting the quality of life of a person with a neuropsychiatric disease. Pathological alterations of neuroplasticity of brain are increasingly explored as pathophysiological foundation of diverse neuropsychiatric disorders. Non invasive brain stimulation techniques such as tDCS have been tested on stroke patients to recover and have also been tested on patients with Alzheimer’s [29,30] and Parkinsonism, where it increases recognition memory performance in Alzheimer’s patients and working memory in patients with Parkinsonism [31-33]. tDCS has been shown to enhance performance accuracy; it helps the brain to relearn through facilitating local brain activity and inhibiting the competing activity. Cortical excitability changes accompany motor learning. In a randomized controlled trial, it was observed that attention and working memory in patients with depression improved after a single session of active tDCS that was administered for 15 consecutive days [32]. Frontal tDCS has further shown to improve mood and alleviate feelings of sadness as an adjuvant treatment for hospitalized patients in severely drug resistant depression [33]. tDCS is not only a tool that increases performance by facilitating behavior but also fine tunes response by increasing signal to noise ratio; the same study showed that bifrontal tDCS in addition to the anti-depressant effects, presents with acute positive aspects on cognition.
Future studies that will combine the use of tDCS and cognitivebehavioral therapy to improve cognition in neuropsychiatric disorders will be able to further explore the role of tDCS in cognition improvement in mental illness.
Use of tDCS in the treatment of Major Depressive Disorder (MDD) in HIV positive patients
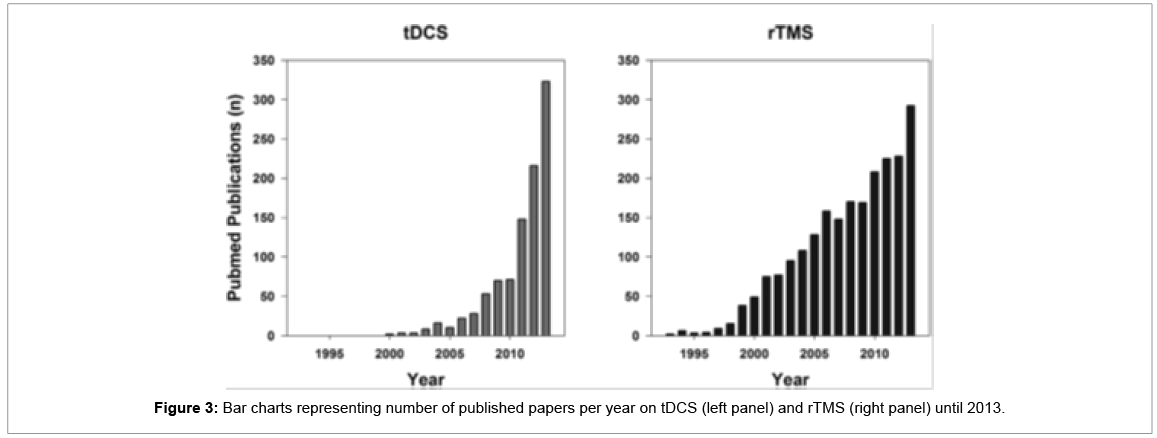
The most common clinical presentation of many neuropsychiatric conditions as well as many debilitating disorders like cancer and HIV is depression [34]. Depression in these circumstances is resistant to treatment by conventional antidepressants and is included in the category of Major Depressive Disorder (MDD) [33-35]. MDD occurs usually as a result of alterations to neural circuitry especially in the prefrontal cortex. tDCS is being increasingly used to manage medicationresistant depression [9]. It works by inducing changes in RMP (Resting Membrane Potential), spontaneous firing rates, and improving the synaptic strength as well as cerebral blood flow and metabolism [13,36]. A study demonstrated that when tDCS is given in combination with sertraline, it substantially increases the efficacy of both therapeutic modalities [37]. Several double-blinded, sham controlled studies have shown significant clinical improvement in patients with depression when they were exposed to anodal tDCS stimulation consecutively for five days, and when given for 15 consecutive days [32-38], this was also demonstrated in an open study performed on HIV patients who were suffering from depression [12]. tDCS can also be used in combination with other neurostimulatory techniques such as transcranial magnetic stimulation to increase their efficacy in the treatment of MDD. tDCS is most effective in the management of MDD when it is used in acute stages of the neuropsychiatric disorders [39,40]. As we have already focused on high prevalence of depression in HIV positive populations, when treatment of depression in this patient population is concerned, tDCS therapy has consistently proven itself as an effective modality. Studies conducted on tDCS have also failed to demonstrate profound adverse effects. On the other hand however, several studies have questioned its efficacy and have suggested further investigational studies on tDCS demanding more reliable evidences [16,39,41].The real benefit of using tDCS therapy, as an alternative to conventional antidepressant therapy, is to prevent the occurrence of adverse effects caused by medications and decrease the non-adherence of HIV patients towards antiretroviral drugs (Figure 3). The search was conducted on the PubMed database using the search terms “transcranial direct current stimulation” and “repetitive transcranial magnetic stimulation” [42].
Why conduct clinical research on tDCS?
Brunoni et al. proposed three main reasons that make it critical to further carry researches on tDCS. They identified that tDCS has a theoretical clinical basis because it can be used as a substitute to pharmacotherapy; especially in cases where people have failed medications, have exhibited poor tolerability, and have suffered serious adverse drug interactions. The second logistic centers around tDCS being an effective augmentative therapy in certain conditions, e.g., tDCS and pharmacotherapy combined for depression or chronic pain. This is also based on the rationale that tDCS is a noninvasive technique and has no proven chronic side effects, along with displaying synergistic effects due to its interaction with the resting membrane potential. Thirdly, tDCS is fairly economical. Thus, with further proven safety and effectiveness, it can play a huge role as a treatment in the developing countries [43]. Because of its inexpensiveness and its easy to build nature, there have been many videos uploaded on YouTube even by laymen who are demonstrating how to build and use this device.
Conclusion
Researchers should be encouraged to further systematically investigate tDCS in larger clinical trials to bring forward more reliable evidence in support of this effective treatment modality. This shall also assist in impacting the way the HIV population perceives tDCS as a therapy for their Major Depression. We need the patient population and the clinicians to recognize the worth of tDCS in managing this crucial yet ignored aspect of mental health issue that is widely prevailing among the HIV population. tDCS has so far managed a favorable safety profile, hence, there should be a better understanding of its tolerability, safety, and effectiveness. Clinicians need to be well informed about the treatment choices they can offer their patients when addressing their psychiatric issues. tDCS therapy holds a great potential to enhance improvements in managing Major Depressive Disorder in the HIV population, therefore, it should be encouraged and considered as an alternative, safe, and effective technique that will give us a positive approach in handling mental illness. With collective action to acknowledge and address the serious dilemma of depression, as well as commitment to safe and reliable interventions, combating the issue is within reach.
References
- Ortblad KF, Lozano R, Murray CJ (2013) The burden of HIV: Insights from the Global Burden of Disease Study 2010. AIDS 27: 2003-2017.
- Kaplan JE, Hamm TE, Forhan S, Hassani AS, Bang G, et al. (2015) The impact of HIV care and support interventions on key outcomes in low-and middle-income countries: A literature review—introduction. JAIDS Journal of Acquired Immune Deficiency Syndromes 68:S253-S6.
- Steinbrook R (2004) The AIDS epidemic in 2004. N Engl J Med 351: 115-117.
- World Health Organization. Global update on HIV treatment 2013: Results, impact and opportunities 2013.
- [No authors listed] (1995) UNAIDS: mission and roles. Glob AIDSnews 2-3.
- Joint United Nations Programme on HIV/AIDS U. Epidemiological slides – gap report 2014.
- Gonzalez JS, Batchelder AW, Psaros C, Safren SA (2011) Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. J Acquir Immune DeficSyndr 58: 181-187.
- Mehta S, Moore RD, Graham NM (1997) Potential factors affecting adherence with HIV therapy. AIDS 11: 1665-1670.
- Nitsche MA, Boggio PS, Fregni F, Pascual-Leone A (2009) Treatment of depression with transcranial direct current stimulation (tDCS): A review. Exp Neurol 219: 14-19.
- Berlim MT, Dias Neto V, Turecki G (2009) Transcranial direct current stimulation: A promising alternative for the treatment of major depression? Rev Bras Psiquiatr 31 Suppl 1: S34-38.
- Nitsche MA, Paulus W (2000) Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol 527 Pt 3: 633-639.
- Knotkova H, Rosedale M, Strauss SM, Horne J, Soto E, et al. (2012) Using transcranial direct current stimulation to treat depression in HIV-infected persons: The outcomes of a feasibility study. Frontiers in psychiatry 3:59.
- Arul-Anandam AP, Loo C (2009) Transcranial direct current stimulation: A new tool for the treatment of depression? J Affect Disord 117: 137-145.
- George MS, Rush AJ, Marangell LB, Sackeim HA, Brannan SK, et al. (2005) A one-year comparison of vagus nerve stimulation with treatment as usual for treatment-resistant depression. Biol Psychiatry 58: 364-373.
- Lang N, Siebner HR, Ward NS, Lee L, Nitsche MA, et al. (2005) How does transcranial DC stimulation of the primary motor cortex alter regional neuronal activity in the human brain? Eur J Neurosci 22: 495-504.
- Nitsche MA, Schauenburg A, Lang N, Liebetanz D, Exner C, et al. (2003) Facilitation of implicit motor learning by weak transcranial direct current stimulation of the primary motor cortex in the human. J Cogn Neurosci 15: 619-626.
- Antal A, Paulus W, Nitsche M (2009) Principle and mechanisms of transcranial direct current stimulation (tdcs). J Pain Manag 249-258.
- Kuo MF, Paulus W, Nitsche MA (2014) Therapeutic effects of non-invasive brain stimulation with direct currents (tDCS) in neuropsychiatric diseases. Neuroimage 85 Pt 3: 948-960.
- Liebetanz D, Nitsche MA, Tergau F, Paulus W (2002) Pharmacological approach to the mechanisms of transcranial DC-stimulation-induced after-effects of human motor cortex excitability. Brain 125: 2238-2247.
- Brunoni AR, Valiengo L, Zanao T, de Oliveira JF, Bensenor IM, et al. (2011) Manic psychosis after sertraline and transcranial direct-current stimulation. J Neuropsychiatry Clin Neurosci 23: E4-5.
- Been G, Ngo TT, Miller SM, Fitzgerald PB (2007) The use of tDCS and CVS as methods of non-invasive brain stimulation. Brain Res Rev 56: 346-361.
- Goto Y, Yang CR, Otani S (2010) Functional and dysfunctional synaptic plasticity in prefrontal cortex: Roles in psychiatric disorders. Biol Psychiatry 67: 199-207.
- Brunoni AR, Valiengo L, Baccaro A, Zanao TA, de Oliveira JF, et al. (2011) Sertraline vs. Electrical current therapy for treating depression clinical trial-select tdcs: Design, rationale and objectives.Contemp Clin Trials 32:90-98.
- Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, et al. (2008) Transcranial direct current stimulation: State of the art 2008. Brain Stimul 1: 206-223.
- Loo CK, Sachdev P, Martin D, Pigot M, Alonzo A, et al. (2010) A double-blind, sham-controlled trial of transcranial direct current stimulation for the treatment of depression. Int J Neuropsychopharmacol 13: 61-69.
- Shiozawa P, da Silva ME, Cordeiro Q, Fregni F, Brunoni AR (2013) Transcranial direct current stimulation (tDCS) for the treatment of persistent visual and auditory hallucinations in schizophrenia: a case study. Brain Stimul 6: 831-833.
- Priori A, Hallett M, Rothwell JC (2009) Repetitive transcranial magnetic stimulation or transcranial direct current stimulation? Brain Stimul 2: 241-245.
- Nawani H, Kalmady SV, Bose A, Shivakumar V, Rakesh G, et al. (2014) Neural basis of tDCS effects on auditory verbal hallucinations in schizophrenia: A case report evidence for cortical neuroplasticity modulation. J ECT 30: e2-4.
- Ferrucci R, Mameli F, Guidi I, Mrakic-Sposta S, Vergari M, et al. (2008) Transcranial direct current stimulation improves recognition memory in Alzheimer disease. Neurology 71: 493-498.
- Penolazzi B, Bergamaschi S, Pastore M, Villani D, Sartori G, et al. (2015) Transcranial direct current stimulation and cognitive training in the rehabilitation of Alzheimer disease: A case study. Neuropsychol Rehabil 25: 799-817.
- Boggio PS, Ferrucci R, Rigonatti SP, Covre P, Nitsche M, et al. (2006) Effects of transcranial direct current stimulation on working memory in patients with Parkinson's disease. J Neurol Sci 249: 31-38.
- Loo CK, Alonzo A, Martin D, Mitchell PB, Galvez V, et al. (2012) Transcranial direct current stimulation for depression: 3-week, randomised, sham-controlled trial. Br J Psychiatry 200: 52-59.
- Ferrucci R, Bortolomasi M, Vergari M, Tadini L, Salvoro B, et al. (2009) Transcranial direct current stimulation in severe, drug-resistant major depression. J Affect Disord 118: 215-219.
- Valiengo LC, Benseñor IM, Lotufo PA, FraguasJr R, Brunoni AR (2013) Transcranial direct current stimulation and repetitive transcranial magnetic stimulation in consultation-liaison psychiatry. Braz J Med Biol Res 46: 815-823.
- Dell'Osso B, Dobrea C, Arici C, Benatti B, Ferrucci R, et al. (2014) Augmentative transcranial direct current stimulation (tDCS) in poor responder depressed patients: a follow-up study. CNS Spectr 19: 347-354.
- Murphy DN, Boggio P, Fregni F (2009) Transcranial direct current stimulation as a therapeutic tool for the treatment of major depression: insights from past and recent clinical studies. Curr Opin Psychiatry 22: 306-311.
- Valiengo L, Benseñor IM, Goulart AC, Oliveira JF, Zanao TA, et al. (2013) The sertraline versus electrical current therapy for treating depression clinical study (select-tdcs): Results of the crossover and follow-up phases. Depress Anxiety 30:646-653.
- Boggio PS, Rigonatti SP, Ribeiro RB, Myczkowski ML, Nitsche MA, et al. (2008) A randomized, double-blind clinical trial on the efficacy of cortical direct current stimulation for the treatment of major depression. Int J Neuropsychopharmacol 11:249-254.
- Brunoni AR, Valiengo L, Baccaro A, Zanao TA, de Oliveira JF, et al. (2013) The sertraline vs. electrical current therapy for treating depression clinical study: Results from a factorial, randomized, controlled trial. JAMA psychiatry 70:383-391.
- Palm U, Keeser D, Blautzik J, Pogarell O, Ertl-Wagner B, et al. (2013) Prefrontal transcranial direct current stimulation (tdcs) changes negative symptoms and functional connectivity mri (fcmri) in a single case of treatment-resistant schizophrenia. Schizophr Res 150:583-585.
- Nitsche MA, Seeber A, Frommann K, Klein CC, Rochford C, et al. (2005) Modulating parameters of excitability during and after transcranial direct current stimulation of the human motor cortex. J Physiol 568: 291-303.
- Krishnan C, Santos L, Peterson MD, Ehinger M (2015) Safety of noninvasive brain stimulation in children and adolescents. Brain Stimul 8: 76-87.
- Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, et al. (2012) Clinical research with transcranial direct current stimulation (tDCS): Chall enges and future directions. Brain Stimul 5: 175-195.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 15559
- [From(publication date):
September-2015 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 10970
- PDF downloads : 4589