Research Article Open Access
Training in Laparoscopic Surgery in Latin America
Edmundo Dediós Orozco1* and Carlos Dediós La Madrid2
1CEPCEA President, Chief of the Surgery Department, Jorge Reategui Delgado Hospital II-EsSalud, Piura, Peru
2Chief of the Laparoscopic Surgery Laboratory, CEPCEA, Piura, Peru
- *Corresponding Author:
- Edmundo Dediós Orozco
CEPCEA President, Chief of the Surgery Department
Jorge Reategui Delgado Hospital, II-EsSalud, Piura, Peru
Tel: 073-969920022
Fax: 073-285210
E-mail: ed_dedios@hotmail.com
Receiving date: January 31, 2017; Accepted date: February 24, 2017; Published date: February 28, 2017
Citation: Dedios E, Dedios C (2017) Training in Laparoscopic Surgery in Latin America. J Gastrointest Dig Syst 7:489. doi: 10.4172/2161-069X.1000489
Copyright: © 2017 Dedios E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: The training of Residents and Surgeons in Laparoscopic Surgery in Latin America is performed in the OR (Operating Room) on the patient, which predisposes to the risk of many complications, both during learning as during the daily performance of this intervention.
Objective: To evaluate the efficiency of the basic training program in Laparoscopic surgery in the development of cognitive and motor dexterities and skills.
Methodology: CEPCEA (Center for Studies on Prevention and Correction of Abdominal Diseases) has developed a 5-day teaching system, based on the PBL (Problem-Based Learning) development of tests in manual skills on inanimate objects, biological and human tissue and permanent creation of easy to repeat tips, we combine the best of each continent: the American FLS (Fundamentals of Laparoscopic Surgery) Training, the Europeanoriginated Endotrainer and the Japanese KAIZEN. We took a pre-test and a practical post-test to the total cohort of trained surgeons during the period January-December 2016, tests which were based on time and on 20 theoretical questions with a value of 1 point per each correct answer. We used the SPSS v.21 as statistical software.
Results: The population tested consisted of 55 trainees from different Latin-American countries who attended in groups of 4 to 6 participants of general surgery (32), gynecology (11), urology (3), surgery oncology (3), pediatric surgery (1), and others (5) who, on admission, had a mean of peg transfer time of 189.6 seconds, which at the end of their practical training of 4 days was of 68.4 seconds; while the results of the pretest and theoretical posttest showed a media of 5.8 And 14.9 points respectively.
Conclusions: The CEPCEA teaching system is an efficient and necessary method for the development of manual and theoretical skills and dexterities in laparoscopic surgery in the various surgical specialties.
Keywords
Training in laparoscopy; Laparoscopy laboratory; Evaluation in laparoscopy
Introduction
Facing the rapid growth of laparoscopic surgical technology, adequate laboratory training is required, prior to acting in the operating room. The Learning Curve should take place in the laboratory, not in the patient's abdomen [1-3]. It is considered relevant to make an objective measurement of the trained student’s acquisition of skills and dexterities, after the implementation of a new training program with simulators with inanimate, virtual and animal models, prior to contact with the patients [4]. Likewise, in his research, Enciso [5] aims to evaluate the development of rookie surgeon’s skills through the implementation of the training program in basic laparoscopic surgery, as well as obtaining a subjective assessment of it. The learning of Laparoscopic Surgery is not fully standardized, nor is easily accessible. Laparoscopic Surgery learning programs are still incomplete and do not encompass simultaneous cognitive and psychomotor skills.
Furthermore, adequate dexterities are not developed prior to entering the operating room, and the minimum skills needed to be developed in laparoscopic surgery have not yet been standardized [2-11]. Not all surgeons practice laparoscopy, quite many of them are reluctant to learn it in the laboratory, and we are still used to the traditional method of surgery-learning: teacher-apprentice, even though over 60% of surgeries are minimally invasive [12].
It still exists a predominance of conventional surgical treatment for acute abdomen, although acute abdomen through conventional surgery reports more postoperative discomfort. Plus, there are no uniform definitions of protocols and modes of treatment in acute surgical abdomen, and we have not yet formed the necessary human resources to apply laparoscopic surgery 24/7 [7,11].
There are many complications in laparoscopic surgery due to lack of expertise, and there is no consensus or uniform criteria to determine a conversion to Laparoscopic Surgery, and neither there exists consensus on the complication factors in acute-abdomen laparoscopic surgery [7,13,14]. As stated by Camacho et al. [14], the development of new surgical techniques and their swift application in minimally invasive surgery generates the need for optimal, effective and comprehensive learning from the first phase of teaching, which is the training process.
Flyckt et al. conducted a study to see if female surgical residents underestimate their surgical skills compared to males in a standardized laparoscopic skill test. In a sample of 26 male and female general surgery residents and 25 obstetrics and gynecology residents from two academic centers, they were asked to predict their score before taking the Standardized Skills Examination of Fundamental Laparoscopic Surgery. In the results there was no difference in the actual score based on residence or gender. However, male residents more accurately predicted their scores, while female residents significantly underestimated them. Conclusion: There are gender differences in the estimation of laparoscopic surgical capacity that do not reflect actual differences in performance [15].
Dull et al. investigated the resident impact on the surgical time of a single general surgeon in an ambulatory surgical setting. Six-hundred and twenty-five cases were analyzed. Operating time for each operation increased with the participation of residents. Umbilical hernia repairs were associated with a 19% time increase; laparoscopic cholecystectomies showed a 15% increase, and laparoscopic inguinal hernia repairs showed a 25% increase. The conclusion being that each surgeon must decide whether the increase in the operative duration caused by the participation of the residents is justified by the intangible benefits provided by their presence [16].
Zendejas et al. investigated whether the performance of surgeons measured by the basics of laparoscopic surgery (FLS) assessment program could predict their performance in a surgical trial; finding that FLS has the ability to evaluate surgeons prior to enrolling in a surgical trial. Although the best FLS scores predicted better operative performance and improved operative time, other outcome measures of the study showed no difference. These findings have significant implications for documenting the laparoscopic experience of surgeons in practice, and may allow a more adequate selection of surgeons to participate in clinical trials [17].
Thomaier et al. while evaluating the transfer of skills between the platforms of minimally invasive surgical simulation among the participants. Forty medical students participated, of which 20 held a practice session in the robotic simulator and 20 a laparoscopic one. Two minimally invasive and blinded surgeons evaluated participants before and after training, using a previously validated subjective assessment scale.
Objective measures were also recorded including time to complete the task and the Mimic dV-Trainer motion metrics. In their onset results, there were no significant differences between the training groups, as measured by objective and subjective measures. After training, random participants of the laparoscopic practice group completed the laparoscopic task more quickly and scored higher overall score than the robotic group. Participants with robotic training performed the robotic task faster, with better movement economy, and with higher global scoring scores than the laparoscopic group.
The robotic practice group also demonstrated significantly improved performance in the laparoscopic task. The laparoscopically trained participants also improved their robotic performance, although the robotic group had a higher percentage of improvement in the robotic task. Concluding that skills acquired through practice in laparoscopic or robotic simulation platforms seem to be transferable between modalities. However, participants demonstrate superior ability in the mode in which they specifically train [18].
Palazzetti et al. argued that the open surgical approach remains widely adopted, although in the last two decades efforts have been made to evaluate if minimally invasive procedures, whether laparoscopic or robot assisted, could show a benefit in comparison with the standard technique. Similarly, laparoscopic and robotic radical cystectomy shows a reduction in blood loss, hospital stay and transfusion rates, but a longer operative time, whereas open radical cystectomy is typically associated with a shorter operative time but with longer hospital admission, and possibly a higher rate of highgrade complications [19].
Rivas-Blanco et al. argue that the main difficulty in laparoscopic or robot-assisted surgery is the narrow visual field, restricted by the access port of the endoscope. This restriction is accompanied by the difficult handling of the instruments, which is due not only to the access port, but also to the loss of depth of field and perspective due to lack of natural lighting.
They found that intra-abdominal cameras offer a greater number of intuitive views of the surgical field compared to the conventional telescope and appear to provide a similar view to that of open surgery. Areas previously inaccessible to the standard telescope can now be reached. Additional light sources create shadows that increase the perspective of the surgical field.
Concluding that this system seems to increase the possibilities of laparoscopic or robot assisted surgery, since it offers an instant vision of almost the entire abdomen, allowing more complex procedures, which currently require an open path [20].
General Objective
To ascertain the efficiency of the Basic Training Program in Laparoscopic Surgery in the development of cognitive and motor skills at the Center for Studies on Prevention and Correction of Abdominal Diseases, CEPCEA in Piura, Peru.
Methodology
We took the population of 55 trainees from different Latin- American countries (Peru, Ecuador, Colombia, Bolivia, El Salvador, Antilles, Guatemala) who went to the CEPCEA Training Center in the city of Piura, Peru from January 1st to December 31st, 2016; group coming from the specialties of general surgery, gynecology, urology, oncology surgery, pediatric surgery, even general practitioners and, in a single case, a nurse who was a student of the last year of Medicine.
CEPCEA’s Training Program lasts 5 days in which the trainee acquires, develops and shows both manual and cognitive skills, which are graded by means of pre and post-tests which are applied according to the variables to be assessed; for example, the exercises in the FLS training box variables are measured on a time basis, while the skills for the chicken endo-trainer are evaluated according to perfection and cleanliness of the processes to be performed. The cognitive part is evaluated by means of a 20-question exam where 20 is the highest score and each point corresponds to a correct answer. We used the SPSS v.21 program as statistical software.
The methodology of the course is based on the PBL system (Problem-Based Learning) which has shown great comprehension by the trainee and which is divided into 4 modules: in inanimate objects, biological tissue, dead and live animal and finally as assistant in humans, where the best of each Continent is combined: part of the SAGES’ American FLS (Fundamentals of Laparoscopic Surgery) CEPCEA-modified program, the European-originated endo-trainer for practice on dead chickens, and the KAIZEN, the Japanese system of continuous quality and improvement, which consists of 5 very strict stages: Order, Classification, Cleaning, Discipline and Standardization.
Each module consists of the following
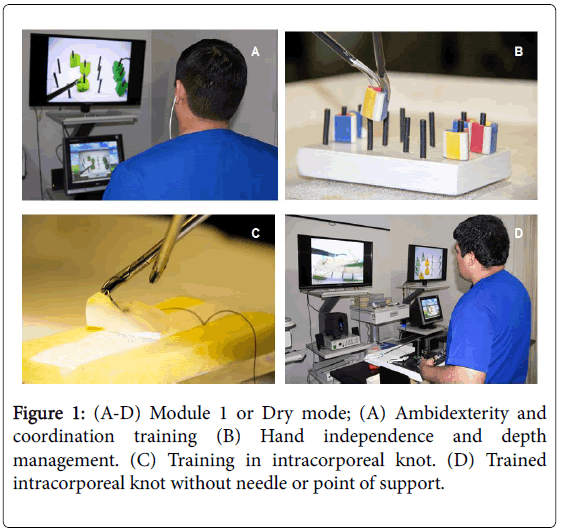
Module 1 or Dry Mode: Knowledge of laparoscopic instruments and intra-abdominal aggregated utility, objects transfer, rotor use, coordination of both hands, visual field expansion, pattern cutting, traction and contraction, theory of knots, tips for simple intracorporeal knots and according to utility by specialty, ergonomics correction, theory of monitors, cameras, laparoscopes and fiberglass cables, perfect realization of the Roeder knot: by progressive tips (Figure 1).
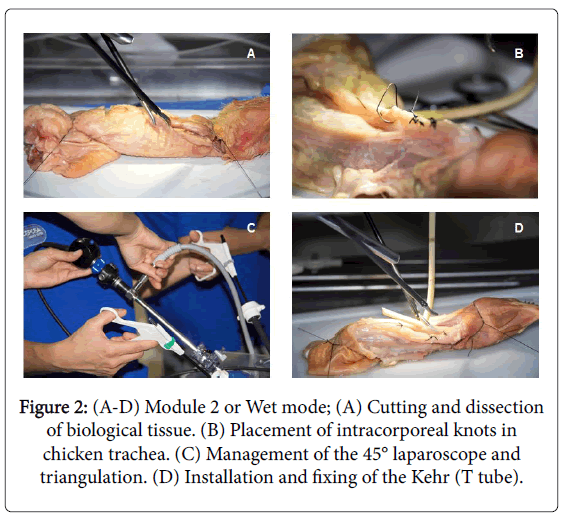
Module 2 or Wet Mode: Tips for use of laparoscopic instruments, centering of the camera with 30° and 45° laparoscope, horizons and third dimension exercises, objective change and adequate panning, advantages of laparoscopes of 30° and 45° over laparoscope of 0°, Kehr (T tube) dominance with both hands (third dimension) and chamber of 30° and 45° (in pairs), practice in Endotrainer on chicken neck: vertical and transversal cut of 90°, how to calculate measurements during a surgery, dissection of the SCT (subcutaneous cellular tissue), use of both hands, focus on monitor, horizon control, cut trachea at 12 hours, partially dissect esophagus, cutting of esophagus and Kehr placement with 45° optics, calculation of distance between points (0.3-0.5 cm) (Figure 2). Theory of energy sources: monopolar and bipolar, irrigation and suction in laparoscopy, theory and practice using Verres and trocars; theory of the pneumoperitoneum (physiological changes), tower knowledge, quality cables and connections, white balance.
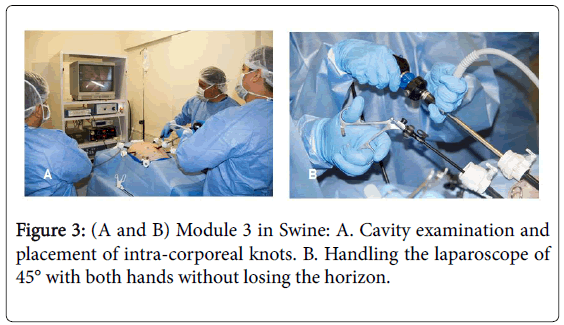
Module 3 in Swine: Verres’ revision and placement, trocar placement, CO2 leak detection (insufflator tips), Triangulation, use of 45° laparoscope, camera bimanuality without loss of horizon, complete examination of cavity, mirror work, Intestinal examination, lateral suture in a single plane, calculation of distance between points (Figure 3).
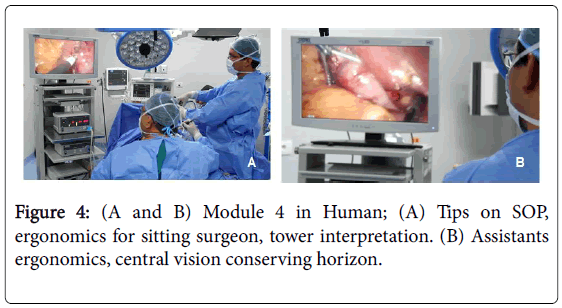
Module 4 in Human: Operating Room Tips, Tower review, electrocautery configuration, insufflator use, position of the cialitic lamp for surgery, application of insufflator theory, 45° camera use and complete abdominal cavity examination, Operating Room ergonomics and overall work results of the surgical team (Figure 4).
Results
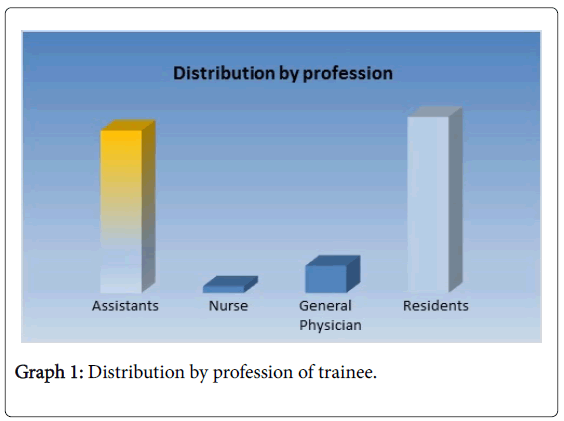
The total population of the study was 55 trainees, of whom 24 were assistants, 26 residents, 4 general practitioners and a graduating nurse who was in the last year of medical school. The specialties attending the training were as follows: general surgery 32, gynecology 11, urology 3, surgery oncology 3 and pediatric surgery 1. The attendance of the male population was higher with 72.7% and female attendance with 27.3%. Table 1 and Graph 1 shows that it is the resident physicians, with 47.3% of them trained and the attendants with 43.6%.
| Profession | Frequency | Percentage |
|---|---|---|
| Assistant | 24 | 43.6 |
| Nurse (Med Student) | 1 | 1.8 |
| General Physician | 4 | 7.3 |
| Resident | 26 | 47.3 |
| Total | 55 | 100.0 |
Table 1: Distribution by profession of trainees.
In Table 2 we see that 58.2% of those trained were General Surgeons and 20% Gynecologists. There are 7.3% of General Medicine practitioners who are interested in this field of surgery.
| Specialty | Frequency | Percentage |
|---|---|---|
| General Surgery | 32 | 58.2 |
| Oncologic Surgery | 3 | 5.4 |
| Pediatric Surgery | 1 | 1.8 |
| Instrumentist Nurse (Med Student) | 1 | 1.8 |
| Gynecologists | 11 | 20.0 |
| General Medicine | 4 | 7.3 |
| Urology | 3 | 5.5 |
| Total | 55 | 100.0 |
Table 2: Distribution by specialty of trainees.
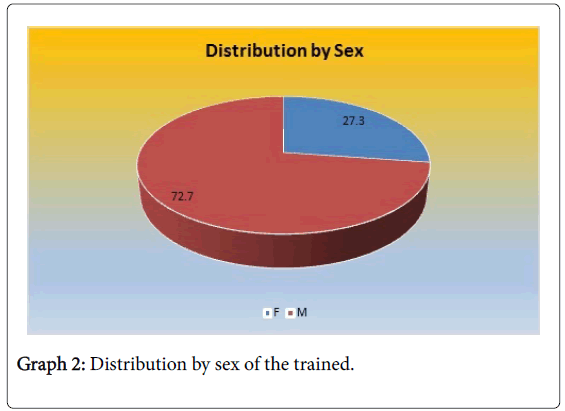
In Table 3 and Graph 2, 72.7% of the trainees were males, which is almost three times more than the females with 27.3%. In Table 4, when the distribution by age group is observed, age groups between the ages of 30 and 44 are the ones that most requested to be trained. Likewise, the group between the ages of 30 and 34 was the highest percentage: 29.1% and the group between 45 and 51 was the lowest with 9.1%.
| Sex | Frequency | Percentage |
|---|---|---|
| F | 15 | 27.3 |
| M | 40 | 72.7 |
| Total | 55 | 100.0 |
Table 3: Distribution by sex of trainees.
| Age Groups | Frequency | Percentage |
|---|---|---|
| 25 to 29 | 9 | 16.4 |
| 30 to 34 | 16 | 29.1 |
| 35 to 39 | 14 | 25.5 |
| 40 to 44 | 11 | 20.0 |
| 45 to 51 | 5 | 9.1 |
| Total | 55 | 100.0 |
Table 4: Distribution by age groups of the trainees.
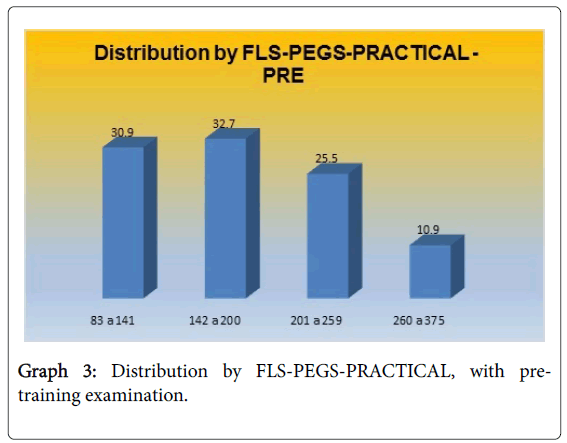
The practical tests pursue a synergy with bimanual or ambidextrous ability, so the evaluation to be taken into account was the transfer of objects, where the shorter the time the better the evaluation, which at the beginning of the training had an average of 189.6 seconds and at the end of same 68.4 seconds; being the highest value 375 seconds and the lowest 44 seconds.
Table 5 and Graph 3 Shows the results of the pre-qualification exam, where 32.7% scored between 142 and 200; 30.9% scored between 83 and 141.
| FLS-PEGS-PRACTICAL: PRE | Frequency | Percentage |
|---|---|---|
| 83 to 141 | 17 | 30.9 |
| 142 to 200 | 18 | 32.7 |
| 201 to 259 | 14 | 25.5 |
| 260 to 375 | 6 | 10.9 |
| Total | 55 | 100.0 |
Table 5: Distribution by FLS-PEGS-PRACTICAL, with PRE-training examination.
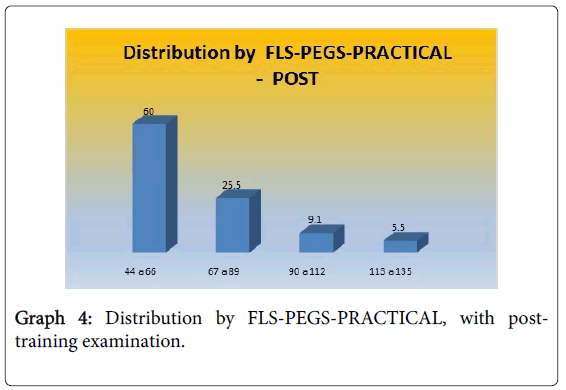
Table 6 and Graph 4 shows the results of the post-qualification exam, where 60% scored between 44 and 66; 25.5% scored between 67 and 89.
| FLS-PEGS-PRÁCTICO: POST | Frequency | Percentage |
|---|---|---|
| 44 a 66 | 33 | 60.0 |
| 67 a 89 | 14 | 25.5 |
| 90 a 112 | 5 | 9.1 |
| 113 a 135 | 3 | 5.5 |
| Total | 55 | 100.0 |
Table 6: Distribution by FLS-PEGS-PRACTICE, with POST-training examination.
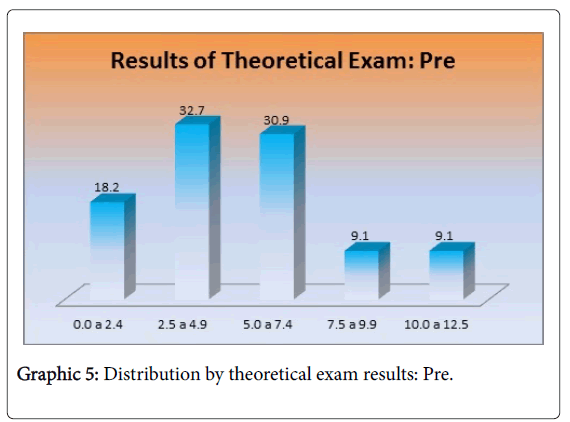
Table 7 and Graph 5 Shows the results of the pre-qualification theoretical exam, where 32.7% scored between 2.5 and 4.9; 30.9% scored between 5.0 and 7.4. It is important to emphasize that 18.2% scored between 0.0 and 2.4.
| Theoretical exam pre | Frequency | Percentage |
|---|---|---|
| 0.0 a 2.4 | 10 | 18.2 |
| 2.5 a 4.9 | 18 | 32.7 |
| 5.0 a 7.4 | 17 | 30.9 |
| 7.5 a 9.9 | 5 | 9.1 |
| 10.0 a 12.5 | 5 | 9.1 |
| Total | 55 | 100.0 |
Table 7: Distribution by theoretical exam results: Pre.
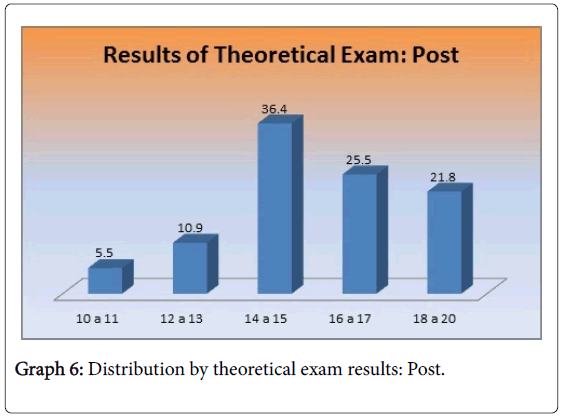
Table 8 and Graph 6 shows the results of the post-qualification theoretical exam, where 16.4% scored between 10 and 13; 83.6% scored over 14, which are a good score in this test. Likewise, 21.8% scored between 18 and 20. It is important to emphasize that there was no score between 0 and 9.
| Theoretical exam: post | Frequency | Percentage |
|---|---|---|
| 10 to 11 | 3 | 5.5 |
| 12 to 13 | 6 | 10.9 |
| 14 to 15 | 20 | 36.4 |
| 16 to 17 | 14 | 25.5 |
| 18 to 20 | 12 | 21.8 |
| Total | 55 | 100.0 |
Table 8: Distribution by theoretical exam results: Post.
The results of the cognitive test are -mostly- directly proportional to the practice, where the media of the tests evaluated (at 20 points the top score) is 5.8 points at the beginning and 14.9 points at the end of the training, the lowest achieved score being of 0 points and the highest 20 points, the latter being only achieved in the post test.
In Table 9, we see that the FLS-PEGS-PRACTICAL: PRE AND POST training, show differences in the average that was: 189.64 ± 62.47 and 68.44 ± 19.92, respectively. Likewise, we appreciate that the THEORETICAL EXAM: PRE AND POST training shows differences in the average, that was: 5.8 ± 3.62 and 14.9 ± 1.69, respectively.
| Descriptive Statistics | N | Minimum | Maximum | Media | Standard Deviation |
|---|---|---|---|---|---|
| FLS-PEGS- PRACTICUM: PRE | 55 | 83 | 375 | 189.64 | 62.47 |
| FLS-PEGS-PRACTICUM: POST | 55 | 44 | 135 | 68.44 | 19.92 |
| THEORETICAL EXAMEN: PRE | 55 | 0 | 12.5 | 5.8 | 3.62 |
| THEORETICAL EXAMEN : POST | 55 | 10 | 18.5 | 14.9 | 1.69 |
Table 9: Descriptive statistics of the results of the exams for the PRE and POST training evaluation of the trainees.
Conclusion
The cognitive and motor level of the trainees with which they initially attend the CEPCEA Training Center Program is deficient according to the standards to be expected at the end of their residency (or during the same), which by contrast highlights and demonstrates their improvement and development through the intensive training received in the program. There is no difference in the development of practical and cognitive skills between an assistant and a resident; on the contrary, we realized that the learning curve is faster in someone who has no experience in laparoscopy than in those already trained, who come in with certain learned skills, but unfortunately also with some “corks” or preconceived ideas which may be hard to dislodge. The basic training in laparoscopic surgery provided by the CEPCEA Training Center Program develops skills which are useful and applicable to all surgical specialties that perform this type of minimally invasive surgery. The training program in Laparoscopic Surgery at CEPCEA Training Center is, therefore, efficient, necessary and crucial to the development of manual and theoretical skills and dexterities in laparoscopic surgery in all its surgical specialties. There is a growing interest in learning this type of surgical technique from general practitioners and young physicians; on the contrary, we find some refusal to be trained by specialist surgeons of the older age, the motive would be an interesting cause to investigate.
References
- Dawson L, Kaufman J (1998) The imperative for medical simulation. Proceedings of the IEEE. USA 86: 479-483
- Salas R, Ardanza P (2011) National center for medical improvement and teaching aids. Simulation as a method of teaching and learning.
- Degregori AJ (2005) Efficiency of the basic training program in laparoscopic surgery of the research unit in laparoscopic surgery in post-surgery residents of the State of Lara, Venezuela. Thesis. Barquisimeto, Venezuela.
- Rodríguez CF, Martínez LL, Gabilondo PB, Gabilondo NF, Atisha FY, et al. (2006) Computerized virtual immersion simulator as a model for initiation of urological laparoscopy training. Urology proceedings records. Spain 30: 819-823.
- Enciso SS (2013) Evaluation of the acquisition of skills and surgical skills during training in laparoscopic surgery. PhD Thesis, Spain.
- Roque GR, Torres PC, Barrios OI, Martínez AM, Barreras GJ, et al. (2012) Instruments for assessing skills in basic laparoscopic surgery. Superior Med Education Havana Cub: 26.
- Rodríguez SJ, Manuel PC, Fernández DJ, Gutiérrez CJ, Martín JA, et al. (2010) Evaluation of training of residents in laparoscopic surgery in the laboratory based on a model of digestive anastomosis.
- Vázquez MG, Guillamet LA (2009) Training based on simulation as an essential innovation in medical training. Medical Education 12.
- Palazuelos JC, Martín JA, Rodríguez SJ, Fernández DM, Gutiérrez CJ, et al. (2009) Training Program for the surgery resident in an experimental laboratory of minimally invasive surgery (CENDOS). Cir 85.
- Sánchez MF, Sanz SE, Usón J. Díaz GI (2004) Effectiveness of an intensive training program in improving basic skills in laparoscopic urological surgery.
- Smith CD, Farrell TM, McNatt SS, Metreveli RE (2001) Assessing laparoscopic manipulative skills. Am J Surg 181: 547-550.
- Beltrán GV, Hernández PL (2013) Impact of training with laparoscopy simulators within the general surgery program. Thesis. Bogotá. Colombia.
- Diaz RP, Leyva SE (2013) Methodology to determine the quality of evaluation instruments. University of Medical Sciences of Holguin, Cuba.
- Camacho FJ, Ramirez JF, Peralta MC, Cortés M (2009) Determination of competence levels in basic training for laparoscopic surgery. Colombia.
- Flyckt RL, White EE, Goodman LR, Mohr C, Dutta S, et al. (2017) The use of laparoscopy simulation to explore gender differences in resident surgical confidence. Obstet Gynecol Int.
- Dull MB, Gier CP, Carroll JT, Hutchison DD, Hobbs DJ, et al. (2016) Resident impact on operative duration for elective general surgical procedures. Am J Surg 9610: 31119-31129.
- Zendejas B, Jakub JW, Terando AM, Sarnaik A, Ariyan CE, et al. (2016) Laparoscopic skill assessment of practicing surgeons prior to enrollment in a surgical trial of a new laparoscopic procedure. Surg Endosc.
- Thomaier L, Orlando M, Abernethy M, Paka C, Chen CC (2016) Laparoscopic and robotic skills are transferable in a simulation setting: a randomized controlled trial. Surg Endosc
- Palazzetti A, Sanchez-Salas R, Capogrosso P, Barret E, Cathala N, et al. (2016) Systematic review of perioperative outcomes and complications after open, laparoscopic and robot-assisted radical cystectomy. Actas Urol Esp.
- Rivas-Blanco I, Sánchez-de-Badajoz E, García-Morales I, Lage-Sánchez JM, Sánchez-Gallegos P, et al. (2016) Global vision system in laparoscopy. Málaga, España. Actas Urol Esp.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 5237
- [From(publication date):
February-2017 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 4490
- PDF downloads : 747