Traditional Ayurvedic medicines: Pathway to develop anti-cancer drugs
Received: 03-Dec-2015 / Accepted Date: 18-Dec-2015 / Published Date: 25-Dec-2015 DOI: 10.4172/2329-9053.1000130
Abstract
Ayurveda, “life knowledge”, is an ancient Indian traditional medical system, which has been practiced for >5000 years and still in use with the same importance among many cultural tribes in Indian sub-continents. Ayurvedic medicine is a unique holistic approach to treatment where herbal medicines, special diets, yoga and relaxation methods, and lifestyle management are key strategies for curing various chronic diseases like diabetes, cancer, cardiovascular, neurological disorders and many other. Cancer is biologically complex disease, causing local damage and inflammation of cells due to lack of full response in a specific tissue that is responsible to maintain cellular differentiation, survival, proliferation and death. Studies have suggested that bioactive phytochemicals present in Ayurvedic plants (fruits, vegetables and herbs) mediate their effects by inhibiting some of the recently identified inflammatory pathways. Nevertheless, for successful implementation of Ayurvedic principles to drug discovery, major concerns relating to proportion, practicality, safety and drug interactions and possible side effects of newly developed Ayurvedic drugs and formulations need to be addressed. Systematic investigations of Ayurvedic drugs, employing contemporary scientific tools and methods, are expected to lead to the discoveries of major significance. Explorations involving studies of bioactive phytochemicals, their side effects, the specific potential targets and the mechanisms of action would transform this traditional therapeutic approach to standard Ayurvedic drug discovery which would be accepted and embraced by global populations. Current review focuses on the importance of anti-cancer drug discovery from Ayurvedic medicines in the modern context, ongoing improvements and major achievements in the field over the past decade or two.
Keywords: Ayurveda; Harmony; Balance
1738Introduction
“Ayurveda ” – ayus (life) and veda (science/knowledge) means “the science of life”, has unbroken long history as ancient Indian medicinal system for over five thousand years. Ayurveda is often known as the “Mother of all healing ” [1] that brings harmony and balance in all areas of life including mind, body, spiritual well-being and social welfare of mankind [2].
According to Ayurveda, the primary components of human beings and universe is one or combination of the five basic elements (Panchamahabhutas) [3], namely: Prithvi (earth-the principle of inertia), Ap (water-the principle of cohesion), Teja (fire-the principle of radiance), Vayu (air-the principle of vibration), Akasha (ether-the principle of pervasiveness). These five basic principles form three vital forces called Tridoshas : Vata (maintaining nervous system responsible for cell growth, differentiation, cell death, movement of cells, molecules, nutrients and waste), Pitta (maintaining venous system for chemical reactions in the body including digestion, metabolic process, immunity and temperature control) and Kapha (stream nutrition to the arterial system responsible for structure, growth, and protection) [3].
Physical, mental and physiological features (constitution or Prakriti ) of every individual are distinctly different from one another. In Ayurvedic medical practice, the combination of Tridosha and panchamahabhutas are used to determine the nature (Prakriti ) of an individual, accordingly, the treatments are individualized [3]. For example, alterations in “Pitta dosha ” is allied with inflammatory diseases [4] resulting from weakened organs (Dhatus ), and hence “Rasayanaprayoga ” (immunotherapy) is commonly practiced for rejuvenating the body’s support system [5]. Ayurvedic medicine is a holistic and multidimensional medical system with inbuilt capacity to diagnose and treat various illnesses including chronic diseases such as cardiovascular, neurological, diabetes, cancer and many other diseases.
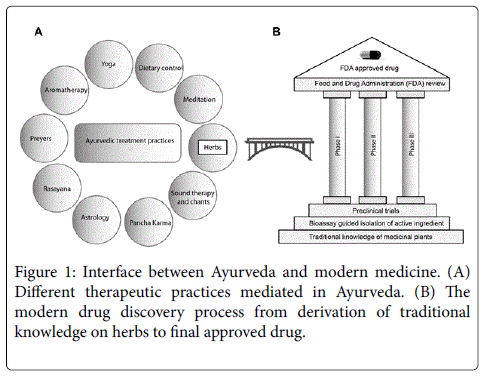
In the context of Ayurveda, a good health is defined as balanced situation of Tridoshas. Imbalance in these vital forces causes diseases and the specific treatment plan for any particular imbalance is defined and practiced in Ayurveda from vedic era. As illustrated in (Figure 1A).
The treatment modality involves a combination of different approaches including yoga, dietary control, meditation, prayers and other means. However, medicinal herbs received greater prominence than other mode of treatments due to their efficacy and prompt curative properties. Globally, herbs and their derivatives became major component of different traditional medicinal systems to treat diseases. Modern scientific and technological advancements have the potential to transform the traditional knowledge of medicinal plants into modern drugs, as described in (Figure 1 B). Many medicinal plant derived drugs such as aspirin, reserpine, and digitalis are a few examples of therapeutic agents discovered from medicinal plants [6]. However, more systematic and robust research is required to derive full benefits of traditional herbs and to discover effective therapeutic agents for life threatening diseases.
Ayurvedic formulations have been the first line of treatment in Indian subcontinent for thousands of years due to their less toxicity and wide acceptability [7]. The emerging chemotherapeutic approaches have hampered the practice of Ayurvedic medicine system during the past couple of decades. This is primarily due to the effectiveness of medicinal herbs on disease symptoms is relatively slower than chemotherapeutic drugs. Apparent success of chemotherapeutic drugs, in the treatment of cancer and other serious diseases, has been masked by their side effects and toxicity which have become major downside. In addition, chemotherapy approaches often are not successful for the treatment of major death causing diseases including cancer. This situation has primarily lead to the renewed interest in complementary therapies as a pathway for finding cure for cancer.
In Ayurveda, Charaka and Sushruta Samhitas define cancer as inflammatory or non-inflammatory swelling often known as Granthi (minor neoplasm) or Arbuda (major neoplasm) [8]. Minor neoplasm is mainly caused by weak Shukra Dhatu (tissue regeneration and cell division) interrelated with imbalanced Kapha and/or Vata Dosha . However, missing coordination amongst all these three vital forces is responsible for unhealthy and maline tridoshic major tumor [9]. In principle, it is caused due to unhealthy lifestyle, such as consumption of unhealthy foods, poor hygiene, or bad habits/addiction, or from physical trauma, causing major discrepancies in Tridoshas (Vata, Pitta , and Kapha ) [10]. Inhibition of the tumoral growth and their destruction is accomplished by making changes in metabolic defects and restoring normal tissue functions by improving lifestyle, known as “Sama Dhatu Parampara” [11].
In modern science, cancer is defined as hyper proliferative disorder that involves damage and inflammation of cells in a specific tissue that is responsible to maintain cellular differentiation, survival, proliferation and death [12]. After cardiovascular diseases, cancer is still the second leading cause of death worldwide worse than AIDS, tuberculosis and malaria. According to World Health Organization (WHO), in the year 2012, total cancer deaths were 8.2 million (~22,000 cancer deaths a day), which means that around 15% of total deaths are caused by cancer alone [13]. It is estimated by 2030, globally 21.7 million new cancer cases may exist and 13 million deaths simply due to the growth and aging of the population [14].
In modern medicine, chemotherapy is the first line treatment method for many types of cancer (especially for metastatic disease) [15]. After a huge investment, intensive and systematic research in drug discovery, there are some useful therapeutic agents in the market that include penicillin [16], temozolomide, carmustin, carboplatin and thalidomide [17]. Biologically, once normal cells get mutated and/or become cancer cells and lose most of the normal regulatory functions and continue to multiply cancer cells which are not seen in normal cells [18]. Thus chemotherapeutic drugs do not work properly on cancer as they are mainly targeted to kill cancer cells but not repair the regulatory function. As a result, the degradation takes place continuously. The disappointment in the use of chemotherapeutic treatments, as expected, is also due to many toxic side effects that occur during and after the treatment [19] which will affect the quality of life of the patient due to the very treatment that is intended to provide relief. As a result, the global community is still looking for an alternative and natural medicine that could cure diseases with least side effects and issues.
Towards these goals, traditional medical systems including Ayurveda, Chinese medicine and European medicine have attracted attention as complementary approaches. Ayurvedic medicinal plants have a special place in the treatment of different types of cancer with established outcomes for thousands of years and hence received particular interest. This review is focused on the discovery of bioactive molecules, ongoing improvements, major achievements, current issues and the areas to be improved in the field of anti-cancer drug development from the vast knowledge of Ayurvedic medicine.
Bioactive molecules from Ayurvedic medicine
Plants produce armoury of secondary metabolites that play a vital role in their biochemical pathways and defence against pests. Taking the advantage of bioactive properties, humans started consuming plant products as neutraceuticals. In Ayurveda treatment practices, diet rich in fruits, vegetables, grains and herbal extracts [20] rich in neutraceuticals are consumed to bring health benefits [21,22]. Traditionally, Ayurvedic medicinal plants are consumed in different forms [7]: chewing, swallowing, applying over the skin, teas, consuming with milk, ghee, honey or other solvents commonly known as “Anupana ” in Ayurveda [23].
To date, more than 25,000 plant-based formulations and individual herbs are used in folk and traditional medicine in India by more than 387 thousand qualified practitioners of traditional medicinal system [24]. Over 75 formulations are readily available in the Indian market for health and vitality; all contain Withania somnifera (100%), Asparagus racemosus (81.5%), A. adscendens (48%) and Curculigo orchioides (15 %), with other plants in small proportions [25]. The plants Glycirrhiza glabra, Piper longum, Adhatoda vasica , W. somnifera , Ciprus rotundus, Tinospora cordifolia, Berberis aristata, Tribulus terrestris, Holarrhena antidysenterica and Boerhavia diffusa are used in approximattely 140 herbal formulations. Triphala containing potent anticancer agents (Terminalia chebula, T. bellerica and Embelica officinalis ) has been found in more than 219 formulations [26]. Some of the formulations that are widely used in treatment of cancer are listed in (Table 1).
| S.No | Name of formulation | Name of herbal plants |
|---|---|---|
| 1. | United States Patent 6780441 Sahajanand Biotech Private Limited (Gujarat, IN) | Withania somnifera, Chlorphyton borivilianum, Boerhavia diffusa, Elephantopus scaber, Moringa oleifera, Tecoma undulata, Bauhinia purpurea, Ficus racemosa, Cyperus rotundus, Sphaeranthus acmella and Tinospora cordifolia. |
| 2. | Immunotone Sino-Vedic Cancer Research Centre |
Immunotone herbal formulation contains active princples isolated from selected antimutagenic and immunoenhancing herbs such as Aegle marmelos,Aloe vera, Alpinia galanga, Andrographis paniculata, Azadirachta indica, Berberis vulgaris, Curcuma domestica, Emblica officinalis, Glycine max, Morinda citrifolia, Ocimum sanctum, Tinospora cordifolia, Trigonella foenum-graecum, Viscum album, Withania somnifera and Zingiber officinale. |
| 3. | Cancertame Sino-Vedic Cancer Research Centre |
Cancertame herbal formulation contains active principles isolated from Bauhinia variegata, Catharanthus roseus, Curcuma longa, Glycine max, Glycyrrhiza glabra, Gossypium hirsutum, Nigella sativa, Phyllanthus emblica, Plumbago zeylanica, Rubia cordifolia, Solanum indicum, Zingiber officinale, Aloe vera, Amoora rohituka and Azadirachta indica. |
| 4. | Oncotame Sino-Vedic Cancer Research Centre |
Oncotame herbal formulation contains active princples isolated from Ginkgo biloba, Oldenlandia diffusa, Podophyllum emodi, Prunella vulgaris, Psoralea corylifolia, Saussurea lappa, Solanum nigrum, Withania somnifera, Panax ginseng, Catharanthus alba, Curcuma aromatica, Andrographis paniculata, Aloe barbadensis, Emblica officinalis and Viscum album. |
| 5. | Chen Pi Ageless Herbs |
Citris reticulate, Astragalus membranaceus, Arctium lappa, Ganoderma lucidum, Trifolium pretense, Eleutherococcus senticosus, Rumex crispus, Atractylodes macrocephala, Spatholobus suberectus, Ascophyllum nodosum, Prunella Vulgaris, Salvia miltiorrhiza, Carthamus tinctorius, Rumex acetosella, Foeniculum vulgare, Althaea officinalis. |
| 6. | Caractol | Blepharis Edulis, Piper Cubeba Linn, Smilax China Linn, Hemidesmus Indicus, Tribulus Terrestris, Ammania Vesieatoria, Lepidium Sativum Linn, Rheum emodi wall. |
| 7. | Triphala | Terminalia chebula, Embelica officinalis, Terminalia bellerica. |
| 8. | Vidakana choornam | Embelia ribes, Mrigna oleifera, piper longum |
| 9. | Liv 52 | Capparis spinosa, Cichorium intybus,Mandur bhasma, Solanum nigrum, Terminalia arjuna, Cassia occidentalis, Achilea millefolium, Tamarix gallica |
| 10. | Immu-21 | Ocimum sanctum, Withania somnifera, Emblica officinalis and Tinospora cordifolia |
Table 1: List of Herbal formulations available in the market for cancer treatment [73-75]
Modern drug discovery process is primarily driven by tracing the traditional medicinal use followed by bioactivity guided fractionation to identify major active ingredients.
In recent decades, versatile analytical techniques have emerged and became readily available to aid the quest for rapid discovery of bioactive compounds. Isolation, identification and characterization of bioactive compounds from medicinal plants is currently a major scientific theme in many research laboratories around the globe. Modern instrumental techniques, such as, mass spectrometry and nuclear magnetic resonance spectroscopy play a major role in the identification, characterization and classification of novel bioactive molecules.
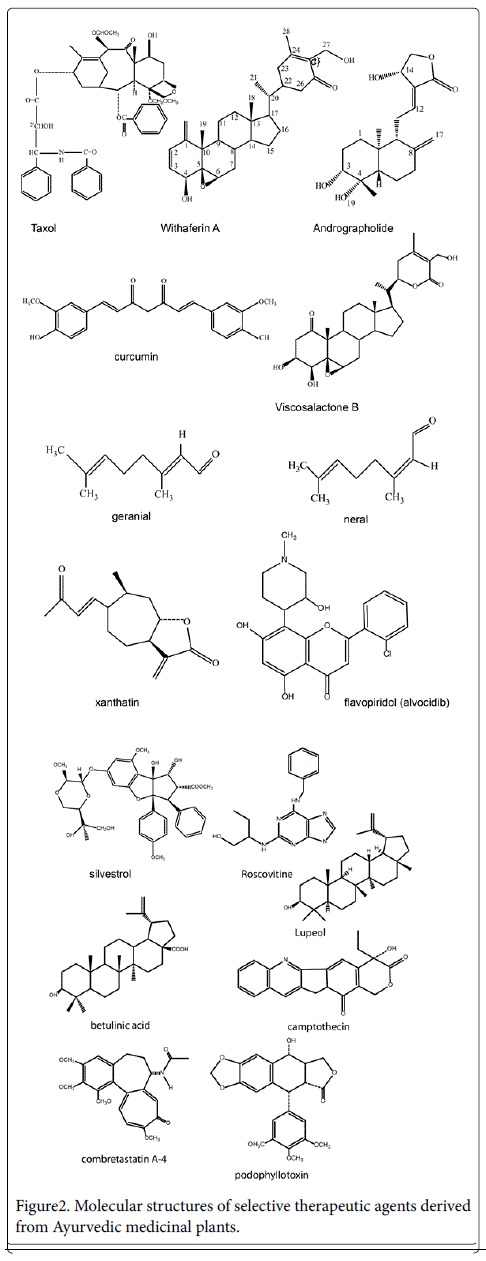
Phytochemicals including alkaloids, carotenoids, phenolics, organo sulfur compounds, non-protein amino acids, saponins, flavonoids and several other molecules with pharmacalogically important activities have been isolated from Ayurvedic herbs [27]. For example, flavonoids such as apigenin and quercetin, have been shown to inhibit melanoma cancer cell lines and metastasis [28]. Research directed towards the identification of agents capable of inhibiting lung colonization revealed that, many polyphenols have the ability to decrease the number of B16- BL6 colonies in lung in a dose-dependent manner [28]. Structures of several anticancer agents derived from Ayurvedic medicinal plants are provided in (Figure 2).
Typically, fruits, vegetables, herbs, and spices containing isothiocyanate, curcumin, genistein, epigallocatechin gallate, lycopene, resveratrol and several other bioactive phytochemicals are consumed as part of regular diet [29] that act as chemotherapeutic agents.
Many plant derived compounds are available in the market and are produced on commercial scale by pharmaceutical companies (Table 2) [30].
| S.No | Plant species Botanical name (local name) |
Active molecules/plant extracts | Biological anti-cancer activities against |
|---|---|---|---|
| 1 | Andrographis paniculata Nees (Green chirayta) | Andrographolide, neoandrographolide and dehydroandrographolide | B16F0 melanoma syngenic and HT-29 xenograft models[47] , 2-cell line panel containing MCF-7 (breast cancer cell line) and HCT-116 (colon cancer cell line)[49], multiple myeloma [50,51], rats induced with gastric ulcer [52] |
| 2 | Alpinia galangal Willd (Greater galangal) | 1’S-1’-acetoxychavicol acetate, 1,8-cineole, beta- bisaboline and beta- seline, Galangin and Camphor | COR L23 cells (lung cancer cell line) and MCF7 cells (breast cancer cell line) with IC50 7.8uM and 23.9uM[76] |
| 4 | Aristolochia indica(Birthwort) | Aristolochic Acid | Cytotoxic against Chinese hamster ovary-K1 ( CHO-K1) cells [77] |
| 5 | Agati grandiflora(Humming bird tree) | Whole plant material ethanol extract | Anticancer effect against Ehrlich Ascites Carcinoma (EAC) in mice cell line [78] |
| 6 | Albizzia lebbeck(Rain tree) | triterpenoid saponins [79] | Antitumor activity against gall tumors [80] |
| 7 | Allium sativum (Garlic) | Abstract Diallyl sulfide[81], S-allylcysteine, S-allymercaptol-cysteine | Cytotoxic against colorectal adeno carcinoma [81] |
| 8 | Aloe vera (Aloe) | Barbaloin (aloe-emodin, aloesin, aloin), acemannan | Selectively inhibited the growth of human neuroectodermal tumors in mice[82], caused tumor shrinkage, tumor necrosis and lymphocytic infiltration in dogs [83] |
| 9 | Alstonia scholarisLinn (Milky pine, sapthaparna) | ethanol extract (Echitamine[84]) | Selectively inhibited the forestomach carcinogenesis in mice[85] |
| 10 | Amorphopallus campanulatus(Elephant foot yam) | Methalonic extract | Cytotoxic and apoptotic activities against human hepatoma cell line [86], against human colon carcinoma cell line HCT-15[86] |
| 11 | Amoora rohituka(Rohituka tree) | Petroleum ether extract | Cytotoxic effects on breast and pancreatic cnacer cells[87] |
| 12 | Azadirachta indica(The wonder tree) | Nimbolide[88] | Antiproliferative effect on human cancel lines[88] |
| 13 | Bacopa monnieri(Indian penny wort) | bacoside A and B[89]stigmasterol [90] | Antitumor against Ehrlich Ascites carcinoma in mice[90] |
| 14 | Berberis aristate(Indian ophthalmic barberry) | Methanolic extract | Cytotoxic activity in MCF7 cell line [91] |
| 15 | Calotropis gigantea R. Br(Gigantic swallow wort) | Alcoholic extract, Lupeol | Anti-cervical cancer activity [92] |
| 16 | Calotropis procera R. Br(Crown floer) | Asclepin, Alcoholic extract | Antiproliferative activity [93] |
| 17 | Cassia fistula(Golden shower tree) | Methanolic extract | Antitumor activities against Ehrlich ascites carcinoma [94] |
| 18 | Carum roxburghianum Kurz(Azowan) | Monoterpene hydrocarbon | Cytotoxic in the brine shrimp lethality assays [95] |
| 19 | Corallocarpus epigaeus (Onion) | Methanolic extract | Cytotoxic activity against human breast adenocarcinoma (MCF7) and human colon carcinoma (HT-29) [96] |
| 20 | Crataeva nurvala(Three leaces caper) | Methanol extract, Lupeol[97] | Cytotoxic activity in brine shrimp lethality bioassay [98] |
| 21 | Curcuma longa(Tumeric) | Curcumin I-III [43,99] | Potent inhibitor of Loekotriene B4 formation in rat peritoneal polymorphonuclear neutrophils (PMNL) [43,99] |
| 22 | Curcuma zedoaria(White turmeric) | Curcuminoids [100] Isocurcumenol [101] |
Cytotoxic against human ovarian cancer OVCAR-3 cells [100] |
| 23 | Cymbopogon citrates(Lemongrass) | Citral [102] | Induced apoptosis in caspase-3 enzymatic activity |
| 24 | Cinnamomum cassia(Cinnamon bark) | Aqueous extract, 2'-Hydroxycinnamaldehyde (HCA)[103] | Induced apoptosis in human cervical cancer line (SiHa) [104] |
| 25 | Datura metel L.(Angel’s trumpet) | Withanolides [105] daturametelins H–J [106] |
Cytotoxic activities agains A549 (lung), BGC-823 (gastric) and K562 (leukemia) cancer cell lines [105] |
| 26 | Euphorbia neriifolia L(Indain spurge tree) | Hydro-ethanolic extract | Chemopreventive effect against DENA-induced renal carcinogenesis in mice [107] |
| 27 | Elephantopus scaber(Elephant’s foot) | Deoxyelephantopin (ESD) [108] Elescaberin, isodeoxyelephantopin, Deoxyelephantopin [109,110] |
Antineoplastic effects of a sesquiterpene lactone on lung adenocarcinoma (A549) cells [109,110] |
| 28 | Ficus glomerata(Goolar fig) | Ethanolic extract | Anticancer activities in mammary carcinoma DMBA induced rats [111] |
| 29 | Madhuca indica(Butter tree) | Ethanolic extract | Cytotoxicity against ling (A-549), colon (502713 HT-29) and neuroblastima (IMR-32) cell line [112] |
| 30 | Mallotus philippinensis Muell. Arg (Kamala tree) | 3alpha-hydroxy-D:A-friedooleanan-2-one [113], Ethanolic extract with Rottlerin [114,115] |
Cytotoxic activity on human cancer cell lines [116] |
| 31 | Saraca indica(Ashoka tree) | 7,12-dimethyl benz(a)anthracene [117] | Chemopreventive property in skin cancer in mice models [117] |
| 32 | Emblica officinalis,Gaertn, | pyrogallol [118]7, 12-dimethyabenz(a)anthrecene [119] Cyclophosphamide (CP) [120] | Chemopreventive property on DMBA induced skin tumorigenesis in Swiss albino mice [119] |
| 33 | Urginea indica (Indian squill/ wild onion) | 29k Da glycoprotein[121] | Antitumor activity against ascites tumor, mouse mammary carcinoma [121] |
| 34 | Taxus buccata(Himalyan yew) | Taxol[122], taxotere | Cytotoxic against breast, lung, ovarian, colorectal cancer and melanoma tumor colony [123] |
| 35 | Withania somnifera(Indian ginseng)[124] | Withaferin A[55] Viscosalactone B[59] |
Antitumor activity on S-180 in BALB/c mice [124], antiproliferative activity on NCL-H460 (lung), HCT-116 (colon), SF-268 (central nervous system;CNS and MCF-7(breast) human tumor cell lines [59] |
| 36 | Xantium strumarium(Burdock datura)[125] | Xanthatin and xanthinosin[126] | Cytotoxicity in the human cancer cell lines WiDr ATCC (colon), MDA-MB-231 ATCC (breast) and NCI-417 (lung) [126], Cytotoxic effects on the human cell line, HL-60 [127] |
Table 2: List of pharmaceutical drug leads derived from Ayurvedic medicinal plants.
Several molecules derived from plants with Ayurvedic importance are the lead compounds for important drugs that are being used to treat cancer and immune related diseases. For example; taxol, roscovitine, combretastatin A-4, betulinic acid, silvestrol, camptothecin, podophyllotoxin, topotecan, irintecan, vincristine, vinblastin and flavopiridol are some of the potential drug leads in the treatment of different cancer types [30].
Taxanes are unique class of anticancer agents that exert cytotoxic activity againt cancer cells with specific mechanism. Many Taxus species have been claimed to be used in treatment of cancer in Ayurveda practices and also by Native American tribes. Paclitaxel (Taxol) is the first taxane anticancer drug, isolated from bark of Taxus brevifolia (Pacific yew), received regulatory approval in many countries for ovarian and breast cancer treatment [31]. Subsequently, paclitaxel and many other precursors have been reported in many Taxus species. Furthermore, 23 taxanes are in preclinical trials for treatment of cancer [32]. In recent years, paclitaxel has attracted attention in treatmet of multiple sclerosis, psoriasis and rheumatoid arthritis [33].
Flavopiridol (alvocidib) is a semisynthetic flavonoid precursor of rohitukine extracted from Dysoxylum binectariferum [34], widely used in Ayurvedic medicine. Flavopiridol showed significant inhibition against cyclin-dependent kinase CDK 1, CDK 2,CDK 4 and CDK 7 [34,35]. Due to its exceptional ability to suppress lung carcinoma, breast cancer carcinoma, multiple myeloa and head and neck squamous cell carcinoma, this molecule has entered into clinical trials. More than 60 clinical trials (Phase I and II) have been carried out between years 1998- 2014 [36,37]. Despite its potent in vitro activities and extensive investment in these trials, there are no Phase III studies reported [38] to date.
Curcumin is a hydrophobic polyphenol compound derived from curcuma longa, commonly known as turmeric is consumed in regular culinary [39]. Traditionally, turmeric is commonly used in the treatment of microbial diseases, stomach and liver ailments. Phytochemical evaluation of turmeric revealed two major constituents demethoxycurcumin (DMC) and bisdemethoxycurcumin (BDMC), apart from curcumin [40]. In vitro and in vivo studies have demonstrated that curcumin is a potent anti-tumorigenic agent [41,42] against different cancer types including colon, skin, duodenum and stomach. Curcumin is considered as noble chemopreventive and antitumor agent with its multiple targeting property without side effects even at high dose [41-43].
On the contrary, poor bioavailability, solubility and absorption hindered its approval as chemotherapeutic agent [39]. Recent studies showed that curcumin posses in vitro anti-angiogenic and in vivo antitumor properties through combined phosphodiesterases- PDE2 and PDE3 inhibition [44]. Furthermore, DMC induced the expression of promoter of methylated genes more than cumin in leukemia cells and on combination could give optimum re-expression of epigenetically silenced genes [45,46]. The ongoing research outcomes provide strong indication that curcumin will be a potenail anticancer chemotherapy agent derived from Ayurvedic herb.
Andrographis paniculata Nees commonly known as ‘King of Bitters’ (Kalmeg ) in Ayurveda [47]. Kalmeg is distributed throughout South India and Srilanka displayed broad spectrum of activities including anticarcinogenic, anti HIV and several other pharmacological activities [47]. Pharmaceutical constituents including andrographolide, neoandrographolide and dehydroandrographolide have been shown to possess anti-cancer properties [48]. Andrographolide being most active compound from kalmeg has shown anticancer properties in several in vitro and in vivo studies against B16F0 melanoma syngeneic and HT-29 xenograft models [47] , 2-cell line panel containing MCF-7 (breast cancer cell line) and HCT-116 (colon cancer cell line)[49], multiple myeloma [50,51], rats induced with gastric ulcer [52]. In one of the human study commenced by Darryl and co-authors, ingestion of A. paniculata at a dose of 500 mg twice daily along with other nutraceuticals by 20 patients with late stage cancer in different parts showed significant improvement in the patients [53]. However, the poor oral biovailability has remained a major setback [54].
Withania somnifera is commonly known as “Ashwagandha”, widely used in Ayurveda for treatment of arthritis, menstrual cycle and uterus related disorders, cancer and other inflammatory diseases [55]. Previous in vivo studies demonstrated antitumor properties of roots of Aswagandha against Sarcoma-180 solid tumor with low toxicity [56]. Withaferin A is a most abundant bioactive constituent of W. somnifera and received a marked interest globally for its exceptional anticancer and anti-inflammatory properties [57].
Withaferin A inhibits Notch-1 signalling and down regulates pro survival pathways such as Akt/NF-kB/Bcl-2, in HCT-116, SW-480 and SW-620 cancer cell lines [58]. Also other in vivo studies suggest antiproliferative activity on NCL-H460 (lung), HCT-116 (colon), SF-268 (central nervous system; CNS and MCF-7 (breast) human tumor cell lines [59]. Recent studies conducted by Li Xu and coauthors [60] suggest the synergistic antitumor activity of withaferin A combined with oxaliplatin.
Withaferin A enhanced oxaliplatin induced growth suppression and apoptosis in PC cells via mitochondrial dysfunction and inactivation of the P13K/AKT pathway [60]. Withaferin A is of particular interst due to its ability to interact and inhibit different cancer-specific pathways with least toxic effects.
Market share of Ayurvedic medicine in the pharmaceutical industry
Natural products derived from plants, animals and other sources have been pivotal in treatment of human diseases. Ayurvedic medicine has significant history in this respect and there is an ongoing demand due to their efficacy, low toxicity and fewer side effects. These positive attributes have led to mushrooming of Ayurvedic medical practices and related herbal based drug manufacturing companies worldwide.
The market value for Ayurvedic herbs and their derivatives is growing annually at 20% and the sales have increased by 25% in the last 10 years. To date, China and India are major sources of herbal products. In the global market, China shares 13% of total market whereas India shares only 2.5% [61]. Remarkably, Traditional Chinese medicinal (TCM) system comprises 5000 plant species while Ayurvedic medicinal system uses 7000 plant species [62]. According to Export / Import Bank, TCM plants have a global trade value of US $6 billion, while Ayurvedic medicine have only a share of US $1 billion. The trade of Ayurvedic products are expected to increase rapidly in the near future, due to the fact that a number of dugs with high efficacy are primarily derived by the utilization of realm of traditional Ayurvedic knowledge.
The trade of Ayurvedic medicine is mainly being affected by poor quality control practices, lack of efficient agricultural practices, lack of knowledge on the global marketing strategies and standardization of processes and services. The projection made by WHO states that the global herbal market would grow to $5 trillion by 2050 from the current market level of $62 billion [61]. The effort from ‘different associations like National Medicinal Plants Board (NMPB), Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy (AYUSH), World Health organization (WHO) in India, USA, UK, Russia, Germany, Hungary and South Africa are now yielding good results in promoting Ayurveda which has opened-up new opportunities [63].
Implications of using Ayurvedic medicine
Ayurvedic medicine system is a very ancient and is now practiced throughout the world. The Ayurvedic medicine preparations are formulated by a combination of medicinal plants, animal products and minerals and metals including gold, copper, lead, mercury, iron and zinc [64]. These metals are primarily added to herbal products as ashes or bhasmas, with a belief that they act as catalyst and improves the target specificity. However, Ayurvedic practioners often prescribe medicine which do not meet the criteria of modern GMP or manufactured by practitioners themselves. According to Centre for Disease Control, during the years between 2000 – 2003, 12 cases were reported with lead toxication after consumption of Ayurvedic products [65]. Strict regulations for Ayurvedic preparations are therefore expected to minimize adverse effects and improve the acceptance of these medicine by global communities.
Many herbal supplements that are available in the market are subjected to limited regulations. Individuals consume these herbal products as dietary supplements without proper knowledge of pros and cons and hence often affected by toxic effects. In a case study of a 69-year-old Caucasian male retired lawyer consumed ‘Bhasma’ an ayurvedic herbal medication on family advice while traveling in India. He reported illness of being lethargy, fatigue, memory impairment, generalized weakness, severe constipation, anorexia and weight loss of 18 kg over preceding eight months. After thorough clinical investigations, discontinuation of Ayurvedic Bhasmas and chelation therapy treatment helped him to recover from these issues [66].
Chemical constituents of plants can be influenced by several factors including habitat, cultivation site, seasonal variations, temperature, soil composition, water availability and pollutant levels in the atmosphere. Furthermore, physicians prescribe different plant species for specific symptoms due to morphological similarities. For instance, Shankhpushpi is herbal drug widely used in the treatment of epilepsy, leucoderma, bronchitis and teething problems. This drug is sourced from three plant species, namely, Clitoria ternatea , Convolvulus pluricaulis and Evolvulus alsinoides in different regions of the country [67]. In fact, the chemical consitutents of these plants are significantly distinct from one another. Due to ever increasing demand for Shankhpushpi and other important herbal products, the preparations are often altered with other plant material. Phytochemical investigations suggest that over 60 % herbal products available in the market are adulterated [68].
In order to supply quality herbral products for better health, there is a requirement of standardized authentication of herbs. For instance, rigourous morphological analysis and quantification of molecular markers can be used as an effective means of identification of plants. It is therefore essential that the regulations on authentication of plant material must be strictly implemented in order to minimize adverse effects due to adultration of herbal medicine and also to gain the desired health benefits.
Interface between Ayurveda and modern medicine
In the realm of moder drug discovery, traditional knowledge of Ayurvedic medicinal plants is playing pivotal role. There has been significant correlation between the use of herbs for particular symptoms and the targets of derived drugs. Anticancer drugs derived from Ayurvedic medicinal plants exert their activity by means of activation or inactivation of signaling pathways [69]. Oncogenes, cancer growth factors, cancer promoting enzymes, protein kinases have been identified as major targets in drug discovery and development process [70]. Thousands of years ago, Ayurvedic medicinal system used many medicinal plants in the treatment of cancer (when there was no modern medicinal knowedge existed). Drugs derived from many of these traditional plants are now well established inhibitors of the targets responsible for different cancers. For instance, Vinca rosea and Taxus species were widely used in the treatment of different cancer types [71]. Vincristine and paclitaxel isolated from these plants showed strong anticancer properties. [71]. These compounds are now available in the drug market.
Modern cancer treatment typically involves administration of a single therapeutic agents into human system. These agents usually lack specificity to the target or multiple targets, leads to apoptosis of healthy cells and causes adverse side effects. Toxicity and side effects remained to be major setbacks in chemotherapeutic approaches to cancer treatment. For example, anticancer drugs, including vincristine and paclitaxel, are responsible for peripheral neuropathy during cancer treatment [71].
Typical Ayurveda treatment involes adminstration of an individual or mixture of different plant extracts. Ayurveda recommends formulation (multiple plants at different proportions) to obtain synergism and diminish drug associated side effects such as cachexia (including nausea, wait loass and anorexia). For instance, W. sominifera, Sida cordifolia, Vitis vinifera, Plumbago zeylanci, Tinospora cordifolia Asparagus racemosa and Zingiber officinale are often used to improve apetite, malnutrition, body resistance and fatigue. In addition, Ayurvedic treatment incorporates yoga and relaxation therapies which provide spiritual well-being of the patient. The effectiveness of these holistic approaches goes beyond the symptom relief and improves physiological and behavioral aspects of the patient.
Owing to these benefits. modern cancer treatments are gradually adapting combinatorial approaches including yoga, meditation, mindpositive thinking and cognitive practices along with chemotherapy. The case of Anita Moorjani’s experience with lymphoma evidences role of mind and positive thinking in curing diseases[72]. Anita underwent many conventional chemotherapy cancer treatments. During the cancer treatment she fell into deep coma for several days and claimed to have had near death experience and out-of-body experience [72]. As the lymphoma had metastasized throughout her body and her death was confirmed. Subsequently, Anita cam e out of coma surviving from cancer, claiming that it was only possible through spontaneous healing developed from positive thinking attitude [33]. Meditation, yoga and prayers have been practiced in Ayurvedic treatment to develop mindbody control [33]. Furthermore, a study conducted by Özlem Ülger and co-authors evidednced improved health conditions in cancer patients after yoga practices [65]. These observations suggest that a revolutionized approach can be devised through integration of Ayurvedic practices with modern day treatments for enhanced efficacy of cancer therapies.
Conclusion
The quest for pharmaceutical drug leads from Ayurvedic medicinal plants has been rapidly growing. The prime reason for this interest is: medicinal plants are cost effective, reliable and posses least side effects. However, ever growing requirement of medicinal plants often leads to cultivation of malpractices. In this respect, educating the communities about correct procedures of collecting, extracting, handling and storing of herbal material, and strict implementation of regulations on quality control would minimize wrong practices and improve the grade of the products and their efficiency. Furthermore, the toxicity and safety assessment procedures for these herbal medicines should be conducted using modern analytical techniques and tools for their improved efficacy. Many international authorities and agencies including the WHO, European Agency for the Evaluation of Medicinal Products and European Scientific Cooperation of Phytomedicine, US Agency for Health Care Policy and Research, European Pharmacopeia Commission and the Department of Indian System of Medicine have initiated developing and implementing new and effective strategies for regulating quality control and standardization of herbal medicine. In addition, appropriate global marketing strategies would boost the usage and economic value of Ayurvedic medicinal plants.
References
- Lad V (1984) Ayurveda: The science of self-healing: A practical guide: Lotus press.
- Verhoef MJ, Lewith G, Ritenbaugh C, Boon H, Fleishman S, et al. (2005) Complementary and alternative medicine whole systems research: beyond identification of inadequacies of the RCT. See comment in PubMed Commons below Complement Ther Med 13: 206-212.
- Ganeshrao BN, Somaji LD, Shrikrishna PA (2014) International Journal of Ayurveda and Pharma Research. Int J Ayur Pharma Research 2: 101-110.
- Lokhande P, Jagdale S, Chabukswar A (2006) Natural remedies for heart diseases. Indian J Tradit Know 5: 420-427
- Krunal D, Rabinarayan A (2013) Therapeutic importance of Eranda (Ricinus communis Linn.) in Ayurveda-a Review. Ayurpharm Int J Ayur Alli Sci 2: 281-295.
- Schmidt LM (2004) Herbal remedies: the other drugs your patients take. See comment in PubMed Commons below Home Healthc Nurse 22: 169-175.
- Ramawat KG, Goyal S (2008) The Indian herbal drugs scenario in global perspectives. Bioactive Molecules and Medicinal Plants: Springer. pp. 325-347.
- Balachandran P, Govindarajan R (2005) Cancer--an ayurvedic perspective. See comment in PubMed Commons below Pharmacol Res 51: 19-30.
- Singh RH (2002) An assessment of the ayurvedic concept of cancer and a new paradigm of anticancer treatment in Ayurveda. See comment in PubMed Commons below J Altern Complement Med 8: 609-614.
- Rastogi S (2014) Ayurvedic Principles of Food and Nutrition: Translating Theory into Evidence-Based Practice. Ayurvedic Science of Food and Nutrition: Springer. pp. 3-14.
- Sumantran VN, Tillu G (2012) Cancer, inflammation, and insights from ayurveda. See comment in PubMed Commons below Evid Based Complement Alternat Med 2012: 306346.
- Aggarwal BB, Sung B, Gupta SC (2014) Inflammation and Cancer: Springer.
- Lindsey Torre M, Rebecca Siegel M, Ahmedin Jemal D (2015) American Cancer Society. Global Cancer Facts & Figures. Atlanta: American Cancer Society 3.
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, et al. (2015) Global cancer statistics, 2012. See comment in PubMed Commons below CA Cancer J Clin 65: 87-108.
- Van Cutsem E, Köhne C-H, Hitre E, Zaluski J, Chang Chien C-R, et al. (2009) Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med 360: 1408-1417.
- Chain E, Florey HW, Gardner AD, Heatley NG, Jennings MA, et al. (1940) Penicillin as a chemotherapeutic agent. The lancet 236: 226-228.
- Guzmán M (2003) Cannabinoids: potential anticancer agents. See comment in PubMed Commons below Nat Rev Cancer 3: 745-755.
- Reya T, Morrison SJ, Clarke MF, Weissman IL (2001) Stem cells, cancer, and cancer stem cells. See comment in PubMed Commons below Nature 414: 105-111.
- Â Partridge AH, Burstein HJ, Winer EP (2000) Side effects of chemotherapy and combined chemohormonal therapy in women with early-stage breast cancer. J Natl Cancer Inst Monogr 30: 135-142.
- Satyavati GV, Raina MK, Sharma M (1976) Medicinal plants of India: Indian council of medical research New Delhi.
- Sinha R, Anderson DE, McDonald SS, Greenwald P (2003) Cancer risk and diet in India. See comment in PubMed Commons below J Postgrad Med 49: 222-228.
- Park EJ1, Pezzuto JM (2002) Botanicals in cancer chemoprevention. See comment in PubMed Commons below Cancer Metastasis Rev 21: 231-255.
- Taviad K, Galib PB, Patgiri BJ, Prajapati PK Metal toxicity due to Ayurvedic drugs-Facts and Myths.
- Jain AK, Sharma BK Developments in the field of ayurveda-past to present.
- Ramawat KG, Jain S, Suri SS, Arora DK (1998) Aphrodisiac plants of Aravalli Hills with special reference to safed musli. Role of biotechnology in medicinal and aromatic plants 1: 210-223.
- Kamboj VP (2000) Herbal medicine. Current science-Bangalore- 78: 35-38.
- Dutta S (2015) Natural sources as potential anti-cancer agents: A review.
- Caltagirone S, Rossi C, Poggi A, Ranelletti FO, Natali PG, et al. (2000) Flavonoids apigenin and quercetin inhibit melanoma growth and metastatic potential. See comment in PubMed Commons below Int J Cancer 87: 595-600.
- Dragsted LO, Strube M, Larsen JC (1993) Cancer-protective factors in fruits and vegetables: biochemical and biological background. See comment in PubMed Commons below Pharmacol Toxicol 72 Suppl 1: 116-135.
- Salim AA, Chin Y-W, Kinghorn AD (2008) Drug discovery from plants. Bioactive molecules and Medicinal plants: Springer. pp. 1-24.
- Wheeler NC, Jech K, Masters S, Brobst SW, Alvarado AB, et al. (1992) Effects of genetic, epigenetic, and environmental factors on taxol content in Taxus brevifolia and related species. See comment in PubMed Commons below J Nat Prod 55: 432-440.
- Colegate SM, Molyneux RJ (2007) Bioactive natural products: detection, isolation, and structural determination .(2nd edn), CRC press.
- Ebers GC1 (1994) Treatment of multiple sclerosis. See comment in PubMed Commons below Lancet 343: 275-279.
- Mohanakumara P1, Sreejayan N, Priti V, Ramesha BT, Ravikanth G, et al. (2010) Dysoxylum binectariferum Hook.f (Meliaceae), a rich source of rohitukine. See comment in PubMed Commons below Fitoterapia 81: 145-148.
- Â Ali S, Heathcote DA, Kroll SHB, Jogalekar AS, Scheiper B, et al. (2009) The development of a selective cyclin-dependent kinase inhibitor that shows antitumor activity. Cancer research 69: 6208-6215
- Phelps MA, Lin TS, Johnson AJ, Hurh E, Rozewski DM, et al. (2009) Clinical response and pharmacokinetics from a phase 1 study of an active dosing schedule of flavopiridol in relapsed chronic lymphocytic leukemia. See comment in PubMed Commons below Blood 113: 2637-2645.
- Shindiapina P, Brown JR, Danilov AV (2014) A new hope: novel therapeutic approaches to treatment of chronic lymphocytic leukaemia with defects in TP53. See comment in PubMed Commons below Br J Haematol 167: 149-161.
- Asghar U, Witkiewicz AK2, Turner NC3, Knudsen ES2 (2015) The history and future of targeting cyclin-dependent kinases in cancer therapy. See comment in PubMed Commons below Nat Rev Drug Discov 14: 130-146.
- Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB (2007) Bioavailability of curcumin: problems and promises. See comment in PubMed Commons below Mol Pharm 4: 807-818.
- Himesh S, Sharan PS, Mishra K, Govind N, Singhai A (2011) Qualitative and quantitative profile of curcumin from ethanolic extract of Curcuma longa. Int Res J Pharm 2: 180-184.
- Shankar S, Ganapathy S, Chen Q, Srivastava RK (2008) Curcumin sensitizes TRAIL-resistant xenografts: molecular mechanisms of apoptosis, metastasis and angiogenesis. Mol Cancer 7: 7-16.
- Shankar S, Chen Q, Sarva K, Siddiqui I, Srivastava RK (2007) Curcumin enhances the apoptosis-inducing potential of TRAIL in prostate cancer cells: molecular mechanisms of apoptosis, migration and angiogenesis. J Mol Signal 2: 10.
- Shankar S, Srivastava RK (2007) Bax and Bak genes are essential for maximum apoptotic response by curcumin, a polyphenolic compound and cancer chemopreventive agent derived from turmeric, Curcuma longa. Carcinogenesis 28: 1277-1286.
- Abusnina A, Keravis T, Zhou Q, Justiniano H, Lobstein A, et al. (2015) Tumour growth inhibition and anti-angiogenic effects using curcumin correspond to combined PDE2 and PDE4 inhibition. See comment in PubMed Commons below Thromb Haemost 113: 319-328.
- Yu J, Peng Y, Wu LC, Xie Z, Deng Y, et al. (2013) Curcumin down-regulates DNA methyltransferase 1 and plays an anti-leukemic role in acute myeloid leukemia. See comment in PubMed Commons below PLoS One 8: e55934.
- Hassan HE, Carlson S, Abdallah I, Buttolph T, Glass KC, et al. (2015) Curcumin and dimethoxycurcumin induced epigenetic changes in leukemia cells. See comment in PubMed Commons below Pharm Res 32: 863-875.
- Rajagopal S, Kumar RA, Deevi DS, Satyanarayana C, Rajagopalan R (2003) Andrographolide, a potential cancer therapeutic agent isolated from Andrographis paniculata. See comment in PubMed Commons below J Exp Ther Oncol 3: 147-158.
- Lim JC, Chan TK, Ng DS, Sagineedu SR, Stanslas J, et al. (2012) Andrographolide and its analogues: versatile bioactive molecules for combating inflammation and cancer. See comment in PubMed Commons below Clin Exp Pharmacol Physiol 39: 300-310.
- Jada SR, Matthews C, Saad MS, Hamzah AS, Lajis NH, et al. (2008) Benzylidene derivatives of andrographolide inhibit growth of breast and colon cancer cells in vitro by inducing G arrest and apoptosis. See comment in PubMed Commons below Br J Pharmacol 155: 641-654.
- Matsuda T, Kuroyanagi M, Sugiyama S, Umehara K, Ueno A, et al. (1994) Cell differentiation-inducing diterpenes from Andrographis paniculata Nees. See comment in PubMed Commons below Chem Pharm Bull (Tokyo) 42: 1216-1225.
- Gunn EJ, Williams JT, Huynh DT, Iannotti MJ, Han C, et al. (2011) The natural products parthenolide and andrographolide exhibit anti-cancer stem cell activity in multiple myeloma. See comment in PubMed Commons below Leuk Lymphoma 52: 1085-1097.
- Saranya P, Geetha A, Selvamathy SM (2011) A biochemical study on the gastroprotective effect of andrographolide in rats induced with gastric ulcer. See comment in PubMed Commons below Indian J Pharm Sci 73: 550-557.
- See D, Mason S, Roshan R (2002) Increased tumor necrosis factor alpha (TNF-alpha) and natural killer cell (NK) function using an integrative approach in late stage cancers. See comment in PubMed Commons below Immunol Invest 31: 137-153.
- Ye L, Wang T, Tang L, Liu W, Yang Z, et al. (2011) Poor oral bioavailability of a promising anticancer agent andrographolide is due to extensive metabolism and efflux by P-glycoprotein. See comment in PubMed Commons below J Pharm Sci 100: 5007-5017.
- Devi PU (1996) Withania somnifera Dunal (Ashwagandha): potential plant source of a promising drug for cancer chemotherapy and radiosensitization. See comment in PubMed Commons below Indian J Exp Biol 34: 927-932.
- Devi PU, Akagi K, Ostapenko V, Tanaka Y, Sugahara T (1996) Withaferin A: a new radiosensitizer from the Indian medicinal plant Withania somnifera. See comment in PubMed Commons below Int J Radiat Biol 69: 193-197.
- Devi PU, Akagi K, Ostapenko V, Tanaka Y, Sugahara T (1996) Withaferin A: a new radiosensitizer from the Indian medicinal plant Withania somnifera. See comment in PubMed Commons below Int J Radiat Biol 69: 193-197.
- Koduru S, Kumar R, Srinivasan S, Evers MB, Damodaran C (2010) Notch-1 inhibition by Withaferin-A: a therapeutic target against colon carcinogenesis. See comment in PubMed Commons below Mol Cancer Ther 9: 202-210.
- Jayaprakasam B1, Zhang Y, Seeram NP, Nair MG (2003) Growth inhibition of human tumor cell lines by withanolides from Withania somnifera leaves. See comment in PubMed Commons below Life Sci 74: 125-132.
- Li X, Zhu F, Jiang J, Sun C, Wang X, et al. (2015) Synergistic antitumor activity of withaferin A combined with oxaliplatin triggers reactive oxygen species-mediated inactivation of the PI3K/AKT pathway in human pancreatic cancer cells. Cancer letters 357: 219-230.
- Bhattacharya R, Reddy KRC, Mishra AK (2014) Export strategy of Ayurvedic Products from India. Intern J Ayurvedic Med 5.
- Verma S, Singh S (2008) Current and future status of herbal medicines. Veterinary world 1: 347-350.
- Chaudhary A, Singh N (2011) Contribution of world health organization in the global acceptance of Ayurveda. See comment in PubMed Commons below J Ayurveda Integr Med 2: 179-186.
- Saper RB, Kales SN, Paquin J, Burns MJ, Eisenberg DM, et al. (2004) Heavy metal content of ayurvedic herbal medicine products. See comment in PubMed Commons below JAMA 292: 2868-2873.
- Centers for Disease Control and Prevention (CDC) (2004) Lead poisoning associated with ayurvedic medications--five states, 2000-2003. See comment in PubMed Commons below MMWR Morb Mortal Wkly Rep 53: 582-584.
- Breeher L, Gerr F, Fuortes L (2013) A case report of adult lead toxicity following use of Ayurvedic herbal medication. See comment in PubMed Commons below J Occup Med Toxicol 8: 26.
- Ganie SH, Ali Z, Das S, Srivastava PS, Sharma MP (2015) Identification of Shankhpushpi by morphological, chemical and molecular markers. European J Biotechnol Biosci 3: 01-09.
- Garlic A (2004) The impediments preventing India from becoming a herbal giant. Current Science 87: 275.
- Garodia P, Ichikawa H, Malani N, Sethi G, Aggarwal BB (2007) From ancient medicine to modern medicine: ayurvedic concepts of health and their role in inflammation and cancer. See comment in PubMed Commons below J Soc Integr Oncol 5: 25-37.
- Cohen P (2002) Protein kinases--the major drug targets of the twenty-first century? See comment in PubMed Commons below Nat Rev Drug Discov 1: 309-315.
- Cragg GM, Newman DJ (2005) Plants as a source of anti-cancer agents. See comment in PubMed Commons below J Ethnopharmacol 100: 72-79.
- Moorjani A (2012) Dying to be me: My journey from cancer, to near death, to true healing: Hay House, Inc.
- Jena GB, Nemmani KV, Kaul CL, Ramarao P (2003) Protective effect of a polyherbal formulation (Immu-21) against cyclophosphamide-induced mutagenicity in mice. See comment in PubMed Commons below Phytother Res 17: 306-310.
- Huseini HF, Alavian SM, Heshmat R, Heydari MR, Abolmaali K (2005) The efficacy of Liv-52 on liver cirrhotic patients: a randomized, double-blind, placebo-controlled first approach. See comment in PubMed Commons below Phytomedicine 12: 619-624.
- Parasuraman S, Thing GS, Dhanaraj SA (2014) Polyherbal formulation: Concept of ayurveda. Pharmacognosy reviews 8: 73.
- Lee CC, Houghton P (2005) Cytotoxicity of plants from Malaysia and Thailand used traditionally to treat cancer. See comment in PubMed Commons below J Ethnopharmacol 100: 237-243.
- Kwak DH, Park JH, Lee HS, Moon JS, Lee S (2014) Aristolochic Acid I induces ovarian toxicity by inhibition of akt phosphorylation. See comment in PubMed Commons below Chem Res Toxicol 27: 2128-2135.
- Sreelatha S, Padma PR, Umasankari E (2011) Evaluation of anticancer activity of ethanol extract of Sesbania grandiflora (Agati Sesban) against Ehrlich ascites carcinoma in Swiss albino mice. J Ethnopharmacol 134: 984-987.
- Melek FR, Miyase T, Ghaly NS, Nabil M (2007) Triterpenoid saponins with N-acetyl sugar from the bark of Albizia procera. See comment in PubMed Commons below Phytochemistry 68: 1261-1266.
- Haque N, Chowdhury SA, Nutan MT, Rahman GM, Rahman KM, et al. (2000) Evaluation of antitumor activity of some medicinal plants of Bangladesh by potato disk bioassay. See comment in PubMed Commons below Fitoterapia 71: 547-552.
- Wargovich MJ (1987) Diallyl sulfide, a flavor component of garlic (Allium sativum), inhibits dimethyihydrazine-induced colon cancer. Carcinogenesis 8: 487-489.
- Pecere T, Gazzola MV, Mucignat C, Parolin C, Dalla Vecchia F, et al. (2000) Aloe-emodin is a new type of anticancer agent with selective activity against neuroectodermal tumors. Cancer research 60: 2800-2804.
- Zongwei W, Yong W, Zhaosheng H, Shiqing Z, Yina W, et al. (2001) Study on Antitumor Effect and Mechanism of Aloe Polysaccharids [J]. J Chin Med Mater 5: 019.
- Â Kamarajan P, Ramamurthy N, Govindasamy S (1995) In Vitro Evaluation of the Anti-Cancer Effects of Echitamine Chloride on Fibrosarcoma Cells. J Clin Biochem Nutr 18: 65-71.
- Jagetia GC, Baliga MS, Venkatesh P (2003) Effect of Sapthaparna (Alstonia scholaris Linn) in modulating the benzo(a)pyrene-induced forestomach carcinogenesis in mice. See comment in PubMed Commons below Toxicol Lett 144: 183-193.
- Ansil PN, Wills PJ, Varun R, Latha MS (2014) Cytotoxic and apoptotic activities of Amorphophallus campanulatus tuber extracts against human hepatoma cell line. Res Pharm Sci 9: 269.
- Chan LL, George S, Ahmad I, Gosangari SL, Abbasi A, et al. (2011) Cytotoxicity Effects of Amoora rohituka and chittagonga on Breast and Pancreatic Cancer Cells. See comment in PubMed Commons below Evid Based Complement Alternat Med 2011: 860605.
- Roy MK, Kobori M, Takenaka M, Nakahara K, Shinmoto H, et al. (2007) Antiproliferative effect on human cancer cell lines after treatment with nimbolide extracted from an edible part of the neem tree (Azadirachta indica). See comment in PubMed Commons below Phytother Res 21: 245-250.
- Deepak M, Amit A (2004) The need for establishing identities of 'bacoside A and B', the putative major bioactive saponins of Indian medicinal plant Bacopa monnieri. See comment in PubMed Commons below Phytomedicine 11: 264-268.
- Ghosh T, Maity TK, Singh J (2011) Evaluation of antitumor activity of stigmasterol, a constituent isolated from Bacopa monnieri Linn aerial parts against Ehrlich Ascites Carcinoma in mice. Orient Pharm Exp Med 11: 41-49.
- Mazumder PM, Das S, Das MK (2010) Cytotoxic Activity of Methanolic Extracts of Berberis aristata DC and Hemidesmus indicus R. Br. in MCF7 Cell Line. J Current Pharm Res 1: 12-15.
- Sureshkumar P, Senthilraja P, Kalavathy S (2012) In-Silico Docking Analysis of Calotropis gigantea (L.) R. Br Derived Compound against Anti-Cervical Cancer Activity. World Research Journal of Computer-Aided Drug Design 1: 9-12
- Magalhães HI, Ferreira PM, Moura ES, Torres MR, Alves AP, et al. (2010) In vitro and in vivo antiproliferative activity of Calotropis procera stem extracts. See comment in PubMed Commons below An Acad Bras Cienc 82: 407-416.
- Gupta M, Mazumder UK, Rath N, Mukhopadhyay DK (2000) Antitumor activity of methanolic extract of Cassia fistula L. seed against Ehrlich ascites carcinoma. See comment in PubMed Commons below J Ethnopharmacol 72: 151-156.
- Paul BK, Saleh-e-In M, Mahamudul Hassan SM, Rahman Z, Saha GC, et al. (2013) Chemical Composition and Biological Activities of Carum roxburghianum Benth.(Radhuni) Seeds of Three Bangladeshi Ecotypes. J Essent Oil Bear Plants 16: 201-211.
- Bhavani MB, Leelavathi S (2015) Investigation on in vitro cytotoxic activity of a selected wild cucurbitaceae plant corallocarpus epigeaus against cancer. Int J Pharm Sci Rev Res 6: 3554.
- Saleem M (2009) Lupeol, a novel anti-inflammatory and anti-cancer dietary triterpene. See comment in PubMed Commons below Cancer Lett 285: 109-115.
- Ali MS, Dey A, Abu Sayeed M, Rahman AA, Kuddus MR, et al. (2014) In vivo sedative and cytotoxic activities of methanol extract of leaves of Crataeva nurvala Buch-Ham. See comment in PubMed Commons below Pak J Biol Sci 17: 439-442.
- Ammon HP, Anazodo MI, Safayhi H, Dhawan BN, Srimal RC (1992) Curcumin: a potent inhibitor of leukotriene B4 formation in rat peritoneal polymorphonuclear neutrophils (PMNL) See comment in PubMed Commons below Planta Med 58: 226.
- Syu WJ, Shen CC, Don MJ, Ou JC, Lee GH, et al. (1998) Cytotoxicity of curcuminoids and some novel compounds from Curcuma zedoaria. See comment in PubMed Commons below J Nat Prod 61: 1531-1534.
- Lakshmi S, Padmaja G, Remani P (2011) Antitumour effects of isocurcumenol isolated from Curcuma zedoaria rhizomes on human and murine cancer cells. Int J Med Chem .
- Dudai N, Weinstein Y, Krup M, Rabinski T, Ofir R (2005) Citral is a new inducer of caspase-3 in tumor cell lines. See comment in PubMed Commons below Planta Med 71: 484-488.
- Lee CW, Hong DH, Han SB, Park SH, Kim HK, et al. (1999) Inhibition of human tumor growth by 2'-hydroxy- and 2'-benzoyloxycinnamaldehydes. See comment in PubMed Commons below Planta Med 65: 263-266.
- Â Koppikar SJ, Choudhari AS, Suryavanshi SA, Kumari S, Chattopadhyay S, et al. (2010) Aqueous cinnamon extract (ACE-c) from the bark of Cinnamomum cassia causes apoptosis in human cervical cancer cell line (SiHa) through loss of mitochondrial membrane potential. BMC cancer 10: 210.
- Pan Y, Wang X, Hu X (2007) Cytotoxic withanolides from the flowers of Datura metel. See comment in PubMed Commons below J Nat Prod 70: 1127-1132.
- Ma L, Xie CM, Li J, Lou FC, Hu LH (2006) Daturametelins H, I, and J: three new withanolide glycosides from Datura metel L. See comment in PubMed Commons below Chem Biodivers 3: 180-186.
- Pracheta P, Sharma V, Singh L, Paliwal R, Sharma S, et al. (2011) Chemopreventive effect of hydroethanolic extract of Euphorbia neriifolia leaves against DENA-induced renal carcinogenesis in mice. See comment in PubMed Commons below Asian Pac J Cancer Prev 12: 677-683.
- Su M, Chung HY, Li Y (2011) Deoxyelephantopin from Elephantopus scaber L. induces cell-cycle arrest and apoptosis in the human nasopharyngeal cancer CNE cells. Biochemical and biophysical research communications 411: 342-347.
- Liang QL, Min ZD, Tang YP (2008) A new elemanolide sesquiterpene lactone from Elephantopus scaber. See comment in PubMed Commons below J Asian Nat Prod Res 10: 403-407.
- Kabeer FA, Sreedevi GB, Nair MS, Rajalekshmi DS, Gopalakrishnan LP, et al. (2013) Antineoplastic effects of deoxyelephantopin, a sesquiterpene lactone from Elephantopus scaber, on lung adenocarcinoma (A549) cells. See comment in PubMed Commons below J Integr Med 11: 269-277.
- Â Kumar VDR, Jayanthi G, Gurusamy K, Gowri S (2013) Antioxidant and anticancer activities of ethanolic extract of ficus glomerata roxb. in dmba induced rats. Int J Pharm Sci Res 4: 3087.
- Â Shaban A, Verma SK, Nautiyal R, Singh SK, Purohit R, et al. (2012) In vitro cytotoxicity of Madhuca indica against different human cancer cell lines. Int J Pharm Sci Res 3: 1385.
- Tanaka R, Nakata T, Yamaguchi C, Wada S, Yamada T, et al. (2008) Potential anti-tumor-promoting activity of 3alpha-hydroxy-D:A-friedooleanan-2-one from the stem bark of Mallotus philippensis. See comment in PubMed Commons below Planta Med 74: 413-416.
- Gschwendt M1, Müller HJ, Kielbassa K, Zang R, Kittstein W, et al. (1994) Rottlerin, a novel protein kinase inhibitor. See comment in PubMed Commons below Biochem Biophys Res Commun 199: 93-98.
- Maioli E, Torricelli C, Valacchi G (2012) Rottlerin and cancer: novel evidence and mechanisms. See comment in PubMed Commons below ScientificWorldJournal 2012: 350826.
- Â Sharma V (2011) A polyphenolic compound rottlerin demonstrates significant in vitro cytotoxicity against human cancer cell lines: isolation and characterization from the fruits of Mallotus philippinensis. J Plant Biochem Biotechnol 20: 190-195.
- Cibin TR1, Devi DG, Abraham A (2010) Chemoprevention of skin cancer by the flavonoid fraction of Saraca asoka. See comment in PubMed Commons below Phytother Res 24: 666-672.
- Khan MT, Lampronti I, Martello D, Bianchi N, Jabbar S, et al. (2002) Identification of pyrogallol as an antiproliferative compound present in extracts from the medicinal plant Emblica officinalis: effects on in vitro cell growth of human tumor cell lines. See comment in PubMed Commons below Int J Oncol 21: 187-192.
- Sancheti G, Jindal A, Kumari R, Goyal PK (2005) Chemopreventive action of emblica officinalis on skin carcinogenesis in mice. See comment in PubMed Commons below Asian Pac J Cancer Prev 6: 197-201.
- Haque R, Bin-Hafeez B, Ahmad I, Parvez S, Pandey S, et al. (2001) Protective effects of Emblica officinalis Gaertn. in cyclophosphamide-treated mice. See comment in PubMed Commons below Hum Exp Toxicol 20: 643-650.
- Deepak AV, Salimath BP (2006) Antiangiogenic and proapoptotic activity of a novel glycoprotein from U. indica is mediated by NF-kappaB and Caspase activated DNase in ascites tumor model. See comment in PubMed Commons below Biochimie 88: 297-307.
-  Strobel GA, Stierle A, Hess WM (1993) Taxol formation in yew—Taxus. Plant Sci 92: 1-12.
- Hanauske AR, Degen D, Hilsenbeck SG, Bissery MC, Von Hoff DD (1992) Effects of Taxotere and taxol on in vitro colony formation of freshly explanted human tumor cells. See comment in PubMed Commons below Anticancer Drugs 3: 121-124.
- Devi PU, Sharada AC, Solomon FE, Kamath MS (1992) In vivo growth inhibitory effect of Withania somnifera (Ashwagandha) on a transplantable mouse tumor, Sarcoma 180. See comment in PubMed Commons below Indian J Exp Biol 30: 169-172.
- . Kamboj A, Saluja AK (2010) Phytopharmacological review of Xanthium strumarium L.(Cocklebur). Int J Green Pharm 4: 129.
- Â RamÃrez-Erosa I, Huang Y, Hickie RA, Sutherland RG, Barl B (2007) Xanthatin and xanthinosin from the burs of Xanthium strumarium L. as potential anticancer agents This article is one of a selection of papers published in this special issue (part 2 of 2) on the Safety and Efficacy of Natural Health Products. Can J Physiol Pharmacol 85: 1160-1172.
- Nibret E, Youns M, Krauth-Siegel RL, Wink M (2011) Biological activities of xanthatin from Xanthium strumarium leaves. See comment in PubMed Commons below Phytother Res 25: 1883-1890.
Citation: Bhandari M, Ravipati AS, Reddy N, Koyyalamudi SR (2015) Traditional Ayurvedic medicines: Pathway to develop anti-cancer drugs. J Mol Pharm Org Process Res 3: 130. DOI: 10.4172/2329-9053.1000130
Copyright: ©2015 Koyyalamudi SR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 29810
- [From(publication date): 12-2015 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 27901
- PDF downloads: 1909