Tracking Progress in Anthropometric Failure among Children in India: A Geospatial Analysis
Received: 28-Jul-2020 / Accepted Date: 02-Sep-2020 / Published Date: 09-Sep-2020 DOI: 10.4172/2161-1165.1000389
Abstract
Background: This paper deals with three key indicators of anthropometric failure viz. stunting, wasting, and underweight, their significant correlates, and spatial dependence across 640 districts of India. The paper uses data from three different rounds of NFHS conducted from 1998 to 2015. The spatial analysis uses district-level information collected first time in NFHS-4 (2015-16).
Methods: Analytical methods used in this paper include multivariate logistic regression to examine the adjusted effects of various predictors and predicted probabilities to explain changes in the likelihood of anthropometric failures over time. Besides, bivariate LISA maps and spatial error models provide spatial dependence and clustering in anthropometric failures among children.
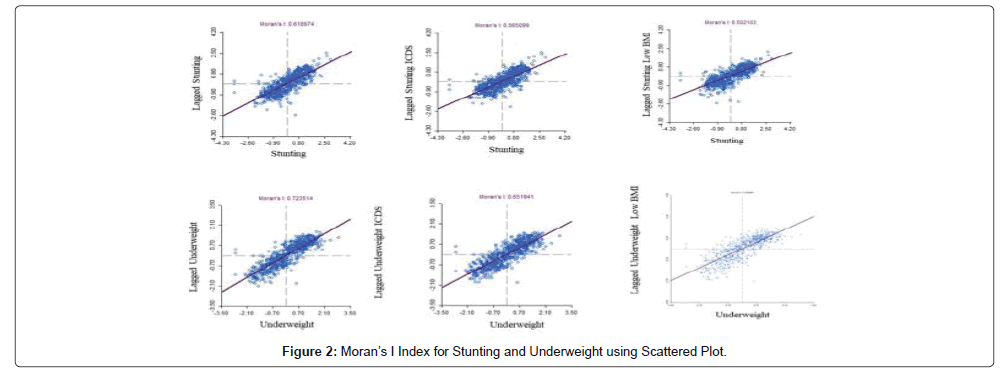
Results: Results highlight that women’s education, maternal nutrition, birth order, birth weight, and the wealth quintiles of households were essential markers of the anthropometric failures among the children. The likelihood of anthropometric failures declined considerably during 1998-2005 in comparison to 2005-15, especially among the children from the wealthiest quintiles. Spatial clustering in the prevalence of anthropometric failures portrayed that Moran’s I values were significant for the utilization of ICDS services and mothers having low BMI. The univariate Moran’s I statistics were 0.62 and 0.72 for stunting and underweight, respectively. When spatial weights were considered, the autoregression model noticeably became stronger in predicting the prevalence of stunting and underweight.
Conclusions: Evidence on significant correlates and spatial dependence of anthropometric failure shed the importance of strengthening multisectoral convergence in various nutrition-specific and nutrition-sensitive interventions in combating the anthropometric failures in the context of nature and patterns emerging in various hotspots and cold spots.
Keywords: Anthropometric failures; Nutrition; Stunting; Underweight; Wasting; Moran’s I; Spatial autocorrelation; Autoregression
Keywords
Anthropometric failures; Nutrition; Stunting; Underweight; Wasting; Moran’s I; Spatial autocorrelation; Autoregression
Background
Three conventional indicators of anthropometric failure among children, namely stunting (low height for age), wasting (low weight for height) and underweight (low weight for age), portray major nutritional challenges not only in the underdeveloped countries but are a telling concern even for developing countries like India [1]. It is also worth mentioning that the development of any country is judged by their economic prosperity as well as by the health and wellbeing of their people, and its ultimate strength is determined by the education and health of its children. Out of all the undernourished children in the world, around 40% live in India [2]. As per the first comprehensive estimate of disease burden due to child malnutrition, two-thirds of 1.04 million under-five deaths in India are primarily due to anthropometric failures [3]. The burden of undernourishment is severe for the health and wellbeing of people in all age groups. Still, children under age five are at a higher risk because undernourishment hampers cognitive development affecting their entire life [4]. Anthropometric failure has both short term and long term unpropitious ramifications associated with it. In the short-term, it leads to ill health and mortality among children [5]. In the long-term, it leads to impaired cognitive development, poorer educational achievement, and impeded economic productivity [6,7].
Additionally, it also accelerates the risk of illnesses and works as the underlying cause of related deaths of a childhood disease such as measles, diarrhea, and acute respiratory infectious diseases [8]. This speaks volumes of the sorry state of the nutritional status of the supposed future of the nation, the building blocks of our nation, our children [9,10]. Given the severity of the problem, eradication of malnourishment was included in the Millennium Development Goals (MDG). Besides, the primary reason this was later included in the Sustainable Development Goals (SDGs), too, was because the target could not be achieved by 2015. Keeping in mind the severity of the challenge, at least 12 of the 17 SDGs are linked to nutrition. Although it seems impossible to achieve it in the short-run, however, with sufficient and continuous efforts, the government plans to achieve SDG-2, which aims to eradicate hunger and all forms of malnutrition by 2030.
The government of India has initiated several large-scale supplementary feeding programs and has been working extensively in the last 65 years to reduce the anthropometric failures in the country [11]. A large number of programs were rolled out to enhance the nutritional status of children, which includes the De-worming program for children, initiation of early breastfeeding under the MAA national breastfeeding program, supplementation of Ironfolic acid tablets (IFA), National Food Security Mission and Poshan Abhiyan for holistic nourishment. Among all these programs, one of the earliest interventions to break the vicious cycle of undernutrition by adopting a lifecycle approach and by reaching the critical age groups is the Integrated Child Development Services (ICDS) Scheme, India’s flagship program for nutrition. It was started in 1975 by the Government of India to achieve better health and nutrition of children, pregnant women, and lactating mothers. Children below age six years are eligible to get the benefits of ICDS services. Under this scheme, beneficiaries receive services like supplementary nutrition for children, health check-up, growth monitoring of children, and their immunization. Besides, pregnant women and lactating mothers receive intensified counseling on nutritional and health information for mothers and their children.
Emphasizing on the broad consensus that, investments in nutrition-specific and nutrition-sensitive programs to ensure healthy living conditions are required to reduce the anthropometric failures substantially. Priorities were always accorded to nutrition-specific interventions that aim to modify individual-level behaviors such as complementary foods and feeding practices and breastfeeding [12-15]. When the findings of NFHS-3 were announced in 2005-06, and it was found that the prevalence of anthropometric failure among children in India was one of the highest in the world, the issue attracted the focused attention of policymakers and program managers. The results highlighted that nearly half of the children under age five were stunted (48%), and (43%) were underweight. Also, it called attention to the fact that the ICDS program in India covered only 110 out of 160 million children under the age of 6 years. With these two sets of information, it is believed that the ICDS scheme is yet to lead a substantial improvement in the nutritional status of children. Also, it can be argued that it is not always food insecurity that affects the level of anthropometric failure in India. There are many other proximate risk factors behind this scenario viz. socioeconomic conditions and maternal characteristics [16]. In addition to this, studies have pointed out that anthropometric failure varies by geographical location because of its altitude, rainfall, crop production, population density and diseases related to the specific area [17-20]. Socio-economic inequality plays a significant role in affecting the three components of anthropometric failure, i.e., stunting, wasting, and underweight in most developing countries like India. There is a pool of the researchers who stringently bolster that the reduction of poverty and strengthening of health infrastructure will assist in improving child health conditions, especially dealing with such failure. However, the causal relationship between socio-economic inequality and anthropometric failure is not explicit. These points toward the need to understand the importance of other known correlates [21]. The fourth round of National Family Health Survey provides the first opportunity in more than a decade to conduct an up-to-date, complete evaluation of the importance of various factors concerning child anthropometric failures in India. It cannot be denied that the nutritional transition in India depicts a significant decline in the prevalence of these failures among children below age five during the last decade, except for childhood wasting. However, several eminent experts have talked about how the problem of anthropometric failure is still severe, with almost two-fifths of the world’s under-nourished children living in India [22]. In the existing nutritional transition among children in India, some critical research questions that emerge from the evolution seen in anthropometric failures are (1) what are the essential contributors to socio-economic and spatial inequalities in anthropometric failures among children in India? (2) How is the spatial heterogeneity in the prevalence of anthropometric failures among under-five children? The results of the spatial analysis will help recognize the role of diverse risk factors in anthropometric failures. This will have pivotal implications for policymakers, planners, and organizations seeking to meet national and international development targets and help policymakers in planning as per the need of the geographical location.
Data and Methods
Data sets
The basic data used in this analysis have been taken from the last three rounds of National Family Health Survey, NFHS-2 (1998-99), NFHS-3 (2005-06), and NFHS-4 (2015-16). NFHS 3 used multistage stratified sampling and was conducted in all 29 states of India. For the first time, the NFHS-4 included all 36 states, union territories, and 640 districts in India [22]. Survey respondents were selected following a stratified two-stage sampling frame by states and urban and rural areas within each state. The data used to pertain to 89,199 eligible women age 15-49 and their children born in the last three years preceding NFHS 2; 124,385 women and their children under five in NFHS-3 and 699,686 women and their children under age five in NFHS-4. The unit of analysis of the study was district; there were 640 districts in India in 2015-16, with each district having an average of 940 households surveyed. The anthropometric measures used were stunting, wasting, and underweight among children born in the last three years for NFHS-2 and the last five years for NFHS 3 and 4.
Description of variables
The predictor variables used in the study were; sex, age of the child, educational level of the mother, place of residence, wealth quintile, belonging to a particular caste, belonging to a particular religion, Body Mass Index (BMI) of the mother, time of initiation of breastfeeding, cesarean section delivery, birth order of the child, birth weight of the child and ICDS usage. All children younger than five years of age were selected for anthropometric measurements. In some of the analyses, we coded age into several groups: 0–5, 6–11, 12–23, 24–35, 36, and above months. BMI of the mother was calculated as weight in kilograms divided by height in meters squared (kg/m2). Mothers were categorized according to three risk factors, ‘underweight” were classified as having a BMI <18.5 k/m2 “normal” was classified as having BMI 18.5-24.95 k/m2 and “overweight/obese” was classified as those having BMI 25- 29.9 kg/m2 and above. Wealth index was divided into quintiles, and each household was assigned its corresponding category (1 being “Poorest” and 5 “Richest” in wealth). Birth order is the number of children a woman has; we have categorized it as “1-2”,” 3-4”, “5 or more”. Mother’s education level has been classified into four groups, “no education”, “primary”, “secondary,” and “higher education”.
Bivariate analysis was used to analyze trends in anthropometric failures among children in India. Univariate and Bivariate Local Moran’s I, and LISA maps were used to analyze the spatial variation in the prevalence of anthropometric failures. Moran’s I is a correlation coefficient that measures the overall spatial autocorrelation of a data set. It is one way to test for autocorrelation and has a value from -1 to 1. A Moran’s value of -1 is perfect clustering of dissimilar values (this can be called perfect dispersion), a value of 0 is no autocorrelation (perfect randomness.), and a value of +1 indicates perfect clustering of similar values (it’s the opposite of dispersion).
A multivariate logistic regression model was used to analyze the adjusted effects of various predictors of anthropometric failure. The OLS suggested there was spatial autocorrelation in its error term for anthropometric failures, so the suitability of Spatial Error Model (SEM) and Spatial Lag Models (SLM) were examined using diagnostic tests. The fundamental difference between the two models is that the spatial lag model, unlike the spatial error model does not consider the spatial dependence in the error term. Diagnostics tests for spatial relationships were carried out, and the value of the Lagrange Multiplier is found significant in both the models (p < 0.001). Next, we compared the Akaike Information Criterion (AIC) value for both the models to know the best spatial fit. Therefore, a larger value of LM (error) than the LM(lag) and relatively larger value of adjusted R2 explained the better model adequacy and lower values of Akaike info criterion and Schwarz criterion, this further explained better suitability of the model, which led us to apply LM(error) model. A detail description of Spatial Error and Spatial Lag models can be found in various literature [23,24].
Findings
Over the last decade, there has been a decline in the level of anthropometric failures among children, except for wasting. The adjusted effect of various predictors of childhood anthropometric failure indicates that the most significant predictors of stunting and underweight are mother’s education, belonging to scheduled caste households, and the lowest wealth quintile. Table 1 shows the trend in anthropometric failure among children below five years of age in India by some selected background characteristics. NFHS-2 had information about children up to 3 years only. The trend in anthropometric failure has been shown in terms of stunting, wasting, and underweight as the nutritional indicators for children under three years and five years of age. Over the last decade, there has been a substantial decline in the proportion of stunted children (from 48% to 38%) and underweight children (from 43% to 36%) in India. However, the trend in wasting is not similar, and there is an increase in the prevalence of wasted children from NFHS-2 to NFHS-4. The study found that the decline in stunting and underweight between NFHS-3 and NFHS-4 was more significant among female children than among male children. The nutritional status of children below age five in rural areas has improved faster in the last decade; there has been a seven-percentage point decline in stunting and a six-percentage point decline among underweight children, but the level of prevalence is still smaller than in urban areas.
| Background variables | Stunting | Wasting | Underweight | ||||||
|---|---|---|---|---|---|---|---|---|---|
| NFHS2* | NFHS3 | NFHS4 | NFHS2* | NFHS3 | NFHS4 | NFHS2* | NFHS3 | NFHS4 | |
| Sex of child | |||||||||
| Male | 49.6 | 42.1 | 37.6 | 18.9 | 19.9 | 22.4 | 39.6 | 36.3 | 34.2 |
| Female | 48.2 | 40 | 34.4 | 17.8 | 18.9 | 20.9 | 38.2 | 36.3 | 32.2 |
| Age of child | |||||||||
| 0-5 m | 24.8 | 18.2 | 20.3 | 24.3 | 28.2 | 29.6 | 30.1 | 25.8 | 25.8 |
| 6-11 m | 33.4 | 25.1 | 23.7 | 20.5 | 25.4 | 25.9 | 32.3 | 29.2 | 27.9 |
| 12-23 m | 55.8 | 48 | 42.3 | 19.1 | 20.1 | 21.1 | 40.9 | 37.9 | 33.9 |
| 24-35 m | 62.7 | 50.6 | 42.2 | 13.3 | 16 | 19.3 | 45.1 | 40.5 | 36.4 |
| 36 and above | NA | 44.1 | 41.9 | NA | 15.3 | 17.3 | NA | 39. 1 | 37.3 |
| Birth size of baby | |||||||||
| Average and above | 46.6 | 39.2 | 35 | 16.3 | 17.8 | 21.1 | 35.4 | 33.5 | 31.7 |
| Below average | 56 | 49.1 | 44.4 | 24.6 | 26 | 26.6 | 49.9 | 47.6 | 45.1 |
| Mother's education | |||||||||
| No education | 58.4 | 52.1 | 47.1 | 21.8 | 24.1 | 25.5 | 49.3 | 48.4 | 46 |
| Primary education | 50 | 45.3 | 41.1 | 18.1 | 20 | 23.2 | 39.5 | 39.1 | 37.8 |
| Secondary education | 39.3 | 34.2 | 31.6 | 14.9 | 16.2 | 20.2 | 27.9 | 28.4 | 28.7 |
| Higher education | 25.8 | 18.3 | 19.9 | 11.2 | 13.1 | 17.2 | 16.5 | 14.9 | 17 |
| BMI of mother | |||||||||
| Underweight | 54.4 | 49.1 | 43.5 | 23.1 | 26.3 | 29.3 | 49.5 | 48.4 | 46.5 |
| Normal | 47.3 | 39.3 | 35.7 | 16.3 | 17.4 | 20.7 | 34.8 | 32.9 | 32.1 |
| Overweight/Obese | 30.9 | 27 | 24.6 | 9.3 | 9.6 | 14.8 | 14.8 | 18 | 18.6 |
| Initiation of breast feeding | |||||||||
| Within 1 hour | 44 | 42.5 | 35.3 | 16.9 | 20.3 | 21.3 | 33.5 | 38.3 | 33.8 |
| After 1 hour | 50.6 | 38.2 | 35.9 | 18.9 | 17.6 | 21.9 | 41 | 32.1 | 33 |
| Birth order | |||||||||
| 1-2 | 44.6 | 31.2 | 33.6 | 16.9 | 18 | 21.1 | 34.4 | 31.2 | 31.3 |
| 3-4 | 52.4 | 39.7 | 41.2 | 19.1 | 19.8 | 22.3 | 42.6 | 39.7 | 37.9 |
| 5 or more | 58.3 | 35.5 | 47.1 | 22.3 | 23.9 | 23.8 | 49 | 49.1 | 44.6 |
| Place of residence | |||||||||
| Rural | 52.2 | 45.2 | 38.3 | 19.5 | 21.1 | 22.3 | 41.9 | 41 | 35.4 |
| Urban | 40.1 | 34.8 | 29.9 | 15.2 | 16.9 | 19.9 | 31 | 29 | 27.1 |
| Religion | |||||||||
| Hindu | 50.1 | 44 | 39 | 19.3 | 19 | 21.8 | 41.6 | 39 | 36.7 |
| Muslim | 50.5 | 45.9 | 39.6 | 18.4 | 17.5 | 18.3 | 39.8 | 37.8 | 33.4 |
| Christian | 38.7 | 39.5 | 33.3 | 13.3 | 13.8 | 13.2 | 20.7 | 25.9 | 20.5 |
| Other | 40.4 | 36.4 | 27.4 | 10.2 | 13.7 | 16.8 | 22.6 | 26.1 | 22.7 |
| Caste | |||||||||
| Scheduled caste | 56.2 | 50.6 | 43.3 | 20.4 | 19.7 | 21.6 | 46.3 | 44.2 | 39.5 |
| Scheduled tribes | 50.7 | 47.1 | 39.7 | 20.2 | 20.6 | 21.6 | 38.7 | 39.4 | 34.7 |
| Other backward caste | 49.5 | 45.9 | 39.4 | 20.1 | 19 | 20.8 | 42.4 | 40.1 | 36.3 |
| Other | 44.2 | 36.1 | 30.4 | 15.3 | 15.7 | 17.9 | 32.9 | 29.7 | 26.8 |
| Wealth quintiles | |||||||||
| Poorest | 60.2 | 56.1 | 49.2 | 26.8 | 28.3 | 28 | 54.8 | 55.5 | 49.1 |
| Poor | 58.3 | 50.7 | 41.5 | 20.8 | 22.1 | 22.8 | 47.9 | 46.2 | 37.7 |
| Middle | 48.2 | 44.9 | 34.4 | 17 | 19.7 | 19.8 | 37.8 | 38 | 30.1 |
| Richer | 42 | 37.2 | 27.5 | 14.7 | 16.8 | 18.5 | 30.5 | 30.7 | 24.4 |
| Richest | 32.3 | 23.9 | 21.8 | 11.1 | 13.5 | 17.3 | 19.8 | 19.1 | 18.7 |
| Total | 48.9 | 48 | 38.4 | 18.3 | 19.8 | 21 | 38.9 | 42.5 | 35.7 |
Table 1: Prevalence in anthropometric failures among children below the age 5 years in India by some selected background characteristic, 1998-2016.
The children whose size was below average at the time of birth were more likely to be malnourished in terms of each of the indicators of anthropometric failure in NFHS-4. Around 50% of underweight mothers had stunted children in 2004-05, the same after a decade in 2015-16 decreased to 43%. In NFHS-3, approximately 36% of mothers having a birth order of 5 or more had stunted children and this rose to 47% in NFHS -4. The percentage of underweight children in rural India declined from 41% to 35% from NFHS-3 to NFHS-4. There was a 4% decline in underweight children from scheduled caste from 2006- 2016. Children age 12 months and above have a higher prevalence of stunting, as well as underweight, than among children aged less than 11 months. However, the same wasn’t true for wasting. As per NFHS-4, around 22% of male children and 21% of female children were wasted
Tables 2a-c presents the predicted probability of being stunted, underweight, and wasted of children using logistic regression analysis for different categories of wealth, mother’s education, and urban-rural place of residence in India, 1998-2016. It is evident from the findings that for children below age three years belonging to the poorest wealth quintile, the estimated probability of being stunted declined from 0.548 in 1998-99 to 0.514 in 2005-06, a decline of 6%. Over the same period, the estimated probability of the stunting among children below age three from the richest wealth quintile declined by 31%. The corresponding declines in the estimated likelihood of stunting among children below age five were 4% among those from the poorest wealth quintiles as against 8% among the children from the wealthiest wealth quintiles. The recent pattern in the decline of the estimated probability of stunting may be attributed to the on-going programs and services to address micronutrient deficiencies and improving child-feeding practices in the country, even among those coming from the poorest wealth quintile. Further, increased nutritional awareness among mothers coming from wealthier households may be the reason behinds the drastic reduction in the estimated probability of stunting among children of mothers from more affluent households.
| Wealth with time | Stunting | Underweight | Wasting | |||
|---|---|---|---|---|---|---|
| predicted probability | C.I. | predicted probability | C.I. | predicted probability | C.I. | |
| 1998-99* | ||||||
| Poorest | 0.548 | (0.533,0.563) | 0.503 | (0.489,0.518) | 0.26 | (0.248,0.272) |
| Poor | 0.543 | (0.529,0.557) | 0.447 | (0.434,0.460) | 0.203 | (0.192,0.214) |
| Middle | 0.474 | (0.461,0.487) | 0.373 | (0.360,0.386) | 0.169 | (0.159,0.18) |
| Richer | 0.453 | (0.439,0.467) | 0.334 | (0.320,0.347) | 0.152 | (0.141,0.163) |
| Richest | 0.41 | (0.392,0.428) | 0.266 | (0.249,0.283) | 0.123 | (0.109,0.136) |
| 2005-06* | ||||||
| Poorest | 0.514 | (0.497,0.530) | 0.498 | (0.482,0.514) | 0.282 | (0.268,0.295) |
| Poor | 0.475 | (0.460,0.490) | 0.431 | (0.417,0.445) | 0.231 | (0.218,0.243) |
| Middle | 0.426 | (0.413,0.440) | 0.348 | (0.335,0.361) | 0.199 | (0.187,0.21) |
| Richer | 0.369 | (0.356,0.382) | 0.29 | (0.277,0.303) | 0.176 | (0.165,0.187) |
| Richest | 0.281 | (0.265,0.298) | 0.212 | (0.197,0.228) | 0.15 | (0.136,0.164) |
| Change 1998-05* | ||||||
| Poorest | -0.034 | -0.005 | 0.022 | |||
| Poor | -0.068 | -0.016 | 0.028 | |||
| Middle | -0.047 | -0.025 | 0.029 | |||
| Richer | -0.084 | -0.044 | 0.024 | |||
| Richest | -0.128 | -0.054 | 0.027 | |||
| 2005-06 | ||||||
| Poorest | 0.485 | (0.031,0.873) | 0.454 | (0.044,0.863) | 0.243 | (0.233,0.253) |
| Poor | 0.524 | (0.071,0.870) | 0.468 | (0.086,0.841) | 0.2 | (0.19,0.209) |
| Middle | 0.458 | (0.044,0.826) | 0.396 | (0.066,0.791) | 0.179 | (0.171,0.187) |
| Richer | 0.39 | (0.032,0.768) | 0.331 | (0.045,0.760) | 0.161 | (0.153,0.169) |
| Richest | 0.262 | (0.028,0.724) | 0.22 | (0.036,0.697) | 0.137 | (0.127,0.147) |
| 2015-2016 | ||||||
| Poorest | 0.464 | (0.047,0.814) | 0.445 | (0.052,0.850) | 0.247 | (0.243,0.25) |
| Poor | 0.482 | (0.074,0.821) | 0.456 | (0.078,0.827) | 0.21 | (0.206,0.213) |
| Middle | 0.41 | (0.057,0.754) | 0.384 | (0.075,0.781) | 0.193 | (0.19,0.197) |
| Richer | 0.339 | (0.046,0.744) | 0.321 | (0.051,0.767) | 0.182 | (0.178,0.187) |
| Richest | 0.241 | (0.036,0.659) | 0.225 | (0.044,0.673) | 0.17 | (0.164,0.175) |
| Change 2005-16 | ||||||
| Poorest | -0.022 | -0.009 | 0.004 | |||
| Poor | -0.042 | -0.012 | 0.01 | |||
| Middle | -0.048 | -0.012 | 0.014 | |||
| Richer | -0.051 | -0.01 | 0.021 | |||
| Richest | -0.021 | 0.006 | 0.032 | |||
* Based on children below three years
Table 2a: Predicted probability of being stunted, underweight and wasted from logistic regression analysis for different categories of wealth in India, 1998-2016
| Education with time | Stunting | Underweight | Wasting | |||
|---|---|---|---|---|---|---|
| predicted probability | C.I. | predicted probability | C.I. | predicted probability | C.I. | |
| 1998-99* | ||||||
| no | 0.554 | (0.545,0.564) | 0.452 | (0.442,0.461) | 0.195 | (0.187,0.202) |
| primary | 0.498 | (0.483,0.513) | 0.394 | (0.380,0.408) | 0.182 | (0.171,0.194) |
| secondary | 0.424 | (0.411,0.436) | 0.323 | (0.311,0.335) | 0.173 | (0.163,0.183) |
| higher | 0.325 | (0.302,0.347) | 0.253 | (0.232,0.275) | 0.158 | (0.140,0.175) |
| 2005-06* | ||||||
| no | 0.463 | (0.452,0.474) | 0.403 | (0.393,0.414) | 0.226 | (0.217,0.235) |
| primary | 0.424 | (0.407,0.440) | 0.36 | (0.344,0.375) | 0.206 | (0.193,0.22) |
| secondary | 0.373 | (0.363,0.383) | 0.31 | (0.300,0.320) | 0.186 | (0.177,0.195) |
| higher | 0.275 | (0.251,0.299) | 0.242 | (0.219,0.265) | 0.177 | (0.157,0.197) |
| Change 1998-05* | ||||||
| no | -0.091 | -0.048 | 0.031 | |||
| primary | -0.074 | -0.034 | 0.024 | |||
| secondary | -0.05 | -0.012 | 0.013 | |||
| higher | -0.049 | -0.011 | 0.02 | |||
| 2005-06 | ||||||
| no | 0.554 | (0.074,0.896) | 0.495 | (0.079,0.877) | 0.197 | (0.190,0.203) |
| primary | 0.471 | (0.053,0.859) | 0.401 | (0.068,0.806) | 0.182 | (0.173,0.192) |
| secondary | 0.372 | (0.033,0.837) | 0.307 | (0.042,0.771) | 0.168 | (0.162,0.175) |
| higher | 0.194 | (0.022,0.643) | 0.157 | (0.027,0.598) | 0.162 | (0.147,0.178) |
| 2015-2016 | ||||||
| no | 0.504 | (0.113,0.821) | 0.48 | (0.113,0.850) | 0.214 | (0.211,0.218) |
| primary | 0.418 | (0.085,0.749) | 0.396 | (0.098,0.769) | 0.204 | (0.200,0.209) |
| secondary | 0.317 | (0.053,0.750) | 0.298 | (0.060,0.755) | 0.203 | (0.200,0.205) |
| higher | 0.181 | (0.036,0.518) | 0.168 | (0.044,0.550) | 0.196 | (0.190,0.203) |
| Change 2005-16 | ||||||
| no | -0.05 | -0.015 | 0.018 | |||
| primary | -0.053 | -0.006 | 0.022 | |||
| secondary | -0.055 | -0.009 | 0.034 | |||
| higher | -0.013 | 0.011 | 0.034 | |||
*Data only for children up to 3 years.
Table 2b: Predicted probability of being stunted, underweight and wasted from logistic regression analysis for different categories of mother’s education in India, 1998-2016.
| Residence with time | Stunting | Underweight | Wasting | |||
|---|---|---|---|---|---|---|
| predicted probability | C.I. | predicted probability | C.I. | predicted probability | C.I. | |
| 1998-99* | ||||||
| Rural | 0.475 | (0.462,0.487) | 0.398 | (0.386,0.410) | 0.183 | (0.177,0.188) |
| Urban | 0.494 | (0.487,0.502) | 0.386 | (0.379,0.393) | 0.186 | (0.176,0.196) |
| 2005-06* | ||||||
| Rural | 0.426 | (0.415,0.437) | 0.36 | (0.349,0.371) | 0.201 | (0.194,0.207) |
| Urban | 0.396 | (0.388,0.404) | 0.34 | (0.333,0.348) | 0.209 | (0.199,0.218) |
| Change 1998-05* | ||||||
| Rural | -0.049 | -0.038 | 0.018 | |||
| Urban | -0.098 | -0.046 | 0.023 | |||
| 2005-06 | ||||||
| Rural | 0.465 | (0.022,0.896) | 0.408 | (0.027,0.877) | 0.179 | (0.174,0.184) |
| Urban | 0.368 | (0.024,0.859) | 0.3 | (0.032,0.808) | 0.185 | (0.179,0.192) |
| 2015-2016 | ||||||
| Rural | 0.423 | (0.040,0.821) | 0.393 | (0.044,0.850) | 0.204 | (0.202,0.206) |
| Urban | 0.305 | (0.036,0.777) | 0.303 | (0.046,0.790) | 0.213 | (0.209,0.217) |
| Change 2005-16 | ||||||
| Rural | -0.042 | -0.015 | 0.025 | |||
| Urban | -0.063 | 0.003 | 0.028 | |||
*Data only for children up to 3 years.
Table 2c: Predicted probability of being stunted, underweight and wasted from logistic regression analysis for different categories of the place of residence in India, 1998-2016
Similarly, the predicted probabilities of being underweight among the children below age three from the poorest wealth quintile declined slightly (only 1%) from 1998-99 to 2005-06. In contrast, the decline in the estimated probability of underweight during the same period was more pronounced among children below age three from the richest quintile (20%). The reduction in predicted probabilities of children being underweight among the most deprived quintiles during the last decade (during NFHS-3 to 4) among children below age 5 was minuscule, ranging from 2% from among those coming from the poorest wealth quintiles to 3% among those coming from the wealthiest wealth quintiles. Besides, Table 2a portrays children below age three; belonging to the poorest quintile, the estimated probability of being wasted increased from 0.260 in 1998-99 to 0.282 in 2005-06, an increase of over 8%. Over the same period, the likelihood of wasting among children below age three from the richest wealth quintile increased from 0.123 in 1998-99 to 0.150 in 2005-06, an increase of 22%. The corresponding increase in the prevalence of wasting among children below age five among those from the poorest and richest wealth quintiles between 2005 and 2016 was 2% and 23%, respectively. These results portray that variation in the estimated probability of stunting as well as underweight were relatively higher among those coming from the poorest households during 1998-99 to 2005-06 in comparison to the recent period of 2005-06 and 2015-16. However, the changes in the estimated probability of wasting remain by and large the same. This may be primarily due to higher values of anthropometric failures during 1998-98, and hence achieving decline might have been more straightforward. Another reason may be the changed age cohort. The prevalence of anthropometric failures in 1998-99 was computed among those below age three, which has the potential to produce faster improvements due to any vertical interventions in comparison to children in the age cohort of under five years.
Table 2b presents the predicted probabilities of stunted, underweight, and wasted children using logistic regression analysis for different categories of mother’s education in India, 1998-2016. The estimated predicted probability of stunting among children below age three among the mothers with no education declined by 16% point during 1998-99 to 2005-06, while the same among those educated up to higher secondary or above declined by 15% during the same period. The corresponding changes in the predicted probability of stunting among children below age five during 2005-06 and 2015-16 were 9% and 6%, respectively. Thus, there is an enormous change in the estimated probability of stunting among women with no education, which gradually declines with time, and hence making is relatively complex to achieve a rapid decline in the future.
For underweight, the changes in the estimated predicted probability among children below age three of the mothers who were having no education were 10%, and for children of those having a higher level of education was only 4% during 1998-99 to 2005-06. However, the corresponding decline in the underweight of children below age five of illiterate mothers during 2006-16 was only 3%. On the other hand, the estimated probability of underweight among the children of mothers educated up to higher secondary or above has increased from 0.157 to 0.167 (7% point) during 2005-06 to 2015-16. In the case of the third indicator of anthropometric failures, i.e. wasting it is worthwhile to mention that the predicted probability of wasting increased uniformly irrespective of their age cohort or periods of 1999-2006 as well as 2006- 16. However, the magnitude of change varies by educational attainment of mothers of those children. Although, it may be complex to explain it precisely it is interesting to point out that during 1999-2006, increase in the estimated probability of wasting was the highest among under three children of illiterate mothers (16%), while the same changes for the cohort of children below age five during 2005-06 to 2015-16 was the highest among mothers educated up to higher secondary or above (21%). This may be one of the reasons behind the increased predicted probability of underweight among children below age 5 of mothers educated up to higher secondary or above. Another possible reason may be the quality of rearing of the children of educated mothers in India, as they might be working in white-collar jobs. Hence, their children might have been looked after either by maids or by elders of the family.
Table 2c portrays the predicted probability of being stunted, underweight, and wasted among children below age three and five, respectively, along with the changes by place of their residence in India during 1998-99, 2005-06, and 2015-16. The prevalence of anthropometric failure among children in India is significantly higher among rural children, irrespective of their age cohort and the periods included in the analysis. It is evident from the results that the predicted probability of stunting among urban children below age three declines by 20% during 1998-99 to 2005-06, while the corresponding decrease among children under age 3 in rural areas was only 10%. The pattern remains the same even among changes in the predicted probability of stunting among children below age five from 2005-06 to 2015-16, where the corresponding declines are 17% and 9% in urban and rural areas, respectively. Mostly a similar pattern has been observed even among the changes in the predicted probability of underweight across urban and rural areas, respectively. These differences in the anthropometric failures among children under age three, as well as under age five may be due to better economic prosperity as well as improved awareness to mass media, which might have altered the child feeding practices in urban areas, resulting into rapid transformation in anthropometric failures among children.
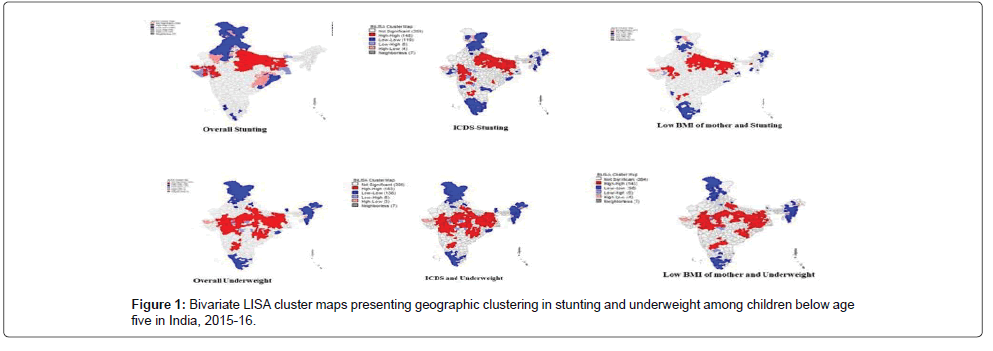
The spatial analysis as shown in Figure 1 indicates that a cluster of 144 districts has the highest level of clustering of stunting and underweight; these districts mostly belong to Uttar Pradesh, Bihar, and Gujarat. In total, 127 districts out of 640 were observed as hotspots for a high prevalence of stunting and low BMI of mothers. Some of these districts are Bijnaur, Bhagpat, Kanpur, Junpur, Agra, Sant ravidas nagar, Buduan, Pilibhit, Rudraprayag.Mainpuri, Etah, Kopal, Bijapur, Davangere, Yadgir, Kaimur, Sitamarhi, VAishali, Darbhanga, Samastipur, Gaya, Narmanda, Bharuch, Kachchh, Anand, Bhopal, Rajnandgaon. The map also shows a high prevalence of the beneficiary of ICDS services and stunted mothers. There are 148 districts, which have been identified as hot spots. These hotspots are mainly in the districts of states like Uttar Pradesh, Bihar, Jharkhand, Gujarat, West Bengal, etc. Some of the hotspot districts are Bahraich, Etawah, Balrampur, Gonda, shrawasti, MAinpuri, Kheri, Farrukhabad, Mirzapur, Kaushambi, Bara banki, Sultanpur, Etah, Fatehpur, Kannauj, Agra, Unnao, Chandauli, Sant Ravidas Nagar, Sitamarhi, Nalanda, Vaishali, Bhabhua, katihar, purnia, madhepura, Muzaffarpur, Lakhisarai,Rohtas, Purba Champaran, Samastipur, Bhagalpur, Khagaria, Parbhani, Nandurbar, Akola, Nashik.
Similarly, the district-level clustering analysis of underweight children identifies 186 districts as hot spots; most of these districts were in poorer states like Odisha, Gujarat, Maharshtra, Chattisgarh, Rajasthan, West Bengal, Uttar Pradesh, Bihar, Jharkhand etc. Around 145 districts show clustering of low maternal BMI and childhood underweight. Some of these districts are Gaya, Lakhisarai, Arwal, Aurangabad, Samastipur, Samastipur, Jabalpur, Sheopur, Guna, Sidhi, Datia, Gwalior, Puruliya, Bankura, Birbhum, Kolkata, Murshidabad. Additionally, the map shows a high prevalence for the beneficiary of ICDS services and underweight mothers, in which total 183 districts were identified as the hot spots. Some of these districts are Narayanpur, Bastar, Uttar bastar kanker, Dakshin bastar kanker, Malkangiri, Nabarangapur, Birbhum, Paschim Medinipu, Bankura, Kolkata, Banka, Gaya, Sheikhpura, Arwal, Madhepura, Lakhisarai, shahjahanpur, Budaun, Lucknow, Lalitpur, Jaunpur.
Figure 2 depicts the bivariate Moran’s I statistics for two measures of anthropometric failures among children across 640 districts of India using the scattered plot. The univariate Moran’s I value for stunting among children is 0.62 (statistically significant), which shows that stunting among children is spatially clustered across Indian districts. Amongst all the factors, the bivariate Moran’s I value for stunting was the highest for utilization of ICDS services by children in the last 12 months (0.57, p<=0.001), followed by low BMI of mothers ( 0.50, p<=0.05). Concerning univariate and bivariate Moran’s I values for underweight, it was found that the univariate Moran’s I was (0.72, p<=0.01) and the spatial autocorrelation was the highest with the utilization of ICDS in the last 12 months (0.65, p <= 0.01) and birth weight (0.60, p<=0).
The spatial autocorrelation with the application of bi-variate LISA maps and Moran’s I put forward the need for analyzing the spatial dependence in the prevalence of stunting and underweight among children aged 0-59 months across different districts of India. To decide the suitability of the model to analyze spatial relationships, two sets of tests on Log Ranges Multipliers (LM) and Robust LM were used with the help of the White test in the OLS model. The White test produces the significance of LM (lag) as well as LM (error). As a result, Robust LM (lag) and Robust LM (error) have been compared. A relatively larger value of LM (error) than the LM (lag) and relatively larger value of adjusted R2, (explaining the better model adequacy) and lower values of Akaike info criterion and Schwarz criterion, (explaining better suitability of the model), guided us to apply LM (error) model to analyze the spatial dependence of stunting and underweight among children with various predictors included in the model. Results of the spatial error model on the spatial relationship of stunting and underweight among under-five children are presented in Table 3.
| Coefficient | Stunting | Underweight | ||||
|---|---|---|---|---|---|---|
| OLS | Spatial Regression (Error Model) | OLS | Spatial Regression (Error Model) | |||
| R-squared | 0.687 | 0.757 | 0.714 | 0.805 | ||
| Log-likelihood | -2035.05 | -1978.57 | -2104.67 | -1997.61 | ||
| Akaike info criterion | 4086.1 | 3973.14 | 4227.35 | 4015.22 | ||
| Schwarz criterion | 4121.83 | 4008.87 | 4267.54 | 4059.88 | ||
| Coefficient | Spatial Error Model (Stunting) | Spatial Error Model (Underweight) | ||||
| Household environment and background characteristics | Coefficient | z-value | Probability | Coefficient | z-value | Probability |
| Lag Coeff. (Rho) | - | - | - | 0.477 | 16.039 | 0 |
| Constant | 6.056 | 3.227 | 0.001 | -14.333 | -4.569 | 0 |
| Rural Place of residence | -0.02 | -1.375 | 0.169 | 0.127 | 3.458 | 0 |
| Belonging to SC/ST caste | -0.0427 | -3.299 | 0 | -0.035 | -3.476 | 0 |
| C-section Delivery | 0.207 | 7.243 | 0 | 0.082 | 3.309 | 0 |
| Higher Birth Order (3+) | 0.352 | 10.529 | 0 | 0.176 | 6.505 | 0 |
| Low BMI of Mother | 0.247 | 7.265 | 0 | 0.419 | 13.251 | 0 |
| Low Birthweight (less than 2.5 kg) | 0.105 | 2.319 | 0.02 | 0.051 | 1.325 | 0.185 |
| No ICDS | -0.0348 | -2.104 | 0.035 | -0.074 | -5.143 | 0 |
| Lambda | 0.582 | 13.957 | 0 | - | - | - |
Table 3: Summary of the output of the spatial error model and maximum likelihood estimation for stunting and Underweight by different background characteristics across districts of India, 2015-16.
The findings portray that in the prevalence of anthropometric failure among children in India, geography matters significantly. When we consider the spatial weights, the spatial regression model becomes more influential in predicting the prevalence of anthropometric failure among children. Poor maternal nutrition, low birth weight, C-section deliveries, and higher birth order were found to be the key predictors significantly explaining the spatial dependence of stunting and underweight among children age 0-59 months. The use of ICDS services in the last 12 months significantly affected the spatial variation in the prevalence of stunting but in a negative direction, which may be primarily due to selection bias for participation in the ICDS. This brings out the issue of selectivity as most of the children who were availing ICDS services either for supplementary nutrition, health check-ups or for immunization services, hail from the socio-economically deprived section of society. Rural place of residence was not significantly affecting the stunting of children, but it has emerged as a considerably affecting predictor of underweight in the spatial model. This find affirms the findings explained in the earlier section that rural children are at a disadvantageous position in terms of anthropometric failures, which varies by space. It is worth mentioning that the inclusion of spatial weights in the model has increased the predicting power of the model from 69% in case of OLS to nearly 76% in the spatial regression model for the prevalence of stunting, while the corresponding values for underweight were 71% and 81% respectively.
Discussion and Conclusions
Anthropometric measures are the most routinely used objective indicators of nutritional status in children [25]. Nevertheless, having the biggest anti-anthropometric failure program and a prolonged history of the fight towards ending it, in 2015-16, more than 38% of children were stunted, 20% were wasted, and 36% were underweight, which is the stark reality. Such high numbers show our failure in securing our children. The relationship between maternal level factors and child’s anthropometric failure has also been documented in several other studies [6,12,16,26]. The study underscores the importance of improving the overall environmental and socioeconomic conditions at the child, maternal and household levels. Children who were more than 12 months of age were more likely to be stunted or underweight; age correlated positively with both, these findings are not surprising and are in line with previous assessments. In the initial months, children are wholly dependent on mother’s milk for food and hence are adequately fed and nourished. However, at a later stage, the child becomes more dependent on other sources of food for his nutrition needs; this could hamper his nourishment levels [27,28].
Our results underscore that factors such as sex of the child, birth order, BMI of the mother, education, and household wealth were highly related to anthropometric failures. Our findings go in line with other authors who talk about maternal education playing a significant role in influencing the anthropometric failure [7,29]. Highly educated have a significant influence on a child’s nutritional status, and this ultimately alters the vicious poverty cycle, as anthropometric failures are critical predictors of human capital. Wasting has a different pattern. Educated mothers had a higher prevalence of wasted children. A possible explanation for this could be the mother’s working status. Mother’s engagement in some occupations adversely affects a child’s growth because they cannot give proper care and time to their children on their own [30].
Further, it is evident from the findings of both rounds of NFHS (2005-06 and 2015-16) that higher birth-order children were under more significant risk of being both stunted and underweight. Frequent pregnancies drain the mother’s health. Many children reflect possibly less care from the mothers to the children [27,29,31]. Our analysis noted significant variation in all the three anthropometric failure measures. A more significant percentage of male children as compared to females were suffering from stunting, underweight, and wasting in 2015-16. Though there is no such discrimination that the male child has to face yet, nature’s phenomenon of male children being more vulnerable right from the womb and later the environmental stress in early life could be leading to this [2,28,32]. Children from the highest wealth quintile were less likely to suffer from such failures. As one climbs up the socio-economic ladder, there is a remarkable drop in the rate of these failures observed. Though no homochromous pattern is there in the prevalence of stunting and underweight in different wealth quintiles, yet, the results of the regression analysis show that children from the highest wealth quintile were in a better predicament than those in the lowest wealth quintile. Similar findings have been well documented in various studies [28-34].
The study findings suggest a clear spatial pattern of stunting, underweight, and wasting across the districts of India. The anthropometric failure (stunting and underweight) showed significant clustering in the districts belonging to the states of Uttar Pradesh, Bihar, Jharkhand, Gujarat, Madhya Pradesh, and Rajasthan. The Moran’s I statistics suggested strong spatial dependence in variation in levels of various anthropometric failures among the states among children aged 0-59 months in India, this highlights that geography plays a substantial role in the levels of stunting and underweight in an area [17-19]. Districts with a higher percentage of underweight women with a BMI of less than 18.5 kg/m2 were significantly more likely to have a higher prevalence of stunting and underweight among their children, and findings were consistent with previous studies. This point towards an intergenerational transfer of poor health from mother to child, studies suggest that a mother’s social and nutritional environment during early life is a significant factor of her children’s subsequent health outcomes [13,20,26].
The districts with a higher incidence of usage of ICDS in the last 12 months are at higher risk of increased prevalence of stunting and underweight. This antagonistic relationship is mainly due to selection bias for the beneficiaries participating in the ICDS program. Strengthening of anganwadis and balwadis will be helpful as they are instrumental in taking care of the child, and educating the child along with providing meals which complement the child’s diet, thus improving their nutritional status. When spatial weights were taken into consideration, the spatial regression model could predict the prevalence of anthropometric failure among children quite substantially. The spatial models suggested a statistically significant association of anthropometric failures (stunting and underweight) with factors such as BMI status of mothers, birth order, caesarean section births, place of residence, BMI of the mother, and ICDS usage. These findings are similar to the results of various studies.
The results of spatial analysis have highlighted that there are variations in the anthropometric failure levels across the country. It is, therefore, vital to plan the combating of the failure in a manner that is suitable for the trends and context of each hotspot and cold spots. The finding that maternal nutrition and maternal education are significant predictors of anthropometric failure among children below age 5 indicate an urgent need to strengthen policy efforts and programs addressing these dimensions of women’s empowerment. Continuous efforts would help reduce disparity in elevating nutrition problems in India and would help in achieving sustainable development goals, particularly those related to the eradication of extreme poverty, hunger, and child survival. Such efforts are the need of the hour given that we have one of the worst anthropometric failure levels worldwide.
Recommendations
These findings demonstrate that multiple factors affect anthropometric failures among children in India. Results on the potential impact of the ICDS indicate that the current efforts of India’s nutrition program, POSHAN Abhiyan, in addressing anthropometric failures can be more productive by enhancing the coverage and efficiency of the ICDS scheme in the country. However, given the multiple social determinants of anthropometric failure, efforts are needed to address those social determinants (wealth, education, etc.) through synergy between the programs and services being implemented by different ministries of Government of India. The government should increase the magnitude of efforts done to combat the anthropometric failure.
Limitations
The study used a number of factors of anthropometric failure among children in India and estimated the contribution of a number of biosocial factors. However, this study did not consider a number of unobserved confounders, including medical factors, which were not investigated as part of the survey.
Author’s Contribution
SKS conceived the idea and designed the experiment. PM reviewed the paper and gave her inputs. SKS and AA analysed the data, interpreted the results, and drafted the manuscript.
The authors reviewed the manuscript and approved the final manuscript for submission for publication.
Conflicts of Interest
The authors do not have any conflict of interest to declare.
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
References
- Nandy S, Miranda JJ (2008) Overlooking undernutrition? Using a composite index of anthropometric failure to assess how underweight misses and misleads the assessment of undernutrition in young children. Social science & medicine 66: 1963-1966.
- Acharya A, Mandal GC, Bose K (2013) Overall burden of under-nutrition measured by a composite index in rural pre-school children in Purba Medinipur, West Bengal, India. Anthropol Rev 76: 109-116.
- Wells JC, Briend A, Boyd EM, Berkely JA, Hall A, et al. (2019) Beyond wasted and stunted- A major shift to fight child undernutrition. Lancet Child Adolesc Health 11: 831-834.
- Progress on sanitation and drinking water: 2014 update. Unicef & World Health Organization (2014).
- World Health Organization (2002)Â The world health report 2002: reducing risks, promoting healthy life. World Health Organization.
- Grantham MGS, Cheung YB, Cueto S, Glewwe P, Richter L, et al. (2007) Developmental potential in the first 5 years for children in developing countries. The lancet 369: 60-70.
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, et al. (2008) Maternal and child undernutrition: consequences for adult health and human capital. The lancet 371: 340-357.
- Abuya BA, Ciera J, Kimani-Murage E (2012) Effect of mother’s education on child’s nutritional status in the slums of Nairobi. BMC pediatrics 12: 80-90.
- Park K (2005) Park's textbook of preventive and social medicine. Preventive Medicine in Obstet, Paediatrics and Geriatrics.
- Meshram II, Arlappa N, Balakrishna N, Rao KM, Laxmaiah A et al. (2012) Trends in the prevalence of undernutrition, nutrient and food intake and predictors of undernutrition among under five year tribal children in India. Asia Pac J Clin Nutr 21: 56-58.
- Demissie S and Worku A (2013) Magnitude and factors associated with malnutrition in children 6-59 months of age in pastoral community of Dollo Ado district, Somali region, Ethiopia. Sci J Public Health 1: 175-83.
- Kishore J (2005)Â National health programs of India: national policies & legislations related to health. Century publications.
- Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, et al. (2008) What works? Interventions for maternal and child undernutrition and survival. The lancet 371: 417-440
- Black RE, Victora CG, Walker SP (2013) Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet 382: 427- 451.
- Ruel MT, Alderman H (2013) Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? The lancet 382: 536-551.
- Menon P, Bamezai A, Subandoro A, Ayoya MA (2015) Ageâ€appropriate infant and young child feeding practices are associated with child nutrition in India: insights from nationally representative data. Matern Child Nutr 11: 73-87.
- Martorell R and Young MF (2012) Patterns of stunting and wasting: potential explanatory factors. Adv Nutr 3: 227-233.
- Miller HJ (2004) Tobler's first law and spatial analysis. Ann Am Assoc Geogr 94: 284-289.
- Pawloski LR, Kevin MC, Constance G David A (2012) Maternal- child overweight/obesity and under nutrition in Kenya: a geographic analysis. Public Health Nutr 15: 2140-2147.
- Spray AL, Eddy B, Hipp JA, Iannotti L (2013) Spatial analysis of undernutrition of children in leogane Commune, Haiti. Food Nutr Bull 34: 444-461.
- Khan J, Mohanty SK (2018) Spatial heterogeneity and correlates of child malnutrition in districts of India. BMC public health 18: 10-27.
- Corsi DJ, MejÃa-Guevara I, Subramanian SV (2016) Risk factors for chronic undernutrition among children in India: Estimating relative importance, population attributable risk and fractions. Soc Sci Med 157: 165-185.
- IIPS & ICF. National Report of 2015-16 National Family Health Survey. 2017
- Darmofal D (2006) Spatial econometrics and political science. In Annual Meeting of Southern Political Science Association, Atlanta, GA.
- Anselin L, Syabri I, Kho Y (2010) GeoDa: An introduction to spatial data analysis. In Handbook of applied spatial analysis (pp. 73-89). Springer, Berlin, Heidelberg.
- Corsi DJ, Subramanyam MA, Subramanian SV (2011) Commentary: Measuring nutritional status of children. Int J Epidemiol 40: 1030-1036
- Subramanian SV, Ackerson LK, Smith GD, John NA (2009) Association of maternal height with child mortality, anthropometric failure, and anemia in India. Jama 301: 1691-1701.
- Pramod Singh GC, Nair M, Grubesic RB, Connell FA (2009) Factors associated with underweight and stunting among children in rural Terai of eastern Nepal. Asia Pac J Public Health 21: 144-152.
- Aguayo VM, Nair R, Badgaiyan N, Krishna V (2016) Determinants of stunting and poor linear growth in children under 2 years of age in India: an inâ€depth analysis of Maharashtra's comprehensive nutrition survey. Matern Child Nutr 12: 121-140.
- Frost MB, Forste R, Haas DW (2005) Maternal education and child nutritional status in Bolivia: finding the links. Soc Sci Med 60: 395-407.
- Mittal A, Singh J, Ahluwalia SK (2007) Effect of maternal factors on nutritional status of 1-5-year-old children in urban slum population. Indian J Community Med 32: 264
- Singh SK, Maharana GB, Srivastava S (2017) Transition in Childhood Malnutrition in India: Evidence from Various Cross-sectional Surveys conducted during 1998 to 2013. Adv Nutr Food Sci 2: 1-13.
- Wamani H, Tylleskar T, Astrom AN, Tumwine JK, Peterson S (2004) Mothers' education but not fathers' education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. Int J Equity Health 3: 9-12.
- Yimer G (2000) Malnutrition among children in Southern Ethiopia: Levels and risk factors. Ethiop J Health Dev 14: 283-292.
Citation: Singh SK, Menon P, Aditi (2020) Tracking Progress in Anthropometric Failure among Children in India: A Geospatial Analysis. Epidemiol Sci 10: 389 DOI: 10.4172/2161-1165.1000389
Copyright: © 2020 Singh SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2849
- [From(publication date): 0-2020 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 2028
- PDF downloads: 821