Perspective Article Open Access
Towards a Standardized Approach for Behavior Change in 21st Century Occupational Health
Jennifer Lunt*Health and Safety Laboratory, Harpur Hill, Buxton, United Kingdom
- *Corresponding Author:
- Jennifer Lunt
Health and Safety Laboratory
Harpur Hill, Buxton, United Kingdom
Tel: +44 (0)1298-218373
Fax: +44 (0)1298-218751
E-mail: jennifer.lunt@hsl.gsi.gov.uk
Received date: May 20, 2013; Accepted date: June 12, 2013; Published date: June 14, 2013
Citation: Lunt J (2013) Towards a Standardized Approach for Behavior Change in 21st Century Occupational Health. Occup Med Health Aff 1:119. doi: 10.4172/2329-6879.1000119
Copyright: © 2013 Lunt J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Not all occupational health risks can be designed out of the workplace. Even with a full complement of protective measures, workers may intentionally or unintentionally behave in such a way that harms their health. This makes understanding the constituents of an effective behavioral change intervention an essential feature of occupational health management. Acquiring this understanding is thwarted in the current occupational health and safety evidence base by (a) an inaccurate assumption health should be managed in the same way as safety; (b) inadequate awareness and coverage of established behavioral determinants, and (c) under reporting of how interventions were designed and implemented. Within public health concerted efforts are underway to standardize behavior change intervention design and reporting at an international level so that a more reliable and informative evidence base can be accrued that permits efficient targeting of resource. This paper makes the case for instigating a similar process in occupational health. Given the diversity of behaviors across different work contexts and hazards, a potential solution for striking a balance between design consistency and relevance is made. This is based on grouping contemporary occupational health conditions according to common behavioral determinants, and targeting approaches at those shared determinants. Developing a more standardized approach to behavior change in occupational health is essential for optimizing prevention of avoidable occupational illnesses, and in preventing sickness absence from other work-relevant conditions over whose incidence the workplace has limited control.
Keywords
Behavioral safety; Occupational health hazards; Behavior change taxonomy; Behavior change wheel
Any credible risk management approach for health and safety should reflect ‘hierarchy of control’ principles [1,2]. In attempting to control risk, eliminating or designing out risk should be addressed before recourse to administrative or personal protective measures. However, not all risks can be designed out. Even with proper controls in place, human fallibility means that workers will still intentionally or unwittingly take a chance with their or their colleague’s health. For example, a paint sprayer may momentarily lift their visor to check the quality of their handiwork, and, in doing so, inhale isocyanatescontaining paint fumes, which may lead to the development of occupational asthma. Despite receiving training on dermatitis risks, a hair dresser may choose not to wear gloves in order to preserve tactile dexterity. Health and Safety Legislation typically imposes a duty of care on employers to, as far as reasonably practicable, ensure the health and safety of their workforce [3-5]. Employees are also required to take reasonable care of their own health and safety of others affected by their “acts or omissions”3. Since an act denotes a behavior, the ability to implement effective behavior change interventions to mitigate risk taking behavior should, therefore, be an essential component of the occupational health professional’s toolbox.
Behavior change interventions have been defined as a “coordinated set of activities designed to change specified behavior patterns” in terms of the behavior’s prevalence and incidence [6,7]. As regards workplace health, not only does understanding how to effectively change behavior apply to mitigating harm to worker’s health, it also applies to workplace health promotion. Positive models of health view wellbeing at work as instilling positive factors over and above the prevention of harm [8]. This might include creating meaningful work, increasing social capital and encouraging uptake of health behaviors [9,10]. Consequently, behavior change is relevant to occupational medicine in two main ways: reducing risk taking and encouraging health promoting behavior.
Current Approaches
‘Behavioral safety’ represents one of the main behavior change approaches currently used within the health and safety domain. Traditionally these comprise a component of either peer or supervisoron worker observation followed by verbal feedback on whether behaviors were safe or require modification [11]. Through recognition that such programs can overlook latent causes of unsafe behavior that may reside within the organization’s culture or management systems, such programs have more recently evolved to include safety leadership and educational elements, for example. An assumption of such programs is that health can be managed in the same way as safety. A growing body of research undertaken by the UK’s Health and Safety Laboratory, including a workshop with industry experts, highlights that this is not the case [12,13] for a number of reasons.
Foremost, relative to safety, occupational health hazards (physical or psychosocial) generally tend to have a longer latency between exposure and harm. Asbestos related disease may arise 40 years after contact with a carcinogenic asbestos fiber [14]. Indeed, health problems may only come about through accumulated exposure, as in occupational asthma [15]. Second, safety hazards tend to be more tangible. A precariously positioned overhead container is easier to spot than toxic gases building up in a grain silo. Third, long latency together with the insidious nature of occupational health hazards can make it harder to attribute cause to the workplace, and to judge whether risk controls are ultimately effective in preventing ill health. Finally, difficulty in isolating cause makes employers’ duty of care responsibilities more ambiguous and harder to enforce for occupational health than safety. The upshot of these differences is that, relative to safety behavior change programs, programs applied to occupational health need to be more innovative in:
• Securing ‘buy-in’ from leadership and workers and in convincing them of the importance of occupational health;
• Educating on the nature of risks and on the effectiveness of controls so that the necessary foresight for anticipating the long range consequences of harm can be created;
• Creating realistic risk perceptions.
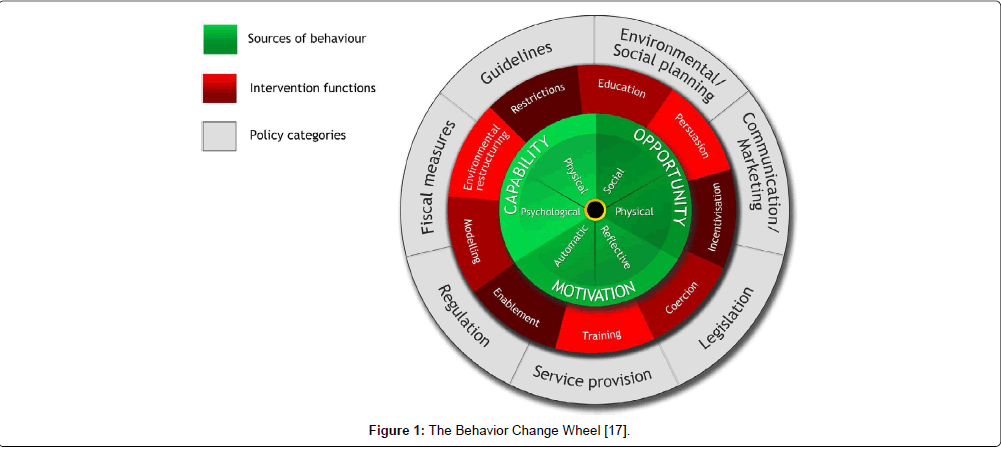
Other common examples of occupational health interventions aimed and either reducing risk taking or promoting positive health behavior tend to be in the form of one-off marketing campaigns or training programmes [13,16]. However, increasing capability through raising awareness and improving skills in this way is only part of the answer for reducing risk taking or encouraging health protective behavior. According to a consensus amongst behavioral theorists, the minimum number of factors required to change behavior involves an interaction between ‘capability’, ‘motivation’ and ‘opportunity’. This is otherwise known as the COM-B model [17]. Capability can be psychological or physical, and encompass knowledge and skills (e.g. job specific, health and safety, intrapersonal, coping). Motivation refers to psychological processes that energize behavior, and can be reflective (e.g. evaluations and plans) or automatic (emotions, impulses, habits, learnt associations at a sub-conscious level). Opportunity corresponds to those factors outside the individual that make a behavior possible, be they physical (e.g. the availability of personal protective measures) or social (e.g. social norms) [17]. It is the interaction between these main behavioral determinants that drives behavior change.
Towards a standardized approach
As we have seen, understanding of what constitutes an effective behavior change intervention as applied to occupational health is thwarted, firstly through an inaccurate assumption that safety and health should be treated in the same way, and secondly, through partial coverage of behavioral determinants. Due to growing recognition that reporting of behavior change interventions has been too poorly specified, and also, that they are too often designed in an ad hoc manner without systematically addressing the ‘active intervention ingredients’ needed to affect change, there exists major initiatives underway in the public health domain to standardize how behavior change interventions are (a) designed, and (b) reported. From this more reliable knowledge accumulation, what does and does not work with respect to behavior change should then emerge. A sounder basis for determining where to invest in public health should then also be more possible. Two initiatives that are potentially key to this drive for greater consistency are the ‘Behavior Change Wheel’ (BCW) and the ‘Behavior Change Taxonomy’ [6,7,17].
Standardizing design
The BCW is a generic evidence-based framework for systematically planning and designing behavior change interventions and policy (Figure 1). With the COM-B model at its heart, planners can use the wheel to create the necessary conditions internal and external to the individual that can achieve behavior change. The different ‘functions’ that interventions would need to serve in order to influence COM-B elements are positioned around the hub. Intervention functions comprise education, persuasion, incentivisation (creating expectation of reward), coercion (creating expectation of punishment), training (skill development) restriction (of options), modeling (provide examples) and enablement (reduce barriers, increase means). Policies that enable the various intervention functions form the outermost layer. In this context, policies refer to activities by the different partners that can help support the intervention. The point behind this wheel is not necessarily to design new interventions to cover all aspects of the framework, but to target design so that the new intervention, together with existing approaches, collectively provide the conditions that drive new behavior.
Standardizing reporting
To enable accurate and faithful implementation of interventions according to how they are planned, an extensive ‘behavior change taxonomy’ [7,8] has been developed for standardizing how the ‘active’ ingredients of an intervention are reported. Ninety three behavior change techniques (BCT’s) have been identified and classified through international multidisciplinary consensus. BCTs are meant to be ‘non-reducible’, ‘non-redundant’ and ‘non-overlapping’ and range from restructuring the social environment, through to reviewing goals and habit formation. Work is now underway to formally link BCTs with each of the interventions functions captured by the behavior change wheel [3].
Clearly, in the public health domain, there is willingness and momentum to drive greater clarity over what constitutes an effective behavior change intervention. Arguably, although improving, the body of research on behavior change interventions undertaken in occupational health settings is considerably smaller than in public health, and has suffered a similar problem in failing to follow a consistent pattern in intervention design and delivery. Equally, it cannot be assumed that what works in public health by default transfers across to occupational health. For example, in public health individual motives may be different. Employees may see it as their employer’s responsibility to protect their health and may therefore adopt a more passive attitude to occupational health risks than lifestyle-related risks. Due to its basis in predominantly health promotion initiatives, the BCT is unlikely to fully capture the complexity of contextual influences that operate in the workplace, such as organizational culture, leadership style and supervisor competency. So, surely the need to standardize the design and reporting of behavior change initiative also applies to occupational health? Making informed decisions about where to target resources is no less important.
The picture is further complicated by the sheer range and complexity of risk taking or health promoting behaviors that can fall under the banner of occupational health. Behaviors will vary according to job type, industry sector, organizational size, or the nature of the hazard to which the individual is exposed. This poses a considerable challenge for developing a standardized approach that retains relevance to a wide range of work contexts and behaviors. One solution may be to find a way of grouping common determinants of either risk taking or health promoting behavior, and then standardizing the approach at the level of that grouping. For example, motivation to change is likely to be a function of the perceived severity of the hazard. Avoiding an obviously life threatening occupational health hazard will be more motivating than avoiding inhaling too much flour dust, for example. Therefore, grouping different occupational health conditions according to similar ‘hazard characteristics’, on the premise that these hazard characteristics interact with the main determinants of behavior (e.g. motivation, capability and opportunity) in a similar ways, could provide a way of striking the balance between consistency and relevance.
Table 1 summarizes one suggested way of grouping contemporary occupational health issues according to different hazard ‘characteristics’. For clarity this table focuses on longer term conditions due to their potential cost implications for employers and upon conditions that arise from exposure to an external hazard rather than an internal disease processes. Accidents are also included to help demark group differences with safety. The differences within the table are relative rather than absolute. Occupational health conditions are split into occupational illnesses that can be more confidently attributed to work specific causes, and work-relevant health conditions that may not be caused by work, but nonetheless are work-relevant because they can impact upon ‘workability’ [18]. Both of these groups can be separated into chronic conditions and conditions that have a life threatening prognosis. The work-relevant group includes common health problems (CHPs) such as anxiety, depression and stress. CHPs differ from the other group by virtue of having psychosocial hazards implicated in their etiology.
While any behavior change intervention aimed at reducing the risks of each of these conditions will have to comprise content that motivates and increases capability and opportunities, it is the relative weighting given to each of these factors that will vary between the groups. Compared to safety, for chronic occupational illnesses, greater emphasis will need to be placed on persuading employees about long term harm. The persuasion process will be even easier for terminal conditions. For work-relevant conditions, education on risk will need to include those encountered outside as well as at work. Equally, since the causes of these conditions are more ambiguous, education, persuasion and enablement will need to foster an attitude in which the responsibility for preventing and managing these conditions is seen as shared between employee and employer. Likewise, since the causes of these work-relevant health conditions cannot realistically be totally prevented by the workplace, then in order to retain a valued skill set, the employer will need to be prepared to develop interventions that enable people with these conditions to remain productive without going off sick. Generally, for all occupational health conditions individuals are more likely to cope successfully with their symptoms where they believe they have control over the demands that are placed on them [19].
The condition classification approach presented in Table 1 is intended to present a potential way forward standardizing behavior change in occupational health. Such approaches should be seen as a supplement to conventional risk management. Developing a more standardized approach is crucial for optimizing prevention of avoidable occupational illness. It is also essential for minimizing sickness absence for those work-relevant conditions that can never be fully prevented by the workplace due to their ubiquitous nature.
| Accidents | Occupational Illnesses | Work-Relevant Health Conditions | Behavior Change Emphasis* | ||||
| Factors distinguishing groups | Chronic | Life threatening | Common Health Problems | Chronic | Terminal/ Degenerative | ||
| Does it: | |||||||
| …have work specific origins? | ✓ | ☑ | ☑ | ₓ | ₓ | ₓ | If not applicable : -Educate on the range of work and non-work risks. -Enable accommodation of unavoidable health limitations |
| ….have physical health hazard as its root cause? | ₓ | ✓ | ✓ | ₓ | ₓ | - | If applicable: -Educate and train on work- based risks and controls |
| …have psychosocial hazards as a root cause? | ₓ | ₓ | ₓ | ✓ | ₓ | ₓ | If applicable: -Train in coping skills for demands and symptoms Restructure the environment to reduce stressors -Enable dual responsibility & workability beliefs |
| …have latent consequences? | ₓ | ✓ | ✓ | ✓ | ✓ | ✓ | Persuade on severity of long term harm. |
| ….have a life threatening consequences? | ✓ | ₓ | ✓ | ₓ | ₓ | ✓ | If applicable: -Persuade on long term -harm and ensure skills for -avoiding harm. |
| …allow a clear cut duty of care? | ✓ | ☑ | ☑ | ₓ | ₓ | ₓ | If not applicable: -Enable dual responsibility & workability beliefs |
| Can it be fully prevented by the workplace? | ✓ | ✓ | ✓ | ₓ | ₓ | ₓ | If not applicable: -Enable accommodation of unavoidable health limitations -Apply behavior change principles to retention at work |
| Examples | Occupational Asthma, Occupational Dermatitis | COPD, Asbestosis | Stress, Anxiety, Depression, MSDs | Work- Relevant Asthma | Cancer | ||
✓ Fully applicable
☑ Less applicable than for safety
x Not applicable
Table 1: Potential classification of occupational health conditions to support a standardized behavior change approach.
Conclusions
Occupational health experts need to work together in a multidisciplinary capacity to establish a workable convention for standardizing behavior change interventions as applied occupational health. A first step may be to achieve consensus on an acceptable way of balancing standardization with relevance, and testing these solutions on a range of conditions. A second step may be to test the behavior change taxonomy on examples of more effective occupational health behavior change interventions to determine how inclusive they are of the approaches used. Without greater consistency in behavior change intervention design and reporting, occupational health may remain on the back foot relative to public health.
References
- HSE (2011) Management of risk when planning work: The right priorities.
- Health & Safety Executive (1997) Successful Health and Safety Management (2ndedn) Sudbury: HSE Books.
- HSE (1974) Health and Safety at Work Act 1974. Accessed 10.06.2013.
- OSH (1989) The European Directive on Safety and Health at Work (Directive 89/391 EEC).
- OSHA (1971) Occupational Safety and Health Act.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, et al. (2013) The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann Behav Med.
- Michie S, Abraham C, Eccles MP, Francis JJ, Hardeman W, et al. (2011) Strengthening evaluation and implementation by specifying components of behaviour change interventions: a study protocol. Implement Sci 6: 10.
- Lunt J, Fox D, Bowen J, Higgins G, Crozier S, et al. (2007). Applying to Biopsychosocial Approach to Managing the Risks of Contemporary Occupational Health Conditions. Scoping Review.
- Steger MF, Dik BJ, Duffy RD (2012). Measuring Meaningful Work: The Work and Meaning Inventory (WAMI). Journal of Career Assessment 20: 322-337.
- Lin N, Cook K, Burt (2002) Social capital: Theory and research,Aldine de Gruyter: New York.
- Hopkins A. (2006). What are we to make of safe behaviour programs? Safety Science 44: 583-597.
- Lunt JA, Sheffield D, Bell N, Bennett V, Morris LA (2011) Review of preventative behavioural interventions for dermal and respiratory hazards. Occup Med (Lond) 61: 311-320.
- Lunt J, O’Hara R, Cummings (2007). “Which Mask Do You Prefer? Changing Occupational Health Behaviour”. Houdmont J, McIntyre S (Eds.). Occupational health psychology: European perspectives on research, practice and education (Vol. 2), Maia, Portugal: ISMAI Publishers.
- O’Regan S, Tyers C, Hill D, Gordon-Dseagu V, Rick J (2007) Taking risks with asbestos. HSE Research Report RR558.
- Fishwick D, Bradshaw L, Davies J, Henson M, Stenton C, et al. (2007) Are we failing workers with symptoms suggestive of occupational asthma? Prim Care Respir J 16: 304-310.
- Robson LS, Stephenson CM, Schulte PA, Amick BC 3rd, Irvin EL, et al. (2012) A systematic review of the effectiveness of occupational health and safety training. Scand J Work Environ Health 38: 193-208.
- Michie S, van Stralen MM, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 6: 42.
- Ilmarinen J (2007) The Work Ability Index (WAI). Occup Med (Lond) 57: 160.
- Hagger MS, Orbell S (2003) A Meta-Analytic Review of the Common-Sense Model of Illness Representations. Psychology and Health 18: 141-184.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 15939
- [From(publication date):
June-2013 - Apr 01, 2025] - Breakdown by view type
- HTML page views : 11323
- PDF downloads : 4616