Review Article Open Access
Towards a Practice Guided Evidence Based Theory of Mentoring in Palliative Care
Loo Teck Wee Wesley1,2, Muhammad Fadhli Bin Mohamad Ikbal1,2, Wu Jingting1,2, Muhammad Taufeeq Wahab1,2, Yeam Cheng Teng2, Ee Hui Fang Margaret2*, Ravindran Kanesvaran1,3,4and Lalit Kumar Radha Krishna1,2,3,51Yong Loo Lin School of Medicine, Singapore
2Department of Palliative Medicine National Cancer Center, Singapore
3Practice Course 2, Duke NUS Postgraduate Medical School, Singapore
4Department of Medical Oncology National Cancer Center, Singapore
5Department of Medical Oncology National Cancer Center, Singapore
- *Corresponding Author:
- Ee Hui Fang Margaret
Elective Student, Department of Palliative Medicine National Cancer Center
Singapore, 11 Hospital Drive, Singapore 169610
Email: margaret.ee8@gmail.com
Received date: November 29, 2016; Accepted date: December 28, 2016; Published date: January 02, 2017
Citation: Wesley LT, Mohamad Ikbal MF, Wu JT, Wahab MT, Cheng Teng Y, et al. (2017) Towards a Practice Guided Evidence Based Theory of Mentoring in Palliative Care. J Palliat Care Med 7:296. doi: 10.4172/2165-7386.1000296
Copyright: © 2017 Wesley LT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Provision of end of life care and coping with the emotional and existential distress engendered by palliative care demands the provision of holistic support and training for palliativists. Mentoring is an effective means of meeting this need; however little is known of mentoring in palliative care and a universally accepted learning theory of mentoring remains lacking in this setting. To advance mentoring practice in palliative care, we review the only two evidenced based mentoring theories based upon narrative reviews of mentoring practice in the key specialties within palliative care teams. Building upon mentoring’s mentee, mentor and organizational dependent, goal specific, context sensitive features highlighted in both recent reviews of mentoring this paper proffers a working theory of mentoring. Constructed Krishna’s Mentoring Pyramid that underlines the 5 core elements of successful mentoring programs, we propose melding elements of the cognitive apprenticeship model with the adult learning theory using the multi-theories model of adult learning offers an effective starting point for a mentoring theory. More context-specific studies are needed to provide better insight into the validity of this framework in the ongoing pursuit of an interprofessional mentoring theory in Palliative Medicine.
Keywords
Mentor; Mentee; Mentoring theory; Palliative medicine; Palliative care; Mentoring
Introduction
Palliative care is characterized by its holistic interprofessional approach to care of patients and their families facing life-threatening illnesses [1]. Provision of end of life care, working in interprofessional set ups and providing holistic support of patients and their families are not often featured in undergraduate and early postgraduate training for nurses, physicians and social workers leaving most clinicians with a superficial understanding of palliative care practice [2]. Training clinicians from different clinical specialties, professional backgrounds and experience in the ethos and practice of palliative care is thus complicated not least, as many require mosaic training which sees training provided by palliativists from different clinical backgrounds [3-11]. Physicians, nurses and social workers for example often receive training from senior palliative care doctors, nurses and social workers [3-11].
Mentoring is increasingly seen as an effective means of providing holistic support for palliative care clinicians [5-11]. Yet no reports of mentoring programs within palliative care exist save for recommendations for the use of mosaic mentoring which would see learners mentored by palliativists from different clinical backgrounds [5-11].
A further obstacle to any proposed employ of mentoring in palliative care is a lack of consistency in the mentoring approaches employed in the key specialties in palliative care teams such as nursing, medicine and social work [10,11]. In part variances in mentoring practice are a result of differences in mentoring goals, clinical practice and healthcare settings and mentee and mentor-dependent factors [10,11]. In turn these differences in mentoring practice obstruct the establishment of clear mentoring goals, compromises understanding and assumption of roles and responsibilities within the mentoring relationships, frustrates efforts to provide consistent, appropriate, timely and individualized support and prevents the forwarding of best practices in mentoring and the employ of mentoring programs within the Palliative Medicine. Meanwhile conflation with practices such as preceptorship, role-modelling, sponsorship, supervision and counselling impede the consistent provision of timely, appropriate and personalised mentoring support, obstructs oversight of the mentoring relationships, inhibits awareness of roles and responsibilities, hinders the realisation of mentoring goals and raises concerns of “exploitative”3 mentoring relationships.
It is therefore argued that if mentoring is to occupy a formal position within palliative care a learning theory of mentoring (henceforth mentoring theory) becomes mandatory to guide and standardize mentoring approaches and ensure a consistent and transparent process.
To our knowledge there are no mentoring theories that account for mentoring in an interprofessional setting much less in clinical palliative care [11]. Forwarding a mentoring theory in interprofessional palliative care to address this gap and streamline mentoring practices, however, necessitates a clinically relevant and robust framework that can account for the varied settings that mentoring takes place within palliative care [10,11]. In addition any mentoring theory within the palliative care setting must also consider its interprofessional and clinical nature.
To forward an evidenced based mentoring theory we draw upon Wu et al. review of mentoring programs entitled “Toward an interprofessional mentoring program in palliative care - a review of undergraduate and postgraduate mentoring in medicine, nursing, surgery and social work” [10] and Wahab et al. review “Creating effective interprofessional mentoring relationships in Palliative Carelessons from medicine, nursing, surgery and social work” [11] that focused upon mentoring relationships in systematic and literature reviews of undergraduate and postgraduate mentoring programs in medicine, surgery, nursing and social work involving senior clinicians and junior clinicians and/or undergraduates. We opted to scrutinize Wu et al. [10] and Wahab et al. [11] reviews given that they represent the latest review of mentoring in healthcare. In addition Wu et al. [10] and Wahab et al. [11] thematic review of systematic reviews of mentoring allows for the circumnavigation of mentoring’s contextsensitive, goal-specific, mentee and mentor-dependent features and circumventing of the influence of different healthcare systems, settings and programs upon mentoring accounts.
It is our belief that the common aspects of mentoring programs and mentoring relationships amongst the key specialties in palliative care highlighted by Wu et al. [10] and Wahab et al. [11] could be used to form the basis for a framework of mentoring theory in interprofessional palliative care [10,11].
Prevailing Data in Clinical Mentoring
In their narrative reviews of systematic reviews of mentoring between 1st January 2000 to 31st December 2015, Wu et al. [10] and Wahab et al. [11] evaluated one review of mentoring in medicine and nursing, 10 mentoring reviews in medicine, 4 mentoring reviews in surgery and 5 mentoring reviews in nursing. Wu et al. [10] focused upon mentoring programs whilst Wahab et al. [11] focused on mentoring relationships. Given the different focus of these studies we will discuss the findings of each paper in turn.
Review of mentoring programs
In their review Wu et al. [10] identified 3 semantic themes constructed from ‘detail rich’ codes surrounding mentoring programs in nursing, medicine and surgery. These themes related to common elements within prevailing definitions of mentoring, components of mentoring approaches and elements of the mentoring process. Wu et al. [10] found that definitions of mentoring in nursing, surgery and medicine described mentoring as a dynamic, context dependent, goal sensitive, mutually beneficial relationship between an experienced clinician and junior clinicians and or undergraduates that is focused upon advancing the development of the mentee.
Wu et al. [10] found that mentoring approaches in nursing, medicine and surgery were individualized and dyadic to ensure privacy. In the palliative care setting where mentees frequently have more than one mentor to address different aspects of their professional, personal, academic and social development Wu et al. [10] advocated that interactions within mosaic mentoring remain individualized and supplemented by e-mentoring or online support that can facilitate timely, holistic, individualized, appropriate and specific mentoring support.
Wu et al. [10] also conclude that mentoring processes in palliative care should be formally supported by a host organization to ensure consistent and effective matching of mentors with mentees, formal mentor training, use of common and established mentoring approaches and to ensure consistency, transparency and accountability of the mentoring process.
Reliance upon mentee dependent factors and the nature and responsibility of mentees and mentors led Wu et al. [10] to conclude that the adult learning theory best encapsulates the mentoring process.
Review of mentoring relationships
Wahab et al. [11] thematically analyzed elements of the mentoring relationship and identified 6 semantic themes built on ‘data rich’ codes of mentoring relationships in medicine, surgery and nursing. These themes included (1) characteristics of prevailing definitions of mentoring, (2) characteristics of mentoring relationships, (3) characteristics of mentors and (4) mentees, (5) benefits of mentoring and (6) drawbacks of mentoring [11]. These themes allowed Wahab et al. [11] to forward a rudimentary structure for the development of mentoring relationship. Echoing Wu et al.’s [10] findings, Wahab et al. [11] found that mentoring to be a dynamic, flexible and evolving process.
Critically, Wahab et al. [11] findings emphasized the pivotal role of apprenticeship with mentoring relationships prompting their adoption of the adapted cognitive apprenticeship model to describe the mentoring process.
Scrutiny of Wu et al. and Wahab et al. positions
The presence of two dissimilar mentoring theories to describe mentoring processes in in medicine, surgery and nursing warrants closer scrutiny. We summarize these findings in [Table 1].
| Review | Summary |
| Wu et al. (2016) “Towards aninterprofessional mentoring program in Palliative Care - a review of undergraduate and postgraduate mentoring in Medicine, Nursing, Surgery and Social Work.” |
Themes of mentoring relationships 1. Components of mentoringapproaches 2. Elements of the mentoring process Recommendation Use of a mosaic-mentoring approachsupplemented with e-mentoring, allhoused within a formal mentoringprogram with organisational support. Underpinned by the adult learningtheory. |
| Wahab et al. (2016) “Creating effective interprofessional relationships in Palliative Care - Lessons from Medicine, Nursing, surgery and Social Work.” |
Themes of mentoring relationships 1. Characteristics of mentoringrelationships 2. Characteristics of mentors 3. Characteristics of mentees 4. Benefits of mentoring 5. Drawbacks of mentoring Recommendation Propose the use of a mosaic-mentoringapproach supplemented with ementoringunderpinned by an adaptedcognitive apprenticeship model |
Table 1: Summary of Wu et al. and Wahab et al. findings. Both studies also studied key components within definitions of mentoring.
Wahab et al. [11] advocate an interprofessional ‘apprenticeship’ model constructed upon an adapted cognitive apprenticeship model that the authors believe “will allow for multiple mentoring relationships that facilitate learning, skills training and personal advice from multiple mentors from different clinical backgrounds”. Wu et al. [10] advocate of a mosaic-mentoring approach supplemented with ementoring set within a formal mentoring program in the belief that this approach “would facilitate holistic, timely, individualized, appropriate and specific support of members of the multidisciplinary team by senior members Palliative Care team from different professional backgrounds”. The presence of two contrasting models hints at the difficulties faced in accounting for the variances in the practice and outcomes of mentoring in these specialties and demand closer scrutiny of the data presented.
Adult learning theory
We begin our analysis of Wu et al. [10] use of Knowles’s [12] adult learning theory or “andragogy” to explain the mentoring processes. Whilst there is little consensus on the exact structure of this evolving concept, the adult learning theory pivots on five critical assumptions [12,13], which when applied to the mentoring context are as follows:
1. Mentees are adults who display self-directed learning [12]. This is evident in the presence of mentee-defined goals of mentoring relationships in mentee initiated mentoring relationship and in their subscription to the overarching goals of a formal mentoring program which mentees enter.
2. Mentees use their experiences to build upon their learning. This makes experiential techniques and case based learning particularly effective [12] especially when mentoring interactions evolve and move from largely theoretical discussions to practical clinical role modelling and research. This is important to Interprofessional Education (IPE) that would underpin mosaic mentoring where “two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes”.
3. Mentees display intrinsic rather than extrinsic motivation [12,13] to learn and motivation is a critical aspect of successful mentoring relationships.
4. Mentees in mentoring relationships in clinical palliative care see learning shift from subject-centred to performance-centred skills and practices [12,13] as they develop their palliative care ‘case based, in-training’ skills.
5. Mentees’ readiness to learn becomes more oriented to the developmental tasks of their social roles [12]. This is evident in the evolving nature of mentoring relationships replete with the development of new roles in clinical practice and stronger participation within the mentoring relationship. Development of such roles are nurtured and guided by mentors.
Wu et al. [10] suggest that mentoring is an individualized context dependent process that sees learning being dependent upon the mentee’s individual experiences and self-directed and reflective learning processes [14-21]. Reflective practice however is commonly not considered in adult learning theories. Meanwhile the presence of mentor-dependent features to help maintain motivation and invigorate learning challenges the notion that mentees are always intrinsically motivated [13,21,22].
Wu et al. [10] suggestion that mentees develop and learn from their experiences points to Experiential learning theories [23] whilst having perspectives shaped in a safe mentoring environment is challenged and supported by the mentor suggests the need to consider Perspective transformation theory [24]. These inconsistencies see Wu et al. [10] adopt Taylor and Hamdy’s [15] multi-theories model that brings together several adult learning theories [25,26] and better captures and explains their findings.
This warrants closer study of the Taylor and Hamdy’s [15] multitheories model. The multi-theories model has five stages. Differing responsibilities conferred upon the mentee and the mentor at each stage reflects the evolving nature of mentoring relationships. In the dissonance phase, gaps are identified in the mentee’s knowledge. The mentor’s role in this phase involves assessing the mentee’s motivation, learning styles and stage of development in order to formulate a mentoring plan and provide the mentee with the necessary resources they would require to develop
In the refinement phase, formation of new concepts is brought about by the addition of new data and experiences to existing knowledge and understanding. This occurs as mentees brainstorm for possible solutions to different problems, actively participate and complete of tasks, and finally, refine these experiences and data into concepts.
The organization phase is marked by mentees restructuring their existing knowledge pool through the process of validating hypotheses of the new knowledge. The feedback and consolidation phase allows the mentee to reflect and validate any new information, acknowledging the increase in their knowledge base as well as the learning process.
The flexibility of this model [15] enables its application to a wide range of mentor-mentee relationships [27] and settings [28]. The model also dichotomizes superficial and deep learning [29,30], suggesting a role for each learning style at different stages of learning. Finally, the model also acknowledges that learning is context dependent, highlighting the situated cognition model [31], which argues that learning is a social activity and its context determines the learning outcome. This model also acknowledges that external factors such as the learning environment may modify the mentees motivation [32].
The cognitive apprenticeship model
Wahab et al. [11] analysis of mentoring relationships sees them propose the adoption of the cognitive apprenticeship model to explicate their findings. Wahab et al. [11] analysis sees junior clinicians build upon their personal and professional experiences through apprenticeship with senior clinicians within the interprofessional team.
Learning occurs through a process known as legitimate peripheral participation – the mentee enters a legitimate profession on the periphery, and develops a new identity [33]. Progress is made through greater participation, learning and practice [33]. This is reflected in modern clinical training: medical students start by observing their mentors, gradually adapting, assimilating and performing various roles and tasks [34]. This process of learning is driven by practical and clinical considerations, focusing upon developing a well-prepared and professional clinician through the acquisition and role modeling of ‘tacit knowledge’, identifiable attitudes and demonstrable knowledge and skills [35] rather than “learning about practice” [36].
Cognitive apprenticeship is adapted from the traditional model of apprenticeship focuses upon assimilation and application of cognitive skills [36]. There are 6 elements to cognitive apprenticeship [34,36] including
1. Role Modeling, which relates to the demonstration of skill by the mentors.
2. Coaching that refers to the provision of feedback by mentors after observing their mentees.
3. Scaffolding which is the process of supporting the mentees in their learning.
4. Articulation serves to encourage mentees to discuss their thoughts in response to questions.
5. Reflection encourages deliberation upon their actions and the reasons underpinning their strengths and weaknesses.
6. Exploration allows mentees to frame and pursue their own problems.
Empirical data appears to suggest that the cognitive apprenticeship model does capture some of the learning processes seen in clinical and social interactions between mentors and mentees [36]. Use of mosaicand e-mentoring to facilitate learning, skills training and personal development from multiple mentors within a interprofessional setting facilitates learning of practical skills and physical processes not commonly associated with cognitive apprenticeship model and envisaging mentoring to be a more holistic and evolving learning process [37,38].
Missing however are due consideration of mentoring relationships and the interactions that occur within them, mentor dependent features, the influence of the mentor upon the mentoring process and the mentor’s ability to mentor [34,38-42].
Reviewing the data
Wahab et al. [11] and Wu et al. [10] posits do not fully explain the mentoring process in healthcare. However Wahab et al. [11] and Wu et al. [10] data does show mentoring between an experienced clinician and a junior physician or medical student as a mutually beneficial, evolving, mentee- and mentor dependent, context-specific, goal goalsensitive relationship. The goals of the mentoring process may either be set by the mentee or by the organization hosting the mentoring program. Success of the mentoring process pivots upon mentoring relationships which in turn relies upon the personal characteristics of mentors and mentees, the manner that mentoring relationships form, the strength of the mentoring ties within these relationships, the influence of environmental, social, personal, academic, professional and organizational factors and the influence of the host organization in supporting the mentoring relationship.
Nurturing mentoring relationships within the context of a formal mentoring relationship that sees mentors matched to potential mentees based upon common interests, values and demographic considerations and the presence of multiple mentoring relationships spanning the width of a mentee’s professional, personal, academic, research and social needs requires careful consideration attempts to foster personal ties.
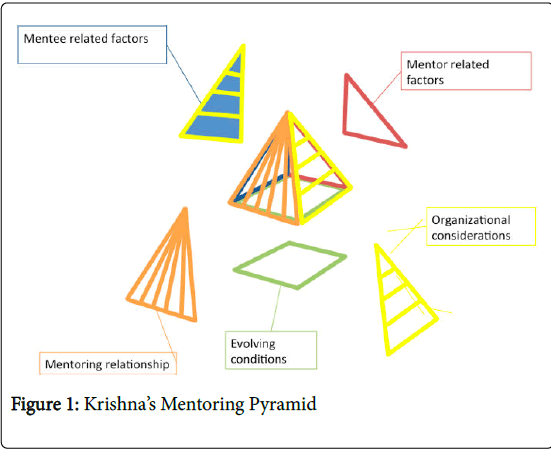
Based on the five dimensions highlighted, Krishna forwards the Mentoring Pyramid (Figure 1) stating that any potential learning theory of mentoring must account for these elements of mentoring practice.
This framework for mentoring in palliative medicine has been developed as a 3-dimensional pyramid built upon four lateral faces with a square base, and is adapted from Miller’s Prism [43]. This framework takes into account a holistic, yet contextualised picture of the evolving nature of mentoring relationship.
The first face of Krishna’s Mentoring Pyramid represents menteerelated factors, and serves to acknowledge the impact and changes in the attitudes, skills and knowledge of mentees as a result of their varied mentoring experiences [12,13,15]. These experiences have an effect on the mentees’ motivations and the contextual factors that impact their participation.
The second face of Krishna’s Mentoring Pyramid considers the key facets of the mentoring relationship. This would include whether the mentoring relationship was informal or formal. The relationship would be determined by the type of research project being mentored, which varies in its duration and frequency of multidimensional appraisal and determines the type and style of support provided. The relationship dimension also includes the degree of mutuality, breadth and depth of the relationship, congruence of mentor and mentee needs and their sensitivity to diversity [10,11,44-46].
The third face of Krishna’s Mentoring Pyramid focuses on mentorrelated factors. These include the mentor’s motivations, their ability to engage mentees and sustain mentees’ interest and motivations, the mentor’s availability and ability to support mentees and how effective the mentor is at detecting, assessing and providing this support [10,11,44-46]. It also necessarily considers the mentor’s character, commitment and ability to meet the multiple roles expected of them. Prior Palliative Medicine training [10,11] that empower the mentor to provide holistic review of the mentees and support mentees within a team-based setting are also considered.
The fourth face of Krishna’s Mentoring Pyramid highlights organizational factors, like the culture of the medical department and the importance given to the program by the major stakeholders in the clinical setting [9]. This aspect of the Mentoring Pyramid considers the support for the mentoring program, whether it is a formal routine established in the curriculum or exists as an informal entity. This affects the resources given to the mentoring relationship, and thus also determines the degree of availability of mentor training and support.
The base of Krishna’s Mentoring Pyramid represents the fluidity of the mentoring process as well as the interactions and impact of each face of the Pyramid on one another. This base represents the maturity of the mentoring relationships, the changes in the mentees’ practice, knowledge and behaviour as a result of their mentoring experiences and interactions with the patients, fellow health care professionals, and senior clinicians including the mentor as mentees progress through different stages of the project [47-50]. This aspect of Krishna’s Mentoring Pyramid underscores the need for a fluid learning theory for mentoring, which makes up the foundation of the mentoring framework for building blocks of the pyramid to be built upon.
Krishna’s Mentoring Pyramid emphasizes the need to consider multidimensional, ethically sensitive, culturally relevant, context specific and organizationally aspects of mentoring when forwrading a mentoring theory [51-52].
Forwarding an evidenced based mentoring theory
A mentoring theory is necessary for advancement of mentoring practice and training of the next generation of hospice and palliative care clinicians, researchers, and leaders. Both Wu et al. [10] proposal of a mentoring theory based upon the principles of adult learning and Wahab et al. [11] advocacy of Cognitive Apprenticeship do encapsulate elements within Krishna’s Mentoring Pyramid and do within their specific confines have their own merits. Broadening considerations to include both aspects of mentoring requires more than simple melding of the two ideas. To effectively consider the various aspects of mentoring we begin by considering Taylor and Hamdy’s [15] evidenced- based Multi-theories Model of adult learning (Multitheories model).
Melding the Multi-theories model
Taylor and Hamdy [15] represent an evidenced based evolution of the traditional adult learning theory. Taylor and Hamdy’s [15] Multitheories model builds upon the six assumptions underpinning the adult learning theory [12,13] which are that mentees are motivated to learn and see the relevance and importance of what they are learning, mentees accept that they are responsible for their own learning and are prepared to learn and mentees tend to build upon their experiences and knowledge. Inspired by a practical appreciation and integration of Kolb’s experiential learning model [22], the three phases of transformative learning, the scaffolding theory that also considers the impact of tutors and mentors and communities of learning, the manner learning occurs according to Krishna’s Mentoring Pyramid and different learning styles allows Taylor and Hamdy [15] to posit 5 phases to learning.
Dissonance relates to challenges to the learner’s knowledge as a result of external challenges from teachers or internal challenges as learners reflect upon gaps in their knowledge. This phase considers the learner’s learning style, stage of development and motivation as well as nature of the task and the available resources. The refinement phase sees the learner reflecting, researching and discussing the problem and integrates ‘new information into…concepts [15]. The organization phase sees learners creating structures for their new information and testing hypotheses based on these structures. Feedback sees these scaffolds and hypotheses tested with peers. The consolidation phase sees reflection upon the process. Critically, Taylor and Hamdy [15] delineate the roles of learners and teachers in each of the five stages.
Applying Wu et al. [10] and Wahab et al. [11] data to the Multitheories model reaffirms the importance of the mentee’s motivation to address recognized gaps in their knowledge within the dissonance phase. The dissonance phase also highlights the importance of a matching process that must consider the needs of the mentees [53] and the pre-mentoring meetings that serve to assess the best means to support the mentee within their particular social, academic, professional and personal environment and their learning styles, their backgrounds, ability and motivations.
The refinement, organization, feedback and consolidation phases highlight the importance of the mentoring relationship and the mentoring environment in providing mentees with the resources required to work through the gaps in their knowledge and provide them with a safe environment to explore their knowledge, provide timely appropriate, individualized and relevant feedback and an opportunity to reflect upon their learning [10,11]. These phases emphasize the importance of the cognitive apprenticeship model highlighted by Wahab et al. [11].
The cognitive apprenticeship model emphasizes the social dimension of the mentoring process. This includes the transition of mentees from peripheral positions to more participatory roles as mentees develop [33]. Highlighting this change also serves to acknowledge the evolving nature of the mentoring relationship as relationships mature. In addition, the cognitive apprenticeship model captures some of the key roles of a mentor including role modeling, coaching, providing individualized and holistic support, scaffolding, facilitating reflective practice and nurturing a safe mentoring environment.
Fusing the cognitive apprenticeship model with the Multi-theories model better captures the mentoring process. Whilst largely complementing the refinement phase, addition of the cognitive apprenticeship model does not drastically change the Multi-theories model.
Conclusion
The melded Multi-theories model does appear to encapsulate the key aspects of the mentoring process described by Wu et al. [10] and Wahab et al. [11]. Whilst this framework does offer a good starting point for an effective mentoring theory further studies need to be carried out within the specific context of mentoring involving senior clinicians and junior clinicians and/or undergraduates within the nursing, medicine, surgery and medical social work settings. Further studies should also be carried out to compare the mentoring process in undergraduates and postgraduate settings to further validate the theory particularly given the potential differences in mentoring approaches, goals and duration in addition to obvious differences in mentee characteristics. We believe an effective mentoring theory is now in sight and hope that standardized mentoring experiences defined by this framework will move palliative care education forward.
References
- http://www.who.int/cancer/palliative/definition/en/
- http://healthaffairs.org/blog/2014/05/28/palliative-care-a-new-direction-for-education-and-training/
- http://bioethics.northwestern.edu/programs/epec/curricula/oncology.html
- http://www.aacn.nche.edu/elnec/about/fact-sheet
- Carey EC, Weissman DE (2010) Understanding and finding mentorship: a review for junior faculty. J Palliat Med 13: 1373-1379.
- Jackson V, Arnold RM (2010) A model of mosaic mentoring. J Palliat Med 13: 1371.
- Arnold RM (2005) Mentoring the next generation: a critical task for palliative medicine. J Palliat Med 8: 696-698.
- Case AA, Orrange SM, Weissman DE (2013) Palliative medicine physician education in the United States: a historical review. J Palliat Med 16: 230-236.
- Periyakoil VS (2007) Declaration of interdependence: the need for mosaic mentoring in palliative care. J Palliat Med 10: 1048-1049.
- Wu JT, Wahab MT, MohamadIkbal MF, Wesley LTW, Kanesvaran R, et al. (2016) Towards an interprofessional mentoring program in Palliative Care – a review of undergraduate and postgraduate mentoring in Medicine, Nursing, Surgery and Social Work. J Palliat Care Med 6:292.
- Wahab MT, MohamadIkbal MF, Wu JT, Wesley LTW, Kanesvaran R, et al.Radha Krishna LK (2016) Creating effective interprofessional relationships in Palliative Care – Lessons from Medicine, Nursing, surgery and Social Work. J Palliat Care Med6: 290
- Knowles MS (1980) The modern practice of adult education: From pedagogy to andragogy (Revised and updated). Cambridge Adult Education, United Kingdom.
- Knowles MS et al. (1984) Andragogy in action: Applying modern principles of adult learning. Jossey-Bass, California.
- Amstutz DD (1999) Adult learning: Moving toward more inclusive theory and practices. New Dir Adult ContinEduc 82:19-32.
- Taylor DC, Hamdy H (2013) Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach 35: e1561-e1572.
- Merriam S (1993) Adult learning: Where have we come from? Where are we headed? New Dir Adult ContinEduc 57:5-14.
- Alhassan AW (2012) Factors affecting adult learning and their persistence: A theoretical approach. EJBSS 1: 150-168.
- Schön D (1987) Educating the reflective practitioner. Jossey-Bass, California.
- Flannery D (1995) Critical multiculturalism: Uncommon voices in a common struggle. Westport, Conn: Bergin & Garvey.
- Kaufman DM (2003) Applying educational theory in practice. BMJ 326: 213-216.
- Abela J (2009) Adult learning theories and medical education: A review. Malta Med J 21: 11-18.
- Morrison R (1998) Teaching and learning in medical practice. Manticore Europe Ltd, United Kingdom.
- Kolb D (1984) Experiential learning. Eaglewood Cliffs, New Jersey.
- Mezirow JE (1990) Fostering critical reflection in adulthood: A guide to transformative and emancipatory learning (1stedn.), Jossey-Bass, California.
- Ingham H, Luft J (1955) The Johari window a graphic model of interpersonal awareness. Western training laboratory in group development.
- Knowles MS (1973) The adult learner: A neglected species. Gulf Publishing, Texas.
- Hawkins A, Jones K, Stanton A (2014) A mentorship programme for final-year students. Clin Teach 11: 345-349.
- Mirghani HM, Ezimokhai M, Shaban S, van Berkel HJ (2014) Superficial and deep learning approaches among medical students in an interdisciplinary integrated curriculum. Educ Health (Abingdon) 27: 10-14.
- Newble DI, Entwistle NJ (1986) Learning styles and approaches: implications for medical education. Med Educ 20: 162-175.
- Newble DI, Clarke RM (1986) The approaches to learning of students in a traditional and in an innovative problem-based medical school. Med Educ 20: 267-273.
- Wilson AP (1993) The promise of situated cognition. An update on adult learning theory. Jossey-Bass, California.
- Sobral DT(2004) What kind of motivation drives medical students' learning quests? Med Educ 38: 950-957.
- Dennen VP (2004) Handbook of research on education communications and technology (2ndedn). Lawrence Erlbaum Associates Publishers, New Jersey.
- Stalmeijer RE, Dolmans DH, Wolfhagen IH, Scherpbier AJ (2009) Cognitive apprenticeship in clinical practice: can it stimulate learning in the opinion of students? Adv Health SciEdu Theory Pract 14:535-546.
- Dornan T, Hadfield J, Brown M, Boshuizen H, Scherpbier A (2005) How can medical students learn in a self-directed way in the clinical environment? Design-based research. Med Educ 39:356-364.
- Collins, A., Brown, J. S., and Newman, S. E. (1988) Cognitive apprenticeship: Teaching the craft of reading, writing and mathematics (Technical Report No). Vol. 8. University of Illinois.
- Lyons K,McLaughlin JE, Khanova J, Roth MT (2016) Cognitive apprenticeship in health sciences education: a qualitative review. Adv Health SciEduc Theory Pract.
- O’Connell HP (2009) Spicing up medical education. Student BMJ 17:b2390.
- Halpern SD, Detsky AS (2014) Graded autonomy in medical education--managing things that go bump in the night. N Engl J Med 370: 1086-1089.
- Straus SE, Chatur F, Taylor M (2009) Issues in the mentor-mentee relationship in academic medicine: a qualitative study. Acad Med 84: 135-139.
- Dillis CR, Romiszowski AJ (1997) Instructional developmental paradigms. Educational Technology Publications, New Jersey.
- Sheehan D, Bagg W, de Beer W, Child S, Hazell W, et al. (2010) The good apprentice in medical education. N Z Med J 123: 89-96.
- Miller GE (1990) The assessment of clinical skills/competence/performance. Acad Med 65: S63-S67.
- Frei E, Stamm M, Buddeberg-Fischer B (2010) Mentoring programs for medical students--a review of the PubMed literature 2000-2008. BMC Med Educ 10: 32.
- Sambunjak D, Straus SE, Marusic A (2010) A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine.Gen Intern Med 25: 72-78.
- Buddeberg-Fischer B, Herta KD (2006) Formal mentoring programmes for medical students and doctors--a review of the Medline literature. Med Teach 28: 248-257.
- Kram KE (1983) Phases of the Mentor Relationship. Acad Manage J 26:608-625.
- White HK, Buhr GT, Pinheiro SO (2009) Mentoring: a key strategy to prepare the next generation of physicians to care for an aging America. J Am GeriatrSoc 57: 1270-1277.
- Chen CM, Lou MF (2014) The effectiveness and application of mentorship programmes for recently registered nurses: a systematic review. J NursManag 22: 433-442.
- Haggerty LA, Grace P (2008) Clinical wisdom: the essential foundation of "good" nursing care.J Prof Nurs 24: 235-240.
- Holmes DR Jr, Hodgson PK, Simari RD, Nishimura RA (2010) Mentoring: making the transition from mentee to mentor. Circulation 121: 336-340.
- Myhre DL, Sherlock K, Williamson T, Pedersen JS (2014) Effect of the discipline of formal faculty advisors on medical student experience and career interest. Can Fam Physician 60:e607-e612.
- Dorsey LE, Baker CM (2004) Mentoring undergraduate nursing students: assessing the state of the science. Nurse Educ 29:260-265.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 4575
- [From(publication date):
January-2017 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 3671
- PDF downloads : 904