Case Report Open Access
Tourette Syndrome: A Case Report, When Exclusion of Differential Diagnoses and Comorbidities Really Matters
Eman A Zaky* and Rana AA MahmoudChild Psychiatry Unit, Department of Pediatrics, Faculty of Medicine, Ain Shams University, Egypt
- *Corresponding Author:
- Eman Ahmed Zaky
Professor of Pediatrics and Head of Child Psychiatry Unit
Department of Pediatrics, Faculty of Medicine
Ain Shams University, Cairo, Egypt
Tel: + 201062978734
E-mail: emanzaky@med.asu.edu.eg
Received date: July 21, 2017; Accepted date: July 28, 2017; Published date: August 07, 2017
Citation: Zaky EA, Mahmoud RAA (2017) Tourette Syndrome: A Case Report, When Exclusion of Differential Diagnoses and Comorbidities Really Matters. J Child Adolesc Behav 5: 352. doi:10.4172/2375-4494.1000352
Copyright: © 2017 Zaky EA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Tourette syndrome (TS) is a childhood-onset neuropsychiatric disorder that is characterized by the presence of multiple motor tics and at least one phonic tic for a minimum of one year duration. It has many differential diagnoses and is often associated with psychiatric comorbidities. One of the differential diagnoses of TS is Autism Spectrum Disorder (ASD); the stereotypic behavior of which needs to be differentiated from the tics of Tourette sufferers. This is a report of an 8-year-old boy with Tourette syndrome who was seriously disabled by his symptoms that necessitated thorough evaluation to exclude any causes, differential diagnoses, and or comorbidities. The treatment of children and adolescents with Tourette syndrome is an important clinical issue. In such cases the potential longterm negative effects of using antipsychotic or other medications need to be weighed against the disruptive effects of persistent Tourette symptoms on patients’ lives.
Keywords
Tourette syndrome (TS); Tics; Autism Spectrum Disorder (ASD); Attention Deficit Hyperactivity Disorder (ADHD); Obsessive Compulsive Disorder (OCD); Cognitive Behavior Therapy (CBT)
Introduction
Tourette syndrome is primarily a pediatric disorder. Children are most commonly affected and the prevalence is 3-4 fold higher in boys (4-5 per 10,000) than in girls; with the highest incidence between 5 and 7 years of age. This developmental disorder is characterized by the presence of multiple motor tics and at least one phonic tic for a minimum period of 1 year, beginning before 18 years of age and occurring in bouts [1].
Tourette syndrome is distinguished by erratic movements of the whole body accompanied by sporadic instances of aimless spitting and shouting which is unpleasant to those around the patient. Tourette syndrome is a chronic disorder that follows a waxing and waning course causing distress for both the patient and the patient's family with symptoms reaching their peak severity between 10 and 12 years of age, and decline drastically or even vanish completely by the end of adolescence [2].
This is a report of an 8-year-old male child with Tourette syndrome that his tics needed to be differentiated from the stereotypic behavior and associated structural language disorder of highly functioning autistics. On the other hand, the reported patient was misdiagnosed as a case of chest infection and accompanying malingering behavior for several weeks prior to settling the diagnosis of Tourette syndrome.
Case Report
An 8-year-old male presented to the Child Psychiatry Clinic, Children’s Hospital, Ain Shams University, Egypt with many motor and vocal tics. He was reluctant to go to school because he does not get along with his classmates; he almost has no friends; and his violent behavior and irritability frequently interfered with his home life and school performance. The condition started about 15 months before presentation to our Clinic with throat-clearing sounds, grunting, and coughing. The mother sought medical advice and he was misdiagnosed as a case of upper respiratory tract infection for which he was given medications with no improvement. One month later, he started to experience repetitive involuntary shoulder shrugging, grimacing, erratic limb movements, and neck twisting to the right side. The intensity and persistence of the symptoms waxed and waned spontaneously but he has never been completely symptom-free since his condition started. Symptoms tended to be less severe when engaged in physical activity but they would exacerbate when he was fatigued, stressed, or frightened. Over the past month, his motor tics showed gradual spontaneous improvement.
His mother reported that prior to the development of tics; he showed hyperactivity and aggressive behavior towards his family members and his teachers and peers at school. The mother also reported delayed speech for which he did not receive any management and spontaneously improved after the age of three. This was followed by stuttering at the age of 5 years which was intermittent and aggravated by emotional disturbances. In addition, he shows bouts of coprolalia and echolalia.
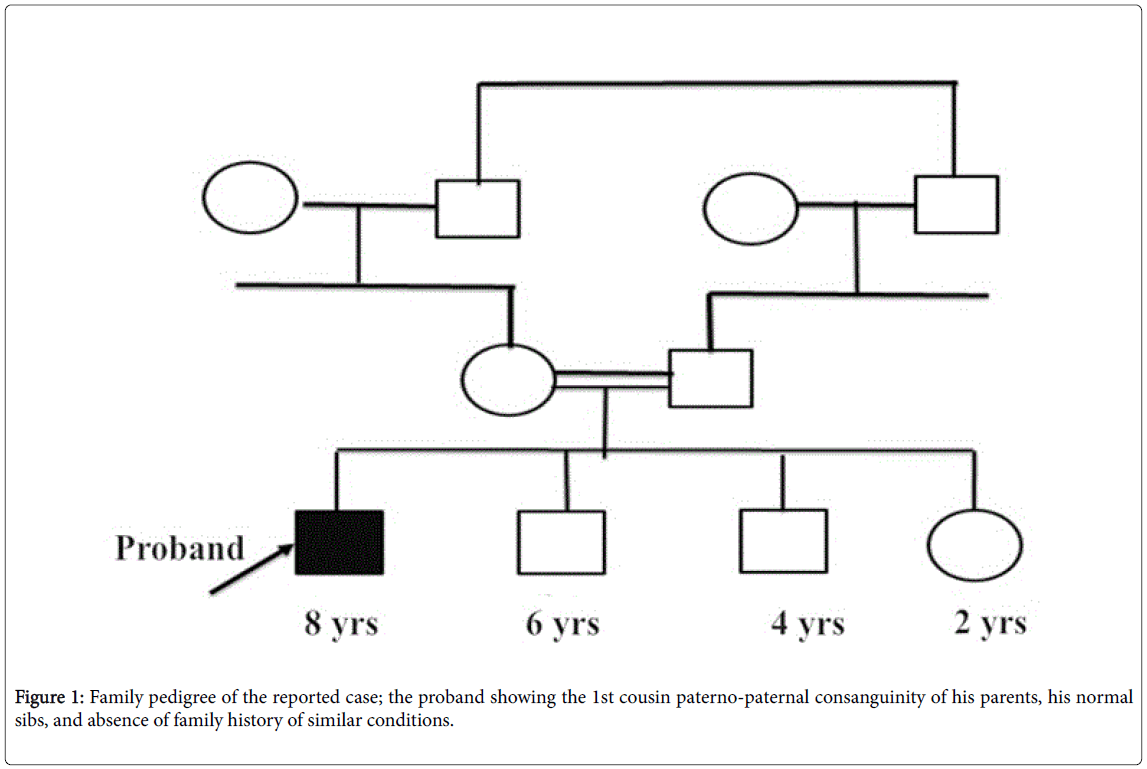
Upon reviewing his perinatal and developmental histories; he was the first born to a first cousin consanguineous parents (paternopaternal); Figure 1, he was a full term baby with a normal vaginal delivery with no antenatal or postnatal complications, achieved the normal developmental milestones apart from delayed speech at the expected average time. He was fully immunized to schedule with no past history of recurrent throat or other significant infections.
He was an average student at school with no learning disabilities but his aggressive behavior with his teachers and classmates interfered with his academic performance. There was no history of obsessiveness, compulsiveness, secondhand smoke exposure, or substance abuse.
He had 2 brothers and a sister who were completely normal and there were no similar conditions in the family and no family history of other mental disorders; Figure 1.
On examination; the patient had fair general condition, temperature was 37ºC, heart rate was 110/min while RR was 20/min. His weight, height, and head circumference were on the 25th percentile for age, and there was no pallor, cyanosis, jaundice, edema, skin rashes, or lymphadenopathy. As for neurological examination; the right handed boy was fully conscious, alert, oriented to person, time, and place with intact thought processes and higher mental functioning. He showed vocal tics in the form of grunting, throat clearing, and production of abnormal sounds with bouts of coprolalia and echolalia. His motor tics at the time of examination were in the form of asymmetric shoulder shrugging, grimacing, erratic limb movements, and twisting his neck to the right side. Because of the delayed speech and the early onset of structural language disorder that was encountered in the reported case, it was crucial to differentiate his motor tics from the stereotypic behavior of highly functioning autistics. The latter starts earlier in life and unlike our case, is bilateral, symmetrical, and rhythmic affecting mainly the extremities although it can involve the trunk as well.
His local neurological examination showed normal tone, power, and reflexes. The cranial nerves examination revealed no abnormality. There were no wasting or deformities. Physical examination revealed no other abnormalities. Chest and heart examination revealed nothing significant with normal heart sounds, bilateral equal intensity of breath sounds, and no adventitious sounds or murmurs. Abdomen was clinically free.
Laboratory investigations showed a normal ESR, CRP, ASOT, CBC, normal renal functions, serum electrolytes, albumin, and normal urine analysis. The liver functions were normal including ALT, AST, and total and direct bilirubin. Thyroid profile was normal excluding hypothyroidism as a cause of tics. Serum copper and ceruloplasmin were normal excluding Wilson’s disease. Toxicological screen was done and excluded cocaine or stimulant toxicity. Imaging studies were carried out including MRI brain that was normal. EEG showed no epileptogenic discharge. DSM 5 diagnostic criteria excluded ASD, ADHD, and OCD.
Discussion
Tourette's is no longer considered a rare condition, but it is not always correctly identified because most cases are mild and the severity of tics decreases for most children as they pass through adolescence. Between 0.4% and 3.8% of children and adolescents ages 5 to 18 may have Tourette's with more boys affected than girls; the prevalence of other tic disorders in school-age children is higher, with the more common tics of eye blinking, coughing, throat clearing, sniffing, and facial movements. Extreme Tourette's in adulthood is a rarity, and Tourette's does not adversely affect intelligence or life expectancy [3].
Tourette syndrome (TS) is characterized by sudden, involuntary, repetitive, non-rhythmic movements (i.e., tics) such as blinking, grimacing, head jerking, or shoulder shrugs. Complex motor tics consist of several simple motor acts occurring in a coordinated sequence or semi-purposeful movements, such as touching or tapping. Simple phonic tics consist of simple, unarticulated sounds such as throat clearing, sniffing, grunting, and coughing. Tic episodes occur in bouts, which can be exacerbated by stress, fatigue, extremes of temperature, and external stimuli. Intentional movements attenuate tic occurrence over the affected area and concentration in non-stressful physical or mental activities tends to diminish tic symptoms [4].
Genetic and environmental factors including autoimmunity play a role in the etiology of Tourette's, but the exact causes are unknown. Comorbid conditions (co-occurring diagnoses other than Tourette's) such as attention deficit hyperactivity disorder (ADHD) and obsessive–compulsive disorder (OCD) are present in many patients. These other conditions often lead to more functional impairment to the individual than the tics that are the hallmark of Tourette's; hence, it is important to correctly identify comorbid conditions and treat them properly [5]. On the other hand, differential diagnoses are many and need to be excluded for implementation of the proper management plan for each patient [6].
The diagnosis of TS is a clinical diagnosis made by an expert observation verifying that the suspected case had both physical and vocal tics for a duration not less than one year. The association with other mental disorders is always a possibility that must be ruled out in each case. Carrying on some investigations will help to exclude such an association and to assess the patient’s general condition before using any medications whenever necessary. For non-experts, misdiagnosis may occur as some parents and inexperienced physicians may consider eye blinking as a reflection of an error of refraction, sneezing as a manifestation of seasonal allergy, or coughing as an asthma equivalent or respiratory tract infection [7].
The patient described in this report is an 8 year old male with a history of multiple motor and vocal tics that waxed and waned over 15 months. This pattern of symptoms clearly meets the diagnostic criteria for TS [1], a condition that is more prevalent in males and usually affects the face (with blinking and grimacing) more than other parts of the body. Our case was misdiagnosed as a case of chest infection and accompanying malingering behavior for several weeks prior to settling the diagnosis of Tourette syndrome at our Clinic and his tics needed to be differentiated from stereotypic behavior of ASD.
Other reports suggest that ADHD and OCD is more common in individuals with a history of TS [1,8]. The reported patient did not manifest DSM 5 diagnostic criteria for obsessive compulsive or attention deficit hyperactivity disorders but it is crucial to continue monitoring him for the emergence of such symptoms in the future.
The definitive etiology of TS is unknown but there is a universal agreement about the strong genetic vulnerability for the disorder with some environmental factors that may play a role in the expression of its severity [9]. The reported case was the first born to a first cousin consanguineous parents (paterno-paternal), nevertheless there were no similar cases in his family or an exposure to a predisposing environmental factor before the development of TS symptomatology.
The decision to begin therapy should be based on the extent to which tics or other symptoms are interfering with the child’s normal development and education or the adult’s ability to function in a productive fashion. Just because a symptom exists, tics or otherwise, is not an adequate reason to initiate behavioral or pharmacotherapy. The patient and family should understand that there is no cure for tics and all treatment is strictly symptomatic. In most cases, medication is unnecessary. There is no effective treatment for every case of tics, but certain medications and therapies can help when their use is warranted. Education is an important part of any treatment plan, and explanation and reassurance alone are often sufficient treatment [6,10]. For the reported case, education about the disease, reassurance, and behavior therapy in the form of awareness training and competing response have been started.
Conclusion
Individuals with a tic disorder should have careful assessment of tics, differential diagnoses, and comorbid conditions with determination of problem severity and functional impairment as well as evaluation of their general health, family history, and prior therapies. Input from the patient, family, and school personnel is required to determine whether tics or associated problems (e.g., ADHD, OCD, school problems, or behavioral disorders) represent a significant handicap that necessitates intervention or not as the potential long-term negative effects of using antipsychotic or other medications need to be weighed against the disruptive effects of persistent Tourette symptoms on patients’ lives.
References
- DSM 5 (2013) Tourette disorder in Diagnostic and Statistical Manual of Mental Disorders, 5th edition. American Psychiatric Association. Arlington.
- Sadock BJ, Sadock VA (2003) Synopsis of Psychiatry. 9th ed. Philadelphia: Lippincott Williams & Wilkins.
- Bhatia MS, Gautam P, Kaur J (2014) Case report on Tourette syndrome treated successfully with aripiprazole. Shanghai Arch Psychiatry 26: 297-300.
- Shim SH, Kwon YJ (2014) Adolescent with Tourette syndrome and bipolar disorder: A case report. Clin Psychopharmacol Neurosci 12: 235.
- Singer HS (2011) Tourette syndrome and other tic disorders. Handb Clin Neurol 100: 641-657.
- Zaky EA (2017) Tourette syndrome; is it an annoying disorder or an inspiring companion??!!! J Child Adolesc Behav 5: e119.
- http://www.ninds.nih.gov/disorders/tourette/detail_tourette.htm
- Leckman JF, Bloch MH, Scahill L, King RA (2006) Tourette syndrome: the self under siege. J Child Neurol 21:642-649.
- O Rourke JA, Scharf JM, Yu D, Pauls DL (2009) The genetics of Tourette syndrome: A review. J Psychosom Res 67: 533-545.
- Roessner V, schoennefeld K, Buse J, Bender S, Ehrlich S, et al. (2013) Pharmacological treatment of tic disorders and Tourette Syndrome. Neuropharmacology 68: 143-149.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 7400
- [From(publication date):
specialissue-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 6443
- PDF downloads : 957