Case Report Open Access
Total Esophagectomy and Endoscopic Radiofrequency Ablation for a Case of Diffuse Esophageal Papillomatosis: Case Report
Angela Romano*, Michele Grassia, Giuseppe Esposito, Marianna Petrillo, Modestino Pezzella, Francesco Maria Romano, Francesco Torelli, Antonio Volpicelli, Franca Ferraraccio, Gerardo Nardone and Natale di MartinoInstitute of Neurology, Catholic University of Sacred Heart, Rome, Italy
- *Corresponding Author:
- Angela Romano
Institute of Neurology, Catholic University of Sacred Heart, Rome, Italy
Tel: 393804354464
E-mail: angelaromano_ar@libero.it
Received date: October 11, 2016; Accepted date: November 07, 2016; Published date: November 14, 2016
Citation: Romano A, Grassia M, Esposito G, Petrillo M, Pezzella M, et al. (2016) Total Esophagectomy and Endoscopic Radiofrequency Ablation for a Case of Diffuse Esophageal Papillomatosis: Case Report. J Gastrointest Dig Syst 6:478. doi:10.4172/2161-069X.1000478
Copyright: © 2016 Romano A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Esophageal squamous papilloma (ESP) is a benign epithelial lesion. ESP is extremely rare and it has been described in few cases in literature. The etiology of ESP may be associated to chronic mucosal irritation and HPV infection. It is usually asymptomatic and mostly discovered as an incidental finding during upper gastrointestinal endoscopy. It is considered a benign neoplasia but recent reports have stressed the potential malignant evolution of these lesions. A 53 year old caucasian woman presented with a four years history of disphagia not responsive to medical therapy. At upper endoscopy, esophageal mucosa appeared hyperemic and completely covered by numerous (>100) sessile peduncolate papules. Biopsies demostrating atypical epithelial proliferation confirmed the diagnosis of esophageal squamal papillomatosis with low grade and focal high grade dysplasia; in situ hybridization studies for HPV were perfomed and it was positive for the type 16. We report a case of diffuse esophageal papillomatosis with histologic and microbiologic findings of genotype 16 HPV and Lichen Planus infection successfully treated with an Ivor Lewis Esophagectomy and a second look endoscopy by radiofrequency ablation.
Keywords
Total esophagectomy; Endoscopic radiofrequency ablation; Diffuse esophageal papillomatosis
Introduction
Although first described [1], squamous papilloma of the esophagus is a rare endoscopic finding, occurring in 0.01% of individals at autopsy and 0.07% of patients during routine endoscopy [2]. Esophageal papillomatosis is a very rare condition and it has a benign clinical course. The natural history of papillomatosis is controversial, with early reports suggesting that it was a benign condition and that endoscopic surveillance was unnecessary [2]. More recently, there have been reports of malignancy in cases of esophageal papillomas. This has led some authors to recommend that esophageal papillomatosis be considered a premalignant condition with the potential for the development of squamous cell carcinoma [3]. Some studies have pointed to the possible presence of malignant tumors in association with esophageal papillomatosis.
Among the viral infections that have proven to play an active role in esophageal carcinogenesis, persistent infection with human papilloma virus (HPV) is thought to have the greatest importance but clear association has not yet been proven. Human papilloma virus (HPV) is an oncogenic, double-stranded, DNA-virus that infects skin and mucosa. Usually associated with benign papillomas, mucosal HPV Infection is one high-risk types, such as HPV 16 and 18 can rarely progress to dysplasia and cancer, a process that takes a long time to occur [4,5].
We describe a case of diffuse esophageal papillomatosis with histologic and microbiologic findings of genotype 16 HPV and Lichen Planus infection successfully treated with an Ivor Lewis Esophagectomy and a second look endoscopy by radiofrequency ablation of the new lesions.
Case report
A 53 year old Caucasian woman was evaluated in Hospital for weight loss and progressive solid food dysphagia not responsive to proton pump inhibitors. Personal Health revealed genital and oral Lichen Planus and for HCV infection. Two years before, the first gastroscopy was negative.
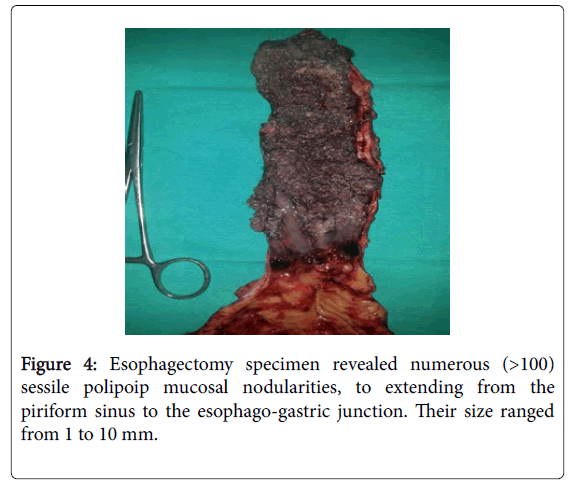
A second endoscopy, performed for solid food impaction, revealed extensive esophageal nodularities and hyperemic, spontaneously bleeding mucosa and it demonstrate multiple flesh coloured pedunculated papules, involving the entire circumference.
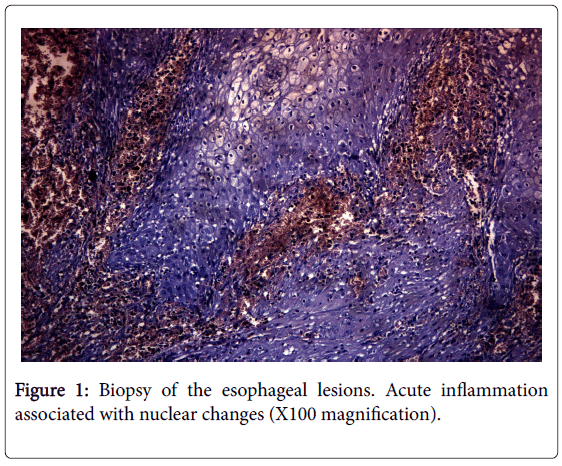
Focal high grade dysplasia and intraepithelial inflammation associated with nuclear changes were found by biopsies; due the possibility of human papilloma virus (HPV) infection, in situ hybridization studies for HPV were performed and it was positive for subtype 16.
The patient underwent endoscopic ultrasound that demonstrated that the changes were limited to the mucosa without penetration into the muscolaris mucosa.
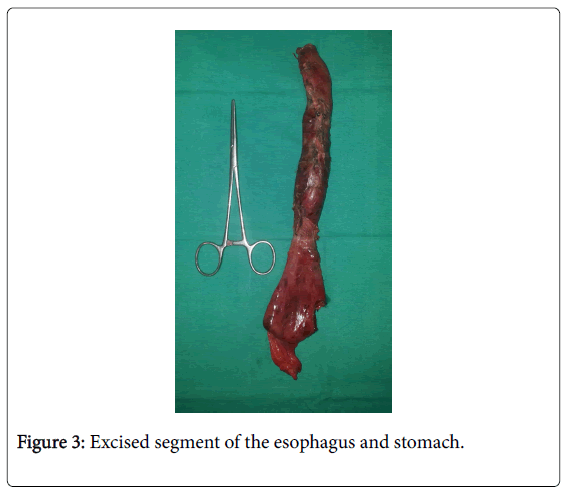
A chest computed tomograpy showed dilated appearing esophagus with a thickening of the mid-distal wall, extending from 15.5 cm to the gastroesophageal junction. Due to the severity of clinical findings we have made a total esophagectomy with gastro-pharyngeal anastomosis.
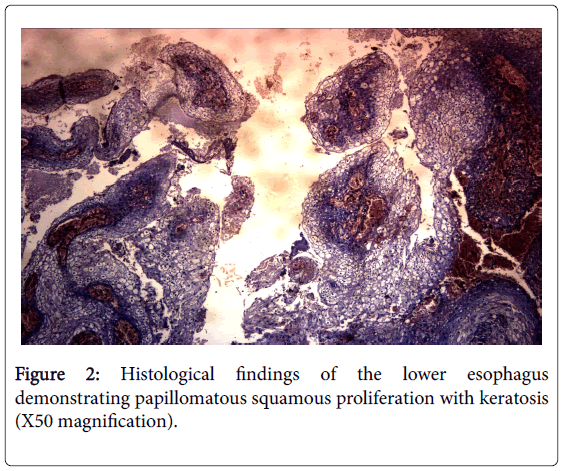
On histological examination of the esophagus, an extensive papillomatosis with diffuse low grade and focal high grade dysplasia was found.The inflammatory infiltrate was chiefly lymphocytic and it formed a dense band, typically observed in Lichen Planus (LP) (Figures 1 and 2). Thus we diagnosed diffuse papillomatosis of the esophagus complicated by esophageal lichen planus and HPV 16 infection in patient HCV positive.
Initial follow-up, six months after esophagectomy, was negative for new papillomas but positive only for granulation tissue. Follow-up endoscopy, one year later, revealed three flesh-coloured peduconlated papules at the gastro-pharyngeal anastomosis; we elected to proceed with endoscopic ablative therapy using the radiofrequency.
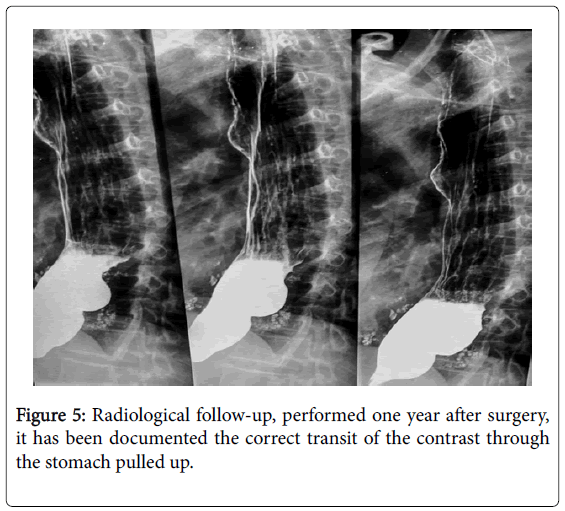
To radiological follow-up, performed one year after surgery, it has been documented the correct transit of the contrast medium through the stomach pulled up.
Discussion
In literature, small isolated lesions have been successfully treated with endoscopic resection, snare polypectomy and cautery [6] but the management of multiple esophageal lesions is more difficult and, due to scarcity reported cases treated in literature, the optimal clinical management of diffuse papillomatosis remains unclear. Photodynamic therapy and radiofrequency ablation may also be useful treatment options [7].
To our knowledge, the present report describes the first successful removal of multiple esophageal squamous papillomas using total esophagectomy and ablation by radiofrequency in second time of residual lesions (Figure 3). In some case, squamous papillomas have the potential for malignant transformation but the optimal management of these lesions has not been established; however, removal of these lesions during endoscopy using radiofrequency is a reasonable option.
Conclusion
Our patient, differs from most cases of esophageal papillomatosis reported in the literature in that, endoscopy therapy using injection therapy of an antiviral drug or removal by piecemeal polypectomy techniques used only in cases with a limited number of lesions, instead, in this case report the massive amount of papillomatous tissue occluding the esophageal lumen and it required treatment with surgery.
In the majority of the cases, squamous cell papilloma (SCP) of the esophagus can be removed using endoscopic biopsy forceps because most are only a few millimeters in size (Figure 4). Larger papillomas can be removed using endoscopic mucosectomy (Figure 5). This case underscores the importance of optimizing treatment results by combining the use of surgery and the endosopic modalities for the ablation of residual lesions.
References
- Adler RH, Carberry DM, Ross CA (1959) Papilloma of the esophagus: Association with hiatal hernia. J Thorac Surg 37: 625-635.
- Mosca S, Manes G, Monaco R, Bellomo PF, Bottino V, et al. (2001) Squamous papilloma of the esophagus: Long-term follow up. J Gastroenterol Hepatol 16: 857-861.
- Attila T, Fu A, Gopinath N, Streutker CJ, Marcon NE (2009) Esophageal papillomatosis complicated by squamous cell carcinoma. Can J Gastroenterol 23: 415-419.
- zur Hausen H (2002) Papillomaviruses and cancer:from basic studies to clinical application. Nat Rev Cancer 2: 342-350.
- Doorbar J (2005) The papillomavirus life cycle. J Clin Virol 32: 7-15.
- Tabatabaei SA, Moghadam NA, Ahmadinejad M, Mirmohammadsadeghi A, Masoudpour H (2009) Giant esophageal squamous papilloma: A case report. J Dig Dis 10: 228-230.
- Kibria R, Akram S, Moezzi J, Ali S (2009) Esophageal squamous papillomatosis with dysplasia. Is there a role of balloon-based radiofrequency ablation therapy? Acta Gastroenterol Belg 72: 373-376.
- Tonna J, Palefsky JM, Rabban J, Campos GM, Theodore P, et al. (2010) Esophageal verrucous carcinoma arising from hyperkeratotic plaques associated with human papilloma virus type 51. Dis Esophagus 23: 17-20.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11322
- [From(publication date):
October-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 10616
- PDF downloads : 706