Case Report Open Access
Total Colectomy with an Ileorectal Anastomosis: Perforation of Distal Portion of the Terminal Ileum
Rubén Gonzalo González1*, Sara Regano Diez1, Maria Antonia de Andrés Fuertes1, José Luis Conty S1, Adela Delgado Tapia2 and Francisco Javier Gil Piedra11Department of General Surgery, Hospital Laredo, Spain
2Department of Radiology, Hospital Laredo, Spain
- *Corresponding Author:
- Rubén Gonzalo González
Department of General Surgery, Hospital Laredo
Av Human Rights, s/n, 39770 Laredo
Cantabria, Spain
Tel: 620 108 834
E-mail: rubsoygg@hotmail.com
Received date: July 16, 2015 Accepted date: August 13, 2015 Published date: August 20, 2015
Citation: González RG, Diez SR, de Andrés Fuertes MA, Conty SJL, Tapia AD, et al. (2015) Total Colectomy with an Ileorectal Anastomosis: Perforation of Distal Portion of the Terminal Ileum. J Gastrointest Dig Syst 5:323. doi:10.4172/2161-069X.1000323
Copyright: © 2015 González RG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Total colectomy followed by ileorectal anastomosis is an established operation that may be employed as a surgical solution for a variety of colonic diseases. Postoperative morbidity and mortality rates are generally regarded as low, and functional outcome is rated as good to excellent by most patients. The ileorectal anastomosis is usually latero-terminal and is constructed with staples. If the segment of terminal ileum extending past the site of the anastomosis is too long, it remains as an appendage, and this portion of bowel may fold or twist upon itself, thus creating an intermittent closed-loop obstruction of its tip, leading to localized perforation, sepsis, and eventual fistula formation. The case of one patient who developed significant complications arising from this portion of the bowel is reported.
Abstract
Total colectomy followed by ileorectal anastomosis is an established operation that may be employed as a surgical solution for a variety of colonic diseases. Postoperative morbidity and mortality rates are generally regarded as low, and functional outcome is rated as good to excellent by most patients. The ileorectal anastomosis is usually latero-terminal and is constructed with staples. If the segment of terminal ileum extending past the site of the anastomosis is too long, it remains as an appendage, and this portion of bowel may fold or twist upon itself, thus creating an intermittent closed-loop obstruction of its tip, leading to localized perforation, sepsis, and eventual fistula formation. The case of one patient who developed significant complications arising from this portion of the bowel is reported.
Keywords:
Total colectomy; Ileorectal anastomosis; Intestinal perforation; Mechanical suture
Introduction
Total colectomy (TC) with ileorectal anastomosis (IRA) is a relatively frequent procedure today. Indications are well defined, functional results are compatible with an almost normal quality of life, and postoperative morbidity and mortality rates are low [1-5]. TC can be performed through laparotomy or laparoscopy; IRA can be manual or mechanic, end-to-end or side-to-end. When performing side-to-end mechanical IRA, the circular stapler head is first introduced through the end of the ileum, leaving 5 cm of terminal ileum distal to the anastomosis, and the circular stapler is introduced through the anus. The stapler is then assembled and the anastomosis is completed. This end of distal ileum may act as an appendix or blind loop if it is too long. We present the case of a patient with a serious complication stemming from this portion of distal ileum.
Case Report
This 64-year-old male patient had no previous significant medical history. Previous surgeries included laparoscopic TC with mechanical side-to-end IRA 10 years earlier to treat a synchronous colonic adenocarcinoma located at the sigmoid and the transversal colon (T3N0M0). Currently, he continued periodic follow-up visits and annual rectal endoscopy carried out by the Digestive Department with no significant findings.
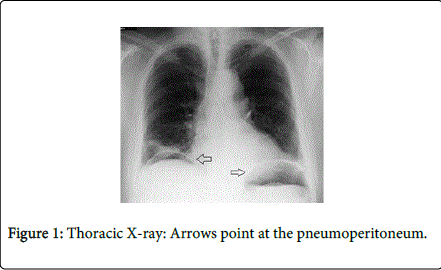
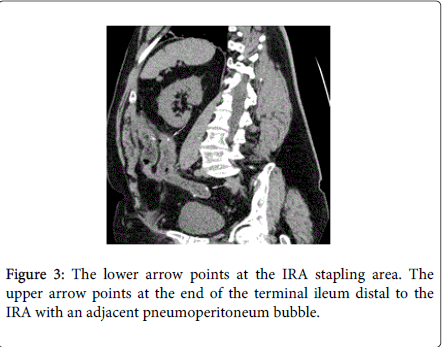
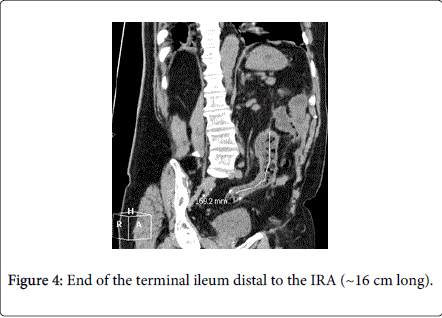
He presented to the emergency department with abdominal pain at the left hemiabdomen. He had been suffering from this pain for the last 15 days, and in the last 12 hours, it increased sharply. He presented with nausea without emesis. His last bowel movement 24 hours earlier was reported to be normal. He had a temperature (38ºC) and was conscious and oriented, and was well hydrated, with normal color. Cardiopulmonary auscultation was normal. The abdomen was distended and tympanic. Palpation at the left hemiabdomen was painfulbut there was no guarding. No masses or hernias are palpated. The hemogram revealed leukocytosis (14,000 leukocytes with 75% neutrophils) and an increased C-reactive protein (10.70 mg/dL). Renal function, pancreatic enzymes, and hepatic profile were normal. Simple thoracic X-ray demonstrated a significant pneumoperitoneum (Figure 1). An urgent abdominal CT scan was performed. It showed the presence of a remarkable pneumoperitoneum at the intra-abdominal level, and a small bowel loop on the left side with a thickened/inflammatory appearance with significant fraying of peripheral fat and a minimal amount of adjacent liquid (corresponding to the terminal ileum segment distal to the IRA). The possibility of this process being the origin of the current pneumoperitoneum could not be excluded.
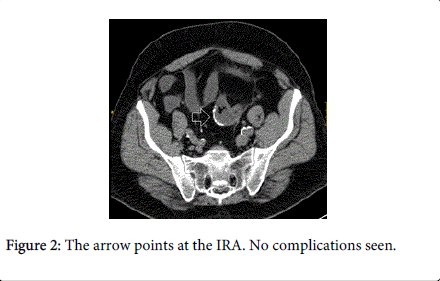
At the pelvic level, the IRA was seen without complications (Figures 2-4). The decision was made to perform a median laparotomy which revealed purulent peritonitis secondary to a perforation on the border of the terminal ileum distal to the IRA. This approximately 15-cm-long small bowel segment (as an appendix or blind loop) was hypertrophic, thickened, and dilated. No additional pathological findings were seen at the IRA or in the rest of the abdominal cavity.
Resection was carried out using the GIA (gastrointestinal anastomosis) stapler, followed by intussusception of the stapling line, washing of the abdominal cavity, and placing of a drainage. Owing to a persistent hematic drainage, the patient was reoperated on three days following the first procedure. A small laceration was identified at the lower pole of the spleen. Therefore, splenectomy was performed. Subsequently, due to the presence of collection at the splenic fossa and a left pleural bleeding, a percutaneous drainage was performed in both. The patient was discharged 4 weeks after admission. He is currently asymptomatic.
Discussion
TC with IRA is a relatively frequent procedure in both elective and emergency surgery today. Indications include colon cancer (familial adenomatous polyposis, hereditary nonpolyposis colorectal cancer, synchronous tumors), inflammatory bowel disease (Crohn’s disease and ulcerative colitis), functional disorders (megacolon/megarectum, colonic inertia), and less frequent pathologies (diverticular disease, ischemic/infectious colitis) [4]. It should first be confirmed that the patient has normal sphincter tone without perianal disease and has adequate rectal distensibility without evidence of dysplasia or cancer before performing the procedure. Also, the intervention can be carried out in a transitory fashion in young patients who do not want their fertility to be affected [5].
Physiologic adaptation to TCn is very satisfactory, and functional results are compatible with an almost normal quality of life. Indeed, 90% of patients achieve normal continence and have four bowel movements daily on average [6-8]. Morbidity and mortality rates are around 26% and 1% (0-6%) respectively (the rate being higher in Crohn’s disease and functional disorder patients) [4], The surgical re-intervention rate is ~7.5% [4,7]. The most frequent postoperative complication described in the literature is intestinal obstruction. Various series report rates of 2-70% associated with adhesions, abnormal motility in functional disorder groups, and recurrence of Crohn’s disease, although laparoscopy has reduced obstruction to 20%. Other significant complications are anastomosis dehiscence (6.5%), surgical wound infection (8.8%), rectovaginal fistula (5.5%), and anastomosis stenosis [4]. In our case, the patient presented with an intestinal perforation at the terminal ileum distal to the IRA, which is an extremely rare complication.
Side-to-end mechanical IRA is the most frequently performed anastomosis. It is created by introducing the head of the circular stapler through the end of the ileum and perforating the anti-mesenteric border, leaving 5 cm of ileum distal to the anastomosis. The circular stapler is introduced through the anus and assembled with its head to perform anastomosis at the level of the promontory. This method should help in carrying a better irrigated ileum border to the rectum, which proves advantageous.
The end of the ileum is closed using a mechanical stapler or manual suture. We have found no evidence which defined the optimal length or the ideal type of suture of the distal ileum in side-to-end IRA [9]. Perforation in this portion of the terminal ileum is rare. In the immediate postoperative course, it usually stems from an ischemic problem.
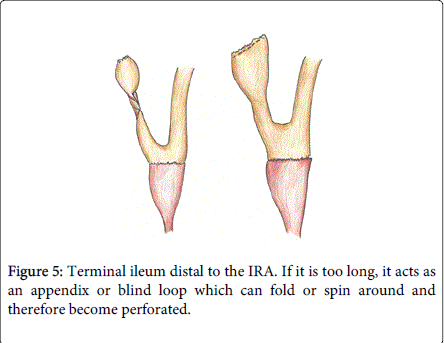
However, if this segment is too long, we think that with time- as in our case- it acts as an appendix or blind loop, which causes a bacterial overgrowth that could predispose to torsion and/or perforation (Figure 5).
This complication can be easily avoided by sectioning the terminal ileum distal to the IRA as close as possible to the anastomosis when it is performed.
In patients undergoing TC with IRA presenting to the emergency department with acute abdomen, we should consider intestinal obstruction as the root of the problem, and we should not forget that the end of the terminal ileum distal to the IRA can be the cause if it was left too long. In the literature, we have found only two similar cases to the one described as a result of leaving an excessively long terminal ileum appendix when performing a repairing proctocolectomy with an ileoanal J-pouch [10,11].
In conclusion, TC with IRA is a safe procedure with optimal functional results in selected patients and with a low morbidity/mortality rate. There is a high incidence of intestinal obstruction following surgery, and a significant number of patients will require surgical re-intervention. Intestinal perforation of the terminal ileum distal to the anastomosis is a rare complication. If it is too long, it acts as an appendix or blind loop which can fold or spin around, creating an intermittent obstruction at the tip, which may cause perforation.
References
- Aylett SO (1966) Three hundred cases of diffuse ulcerative colitis treated by total colectomy and ileo-rectal anastomosis. Br Med J 1: 1001-1005.
- Iacconi P, Aldi R, Bucceri R, Bendinelli C, Barsotti F, et al. (1996) [Total colectomy with ileorectal anastomosis (IRA): our experience in 57 patients]. G Chir 17: 231-234.
- Eu KW, Lim SL, Seow-Choen F, Leong AF, Ho YH (1998) Clinical outcome and bowel function following total abdominal colectomy and ileorectal anastomosis in the Oriental population. Dis Colon Rectum 41: 215-218.
- da Luz Moreira A, Kiran RP, Lavery I (2010) Clinical outcomes of ileorectal anastomosis for ulcerative colitis. Br J Surg 97: 65-69.
- Elton C, Makin G, Hitos K, Cohen CR (2003) Mortality, morbidity and functional outcome after ileorectal anastomosis. Br J Surg 90: 59-65.
- Pastore RL, Wolff BG, Hodge D (1997) Total abdominal colectomy and ileorectal anastomosis for inflammatory bowel disease. Dis Colon Rectum 40: 1455-1464.
- Soravia C, Klein L, Berk T, O’Connor BI, Cohen Z, et al. (1999) Comparison of ileal pouch-anal anastomosis and ileorectal anastomosis in patients with familial adenomatous polyposis. Dis Colon Rectum 42: 1028-1034.
- Günther K, Braunrieder G, Bittorf BR, Hohenberger W, Matzel KE (2003) Patients with familial adenomatous polyposis experience better bowel function and quality of life after ileorectal anastomosis than after ileoanal pouch. Colorectal Dis 5: 38-44.
- Scoglio D, Ahmed Ali U, Fichera A (2014) Surgical treatment of ulcerative colitis: ileorectal vs ileal pouch-anal anastomosis. World J Gastroenterol 20: 13211-13218.
- Bannura BG, Barrera EA, Contreras PJ, Melo LC, Soto CD, et al. (2005) Colectomía total e ileorrectoanastomosis mecánica: análisis de 45 pacientes consecutivos. Rev Chil Cir 57: 213-219.
- Pezim ME, Taylor BA, Davis CJ, Beart RW Jr (1987) Perforation of terminal ileal appendage of J-pelvic ileal reservoir. Dis Colon Rectum 30: 161-163.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 21066
- [From(publication date):
August-2015 - Jul 14, 2025] - Breakdown by view type
- HTML page views : 16422
- PDF downloads : 4644