Tobacco Smoking Life Cycle; Factors Associated to Smoking Initiation and Quitting in a Sample of Lebanese Adults
Received: 22-Jul-2019 / Accepted Date: 18-Jan-2020 / Published Date: 27-Jan-2020 DOI: 10.4172/2161-0711.1000675
Abstract
Aim: This study aimed at evaluating the effect of personal factors in the occurrence of smoking initiation and quitting in Lebanon.
Methods: a retrospective cohort of 621 Lebanese adults recruited from community pharmacies in Mount Lebanon and Beirut districts, to detect the events: ever smoker and former smoker.
Results: Out of the 621 participants 55.6% were ever smokers and 6.4% former smokers. The association between survival curves of males (RR=0.340, p<0.001), having smoker family member (RR=2.087, p<0.001), exposed to tobacco smoke (RR=1.201, p=0.019), got higher education (RR=0.667, p<0.001), household crowding index (RR=1.396, p=0.025) were highly significant for smoking initiation while for quitting smoking, cancer (RR=2.844, p-0.028), age of smoking initiation (RR=1.089, p<0.001) and cardiovascular diseases (RR=0.193, p<0.001) were significantly associated.
Conclusion: Smoking initiation is highly associated with personal factors like gender, family influence and exposure to second-hand smoke, socioeconomic and education levels whereas quitting was highly associated with the health status.
Keywords: Smoking initiation; Quitting smoking; Health risks; Environmental influence; Socioeconomic level; Ever smoker; Former smoker
Introduction
“Tobacco is the only legal drug that kills many of its users when used exactly as intended by manufacturers”. WHO has estimated that it is responsible for the death for millions of people each year due to communicable as well as non-communicable diseases [1]. Current smoking prevalence is estimated to be 33.4% in Lebanon for both sexes and is projected to be 33.5% in 2025 [2] despite all the efforts to reduce these rates and the implementation of tobacco control policies.
Smoking initiation can be due to many factors, like biological factors (genetic predisposition) [3] as well as sociodemographic factors. For instance, in eastern Mediterranean countries, men got higher rates of smoking than women [4,5] since smoking is socially more accepted in men. Furthermore, the person’s surrounding got a great influence on the decision to initiate smoking. Persons who got family members and friends smoking are at higher risk of becoming smokers [6-8] Second hand smoke emission is also an important predictor of smoking initiation [9]. Factors dictating socioeconomic level are also key elements in this issue like education [10] and household crowding index [11]. Urban residency [12] is also important. What is also thought to be a key determinant is the health status like for instance being diagnosed with a respiratory disease [13].
Factors associated with quitting smoking are also numerous. Quitting is made harder due biological factors (genetic predisposition and severe withdrawal symptoms) [14], as well as sociodemographic factors like stress levels [15], family influence and a variety of other factors. One other important predictor of quitting is the age of smoking initiation [16] so that the younger the age of smoking initiation, the harder quitting will become. Health status may dictate and facilitate the willingness and ability to quit smoking. It has been shown that the quality of life of patients with respiratory disease like chronic obstructive pulmonary disease (COPD) is decreased by smoking [13] and cardiovascular disease mortality was reduced by intensive smoking cessation treatment [17], as for the mortality from lung cancer for example was reduced with early smoking cessation interventions [18].
To our knowledge, this is the first study in Lebanon that considered the time factor effect on the occurrence of smoking initiation and quitting. Our aim was to evaluate the role played by personal factors in the occurrence of smoking initiation and quitting in the Lebanese population.
Data and Methods
Population of the study
A retrospective cohort of 621 participants recruited from community pharmacies over 18 months from Greater Beirut and Mount Lebanon districts. Included participants are Lebanese adults who were able to read and understand Arabic.
Ethical aspect
The study protocol was approved by the institutional review board of Saint-Joseph University of Beirut, Lebanon (USJ-2016-53). An informed written consent was signed by each participant prior to recruitment.
Survey tool
Data collection was performed through a questionnaire filling: socio-demographic information (age, gender, educational level, smokers in the surrounding, urban residency, etc.). The smoking status was defined as follows: active smokers (participants who are actively smoking water pipe and/or cigarette) never smoked (participants who never smoked any type of tobacco) and former smokers (participants who quitted smoking at the time of recruitment).
The questionnaire was written in English and was translated to Arabic. The translation process was as follows: First, a bilingual researcher forward-translated the questions into Arabic, then a second independent translator with no knowledge of the questionnaire, backtranslated the questions into English. Translation discrepancies were resolved by consensus between the researchers and the translator. These questions were pretested in a pilot sample of 20 individuals before being adopted in the final questionnaire. These 20 individuals were included in the final database since there was no major corrections to the questions.
Outcomes definition
A regular cigarette smoker is defined as “an adult who has smoked 100 cigarettes in his or her lifetime and who currently smokes cigarettes” [19]. Since there is no official definition of regular waterpipe smoker, we consider a person who smoke one or more waterpipe per week as a regular smoker [20]. A former smoker is “an adult who has smoked at least 100 cigarettes in his or her lifetime but who had quit smoking at the time of interview” [19]. The WHO defined “exposed to second hand “as the smoke emitted from the burning end of a cigarette or from other tobacco products usually in combination with the smoke exhaled by the smoker” [21].
Event detection and time assessment
The following two outcomes: “ever smoking” (becoming a regular smoker) and then “quitting smoking” (becoming a previous smoker) were detected following the answer of the participants to the following questions “have you ever smoked any type of tobacco (cigarette or waterpipe)”, “are you currently smoking”, if no “for how long you quitted smoking”, if yes, “what type” “cigarette (specify quantity per day)”, “waterpipe (specify quantity per week)”. The control group for the event “ever smoker” was “never smoker”. On the other hand, we considered “ever smoker” as a control group for “Former smoker”
Declared age at first smoking was used to assess smoking initiation time, and declared total smoking duration to assess the time of smoking cessation for those who stopped smoking.
Statistical analysis
Data entry and analysis were performed using the Statistical Package for the Social Sciences (SPSS) version 24. Observed survival curves were generated using the COX regression. To decrease confounding factors, Chi-square test and student t-test were used in the bivariate analysis and variables that showed a p<0.2 were taken as independent variables in the final model. The Cox proportional hazards regression model was applied to identify hazard ratios for the outcomes measured, after ensuring the proportional hazard hypothesis adequacy. For all statistical tests, a p<0.05 was considered statistically significant.
Results
Population description
This sample consisted of 621 participants with mean age of 40.39 ± 13.81 years, where 38% were never smoker, 6.4% were former smokers and 55.6% were ever smokers (58% smoked cigarettes, 32% smoked water pipe and 10% smoked both types of tobacco). Furthermore, 58.2% were of male gender, 56.1% had at least one smoker at home, and 35.8% were exposed to this smoke. In this sample, 50.3% got a university degree, 83.5% were currently students and/or in the work place, 55.5% were currently big city residents and the overall house crowding index was 1.01 ± 0.38. Concerning the health status, 4.1% suffered from a respiratory disease, and 9.5% had a family member suffering from cancer.
Bivariate analysis
Ever smoking related factors: Concerning the outcome “ ever smoking”, a significantly higher proportion of smokers were males (69.6% vs. 41.5%), had a smoker at home (68.4% vs. 38.1%), were exposed to smoke (44.3% vs. 23.3%), had lower education level, were big city residents, and had higher mean of household crowding index compared to those without any event. We did not detect any significant association between ever smoking and current health status (cancer, respiratory disease or any other disease state) (p>0.05) (Table 1).
| Ever smoking | P value | HR | 95%CI | ||
|---|---|---|---|---|---|
| Never smoker | Ever smoker | ||||
| Gender | |||||
| Male | 98 (41.5%) | 240 (69.6%) | <0.001*** | 0.454 | 0.361-0.571 |
| Female | 138 (58.5%) | 105 (30.4%) | |||
| Smoker at home | |||||
| No | 146 (61.9%) | 109 (31.6%) | <0.001*** | 2.122 | 1.693-2.659 |
| Yes | 90 (38.1%) | 236 (68.4%) | |||
| Exposed to smoke | |||||
| No | 181 (76.7%) | 192 (55.7%) | <0.001*** | 1.425 | 1.251-1.624 |
| Yes | 55 (23.3%) | 153 (44.3%) | |||
| Education level | |||||
| Non-university degree | 98 (41.5) | 191 (55.4%) | 0.001** | 0.695 | 0.561-0.859 |
| University degree | 138 (58.5%) | 154 (44.6%) | |||
| Household crowding index | 0.928 ± 0.346 | 1.067 ± 0.399 | <0.001*** | 1.952 | 1.529-2.493 |
| City residency | |||||
| Non-big city resident | 122 (51.9%) | 136 (39.4%) | 0.004** | 1.383 | 1.114-1.716 |
| Big city resident | 113 (48.1%) | 209 (60.6%) | |||
| Current respiratory disease | |||||
| No | 221 (94%) | 335 (97.1%) | 0.069 | 0.633 | 0.337-1.188 |
| Yes | 14 (6%) | 10 (2.9%) | |||
| Duration of respiratory disease | 19.71 ± 13.09 | 11 ± 10.23 | 0.093 | 0.963 | 0.927-1.000 |
*Among participants with a respiratory disease.
Table 1: Factors associated with ever smoking.
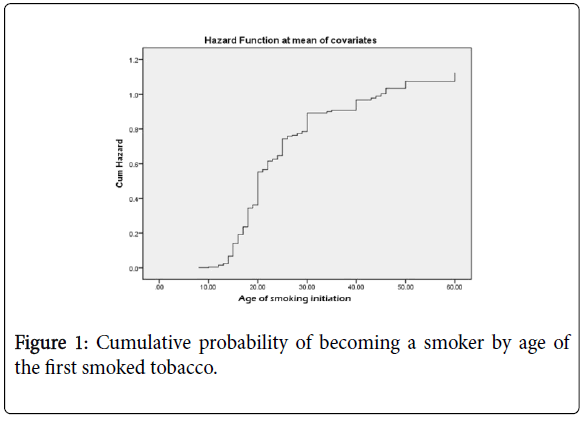
Moreover, the mean age for starting smoking was 19.94 (SD=6.89) the minimal age to start smoking was 8 years, and the maximal age was 60 years The cumulative probability of becoming a regular smoker is presented in Figure 1.
Factors related to quitting smoking
Concerning the outcome “quitting smoking”, a significantly higher proportion of participants who quitted smoking had a respiratory disease, cancer in the family and suffered from a cardiovascular disease. Quitters also had a higher mean age at smoking initiation (49.93 ± 15.37 vs. 19.94 ± 6.90) compared to those who still smoke (Table 2). The mean age for quitting smoking is 45.78 (SD=13.75). The minimal age for quitting smoking was 22 years, and the maximal age was 80 years. The cumulative probability of quitting smoking is shown in Figure 2.
| Quitting smoking | P value | Unadjusted HR | 95%CI | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Current respiratory disease | |||||
| No | 335 (97.1%) | 36 (90%) | 0.047* | 2.988 | 1.060-8.427 |
| Yes | 10 (2.9%) | 4 (10%) | |||
| Cancer in the family | |||||
| No | 315 (91.3%) | 33 (82.5%) | 0.073 | 1.85 | 0.817-4.186 |
| Yes | 30 (8.7%) | 7 (17.5%) | |||
| Current cardiovascular disease | |||||
| No | 311 (90.1%) | 31 (77.5%) | 0.023* | 1.443 | 0.695-2.999 |
| Yes | 34 (9.9%) | 9 (22.5%) | |||
| Age (years) at the first smoked tobacco | 19.94 ± 6.90 | 34.88 ± 15.37 | <0.001*** | 1.067 | 1.053-1.082 |
Table 2: Factors associated with quitting smoking.
Multivariable analyses
The first COX regression taking the outcome “ever smoking” as the dependent variable and the age of starting tobacco smoking as the time variable, showed that having a smoker at home (HR= 2.087), being exposed to smoke at home (HR=1.201) and higher mean of the household crowding index (HR=1.396) were significantly and positively associated with regular smoking initiation. On the other hand, being a female (HR=0.430) and having a higher education level (HR=0.667) were inversely associated with smoking initiation (Table 3).
| COX regression taking the fact of becoming a smoker as dependent variable | |||
|---|---|---|---|
| Hazard Ratio (HR) | 95%CI | P value | |
| Female vs. Malea | 0.43 | 0.341-0.542 | <0.001*** |
| Having a smoker at home vs. not having a smoker at homea | 2.087 | 1.645-2.648 | <0.001*** |
| Exposed to smoke vs. non exposeda | 1.201 | 1.030-1.400 | 0.019* |
| University degree vs. non-university degreea | 0.667 | 0.538-0.827 | <0.001*** |
| Household crowding index | 1.396 | 1.042-1.871 | 0.025* |
| Variables entered: gender, smoker at home, exposure to smoke, education level, household crowding index, city residency, respiratory disease, duration of respiratory disease. | |||
| COX regression taking the fact of quitting smoking as dependent variable | |||
| Hazard Ratio (HR) | 95%CI | P value | |
| Cancer in the family vs. no cancera | 2.844 | 1.123-7.206 | 0.028* |
| Age of smoking initiation | 1.089 | 1.070-1.109 | <0.001*** |
| Current cardiovascular disease vs. no diseasea | 0.193 | 0.073-0.507 | 0.001** |
Variables entered: age (years) at the first smoked tobacco, work status, cancer in the family, current cardiovascular disease, current respiratory disease.
aReference value
Table 3: Multivariable analyses for “ever smoking” and “quitting smoking” outcomes.
The second COX regression taking the outcome “quitting smoking” as the dependent variable, and the duration of smoking as the time variable, showed that having cancer in the family (HR=2.844), and a later age of smoking initiation (HR=1.089), were significantly and positively associated with quitting smoking, while having a cardiovascular disease was inversely associated with quitting smoking (HR=0.193).
Discussion
To our knowledge, this is the first study in Lebanon that analyses the smoking vicious circle. The genetic predisposition and the environmental factors play important roles in smoking initiation especially when it comes to socializing with peers [12]. Quitting smoking is governed not only by environmental and genetic factors, it is also strongly affected by the severity of withdrawal syndrome causing high relapse rates and quitting failures [22]. For instance, our results reflected this fact and showed that 55.6% of the participants were ever smokers, while only 6.4% succeeded in quitting.
The survival cumulative probability of becoming a smoker by age of the first smoked tobacco showed that earlier age of starting smoking is a strong predictor of becoming more addicted to tobacco. Evidence stresses on the reduction of smoking initiation in adolescents to avoid addiction since young people are particularly vulnerable to nicotine addiction [23].
Other important predictors of smoking initiation are living in smokers surrounding and being exposed to second hand smoke [9,12,24]. In fact, early exposure to second hand smoke was shown to significantly predict smoking initiation. This may be explained by the increased risk for biological addictive effect due to nicotine found in smoke [25]; for instance, in Lebanon and other eastern Mediterranean countries, exposure to tobacco smoke from a water pipe [26] and/or cigarette was shown to be a strong predictor for smoking initiation [9]. Another important predictor is the socioeconomic status since people of lower socioeconomic status were more likely to start smoking, to become regular smokers, and less likely to quit [27] Household crowding index is a good reflection of this factor, so that an index less or equal to 1 indicated a higher socioeconomic status. In a study done in Lebanon about the social context of smoking, the household crowding index was higher in the smoker group than in the nonsmokers [11].
On the other hand, factors allowing the protection smoking initiation are also numerous. For instance, higher education level allows for higher harm perception [28,29] and thus may help a person in decision making about initiating smoking. Conversely, in our study, never smokers were more likely to continue their education to higher levels, while smokers were less likely to go for higher education. This fact goes along with the effect of the socioeconomic status. So that higher socioeconomic level is associated with higher education in a person’s family of origin who would teach him about health and wellbeing. These people are more likely to continue their academic achievements and to be less predisposed to smoking initiation [30]. Women are also at lower risk to initiate smoking compared to men [28]. In a study by Salameh it was shown that women got lower smoking prevalence but had higher risk of water pipe dependence than men, since water pipe smoking is becoming more and more acceptable for women than cigarette smoking [4,31,32].
Willing to quit smoking is associated with many biological as well as environmental factors making it a difficult decision to make. In fact, withdrawal syndrome plays a key role in preventing quitting. An important driving force remains the health status. For instance, having a family member with cancer [33] is a strong predictor of quitting smoking since the diagnosis of a family member with cancer has a strong impact on his surrounding, so that his relatives might try stopping smoking particularly if this benefits the recovery of the patient. In a study on lung cancer, 75% of patents’ relatives reported that the diagnosis had increased their desire to quit smoking.
Furthermore and as was mentioned previously, an earlier age of smoking initiation is a strong predictor of becoming a regular smoker and may delay quitting, [28,34]. Finally, in this study, cardiovascular diseases were inversely associated with quitting smoking contradicting what is shown in other studies. Evidence has established smoking is an important cause of cardiovascular diseases morbidity and mortality since smoke exposure promotes vascular dysfunction and atherogenesis [35]. This issue may be due to the lack of reinforcement and adequate education given to the cardiac smokers by their healthcare providers [36]. Additional efforts need to be taken in this regard, particularly given that cardiovascular diseases in Lebanon are highly prevalent, among smokers in particular [37].
Limitations
This study has several limitations. First, the small sample size of former smokers that put some limitations to the analysis. Second, a selection bias is possible, since the participants were recruited from Beirut and Mount Lebanon pharmacies, so this sample does not geographically represent the whole general Lebanese population and might even over or underrepresent subjects with chronic and infectious diseases. This may have prevented us from showing that respiratory diseases are predictors of smoking quitting due to the small sample size of participants with respiratory disease. It may have also affected the results with participants with cardiovascular disease as well those having a family member with cancer. There are also different information biases present in the study, since the information was selfreported. Finally, the factors affecting quitting smoking are numerous, including the genetic factors, which may constitute a residual confounding that was not taken into account in this analysis. Future studies where the pharmacogenomics of nicotine dependence will be taken into consideration are recommended.
Despite the study ’ s limitation, we recommend that authorities deploy further efforts to inhibit smoking initiation among adolescents and young nonsmokers, and to encourage smoking cessation among smokers, to avoid smoking related health risks. It is also recommended that healthcare providers work to promote smoking cessation among patients, especially for those with cancer or cancer predisposition and chronic diseases like respiratory and cardiovascular conditions.
Conclusion
Smoking initiation is highly associated with personal factors like gender, family influence and exposure to second-hand smoke, socioeconomic and education levels. Quitting on the other hand is highly associated with health status of the person or family members. Efforts should be made to prevent smoking initiation and to help smokers in quitting.
References
- World Health Organization (2015) WHO global report on trends in prevalence of tobacco smoking 2015. Geneva.
- World Health Organization (2018) WHO global report on trends in prevalence of tobacco smoking 2000-2025. Geneva.
- Lessov-Schlaggar CN, Pergadia ML, Khroyan TV, Swan GE (2008) Genetics of nicotine dependence and pharmacotherapy. Biochem Pharmacol 75: 178-195.
- Maziak W, Rastam S, Eissenberg T, Asfar T, Hammal F, et al. (2004) Gender and smoking status-based analysis of views regarding waterpipe and cigarette smoking in Aleppo, Syria. Prev Med 38: 479-484.
- World Health Organization (2000) Gender, women, and the tobacco epidemic. Tobacco Free Initiative. Geneva.
- Roupa Z (2016) The effect of family and social environment on smoking behaviour in adolescence. Eur Sci J 12: 62-80.
- Albers AB, Biener L, Siegel M, Cheng DM, Rigotti N (2008) Household smoking bans and adolescent antismoking attitudes and smoking initiation: Findings from a longitudinal study of a Massachusetts youth cohort. Am J Public Health 98: 1886-1893.
- Richardson J, Flay BR, Sussman S, Petraitis J, Siddiqui O, et al. (2006) Differential influence of parental smoking and friends’ smoking on adolescent initiation and escalation and smoking. J Health Soc Behav 35: 248.
- Jawad M, Nakkash RT, Mahfoud Z, Bteddini D, Haddad P, et al. (2015) Parental smoking and exposure to environmental tobacco smoke are associated with waterpipe smoking among youth: Results from a national survey in Lebanon. Public Health 129: 370-376.
- Zhou L, Niu L, Jiang H, Jiang C, Xiao S (2016) Facilitators and barriers of smokers’ compliance with smoking bans in public places: A systematic review of quantitative and qualitative literature. Int J Environ Res Public Health 13: 1228.
- Bejjani N, El Bcheraoui C, Adib SM (2012) The social context of tobacco products use among adolescents in Lebanon (MedSPAD-Lebanon). J Epidemiol Glob Health 2:15-22.
- Griffiths MA, Harmon TR, Gilly MC (2011) Hubble Bubble Trouble: The Need for Education About and Regulation of Hookah Smoking. J Public Policy Mark 30: 119-132.
- Joseph S, Pascale S, Georges K, Mirna W (2012) Cigarette and waterpipe smoking decrease respiratory quality of life in adults: Results from a national cross-sectional study. Pulm Med 2012: 868294.
- Zdanowicz MM, Adams PW (2014) The Pharmacogenetics of Nicotine Dependence and Smoking Cessation Therapies. J Pharmacogenomics Pharmacoproteomics 5: 1-20.
- Cohen S, Lichtenstein E (1990) Perceived stress, quitting smoking, and smoking relapse. Heal Psychol 9: 466-478.
- Johansen H, Nargundkar M, Nair C, Taylor G, elSaadany S (1998) At risk of first or recurring heart disease. Health Rep 9: 19-23.
- Hunter CB, Hilleman DE, Mohiuddin SM, Cloutier DA, Grollmes TL, et al. (2007) Intensive smoking cessation intervention reduces mortality in high-risk smokers with cardiovascular disease. Chest 131: 446-452.
- Peto R (2002) Smoking, smoking cessation, and lung cancer in the UK since 1950: Combination of national statistics with two case-control studies. BMJ 321: 323-329.
- Weitkunat R, Coggins CRE, Sponsiello-Wang Z, Kallischnigg G, Dempsey R (2013) Assessment of cigarette smoking in epidemiologic studies. Beitrage zur Tab Int Contrib to Tob Res 25: 638-648.
- Salameh P, Waked M, Aoun Z (2008) Waterpipe smoking: Construction and validation of the Lebanon Waterpipe Dependence Scale (LWDS-11). Nicotine Tob Res 10: 149-158.
- World Health Organisation (2007) Guidelines on protection from exposure to tobacco smoke. Geneva.
- Ward KD, Hammal F, VanderWeg MW, Eissenberg T, Asfar Tet al. (2005) Are waterpipe users interested in quitting? Nicotine Tob Res 7: 149-156.
- Marcon A, Pesce G, Calciano L, Bellisario V, Dharmage SC, et al. (2018) Trends in smoking initiation in Europe over 40 years: A retrospective cohort study. PLoS One 13: 1-14.
- Subramaniam M, Shahwan S, Fauziana R, Satghare P, Picco L, et al. (2015) Perspectives on smoking initiation and maintenance: A qualitative exploration among singapore youth. Int J Environ Res Public Health 12: 8956-8970.
- Wang MP, Ho SY, Lam TH (2011) Parental smoking, exposure to secondhand smoke at home, and smoking initiation among young children. Nicotine Tob Res 13: 827-832.
- Saade G, Seidenberg AB, Rees VW, Otrock Z, Connolly GN (2010) Indoor secondhand tobacco smoke emission levels in six Lebanese cities. Tob Control 19: 138-142.
- Gilman SE, Abrams DB, Buka SL (2003) Socioeconomic status over the life course and stages of cigarette use: Initiation, regular use, and cessation. J Epidemiol Community Health 57: 802–808.
- Chen J, Millar WJ (1998) Age of smoking initiation: Implications for quitting. Health Rep 9: 39-46.
- Creamer MR, Loukas A, Li X, Pasch KE, Case K, et al. (2016) College students’ perceptions and knowledge of hookah use. Drug Alcohol 168: 191-195.
- Maralani V (2014) Understanding the links between education and smoking. Soc Sci Res 48: 20-34.
- Salameh P, Khayat G, Waked M (2012) Lower prevalence of cigarette and waterpipe smoking, but a higher risk of waterpipe dependence in lebanese adult women than in men. Women Heal 52: 135-150.
- Afifi R, Khalil J, Fouad F, Hammal F, Jarallah Y, et al. (2013) Social norms and attitudes linked to waterpipe use in the eastern mediterranean region. Soc Sci Med 98: 125-134.
- McBride CM, Ostroff JS (2003) Teachable moments for promoting smoking cessation: The context of cancer care and survivorship. Cancer Control 10: 325-333.
- Jõgi R, Abramson MJ, Marcon A, Perret JL, Bousquet J, et al. (2019) Time and age trends in smoking cessation in Europe. PLoS One 14: e0211976.
- Ambrose JA, Barua RS (2004) The pathophysiology of cigarette smoking and cardiovascular disease: An update. J Am Coll Cardiol 43: 1731-1737.
- Stead LF, Bergson G, Lancaster T (2008) Physician advice for smoking cessation. Cochrane Database Syst Rev 16: CD000165.
- Zeidan RK, Farah R, Chahine MN, Asmar R, Hosseini H, et al. (2016) Prevalence and correlates of coronary heart disease: First population-based study in Lebanon. Vasc Health Risk Manag 12: 75-84.
Citation: Malhab SB, Khabbaz LR, Salameh P (2020) Tobacco Smoking Life Cycle; Factors Associated to Smoking Initiation and Quitting in a Sample of Lebanese Adults. J Community Med Health Educ 10: 675. DOI: 10.4172/2161-0711.1000675
Copyright: © 2020 Malhab SB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1979
- [From(publication date): 0-2020 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 1260
- PDF downloads: 719