To investigate the Need for Palliative Care in Cerebrovascular Accident (stroke) Patients at Ladysmith Regional Hospital
Received: 23-May-2020 / Accepted Date: 13-Jul-2020 / Published Date: 22-Jul-2020 DOI: 10.4172/2165-7386.1000368
Abstract
This research study explores the need for palliative care by the patients who are recovering from stroke after an acute event. Stroke survivors need comprehensive care for their physical, psychosocial, spiritual well-being and additional support. The comprehensive total care in all aspect of physical, social and spiritual well-being can only be offered by the holistic approach of palliative care focusing, as it does, on the rehabilitation for stroke survivors to improve their quality of life.
A literature review was conducted to investigate how palliative care can help to change the quality of life for stroke survivors. There has been little research on the topic of providing palliative care to stroke patients in South Africa. The aim of the study is: “To investigate the Need for Palliative care in Cerebrovascular Accident (stroke) patients at Ladysmith Regional Hospital”.
The objectives of the study were:
A. To identify the holistic care needs of stroke patients.
B. To describe the care provided to stroke patients.
C. To identify the gaps in the care requirements of stroke patients.
The study site was Ladysmith Regional Hospital, in UThukela District in Kwa-Zulu-Natal province, South Africa. This is a cross sectional study using mixed methods-both quantitative and qualitative-interviewing patients, and family members of patients who had suffered from a cerebrovascular accident.
From the results of quantitative data analysis by using SS-QOL tools, it was identified that the physical, emotional and social dysfunctions were the major concern of the participants after surviving from acute stroke. The result of qualitative data analysis, it was found that patients’ quality of life was poor, and they needed assistance from different health care team. It was observed in the study that the integration of palliative care with the rehabilitation programme can deliver a better service to the stroke patients with residual disabilities and morbidities.
Keywords: Palliative Care; Patients; Stroke Survivors; Quality of Life; Cerebrovascular Accident
Introduction
Stroke is one of the foremost causes of disability worldwide. Relatively good progress in medical science has been made for the prevention and therapeutic management of stroke but less has been done to identify the need of physical, social and spiritual well-being for stroke survivors.
This study addresses the gap between current practise the understanding of the necessity of palliative care for stroke-survival. This includes care for the last days in life as an important aspect of stroke management for patients with severe cerebrovascular accident. Research suggests that integration of palliative care and rehabilitation programmes provide good outcomes for stroke management in general [1].
Stroke mortality rates remain high in spite of modern therapeutic treatment and facilities for stroke management throughout the world [2]. There is a concern that palliative care management is not recognizing as specialist care in the developing world [3]. There are few hospices and few palliative care trained health workers available especially in rural areas of developing countries. Even in South Africa palliative care is not a recognize speciality in the health sector [4]. In some rural areas in South Africa, there is no hospice facility available and health care teams rely on home-based care only which is mainly delivered by relatives or paid caregivers.
As described by Clark, “stroke has been recognized for a long time as a disability for a patient (it features as “apoplexy” in the writings of Hippocrates)” [5]. Many patients need long-term treatment from multi-disciplinary health professional team. Cerebrovascular accident (CVA) is one of the most common conditions in adults admitted to the medical wards for their treatment and the most common cause of adult morbidity [6].
The prevalence of stroke related disability in South Africa is already higher than any other chronic illness. It was estimated that there are about 6 million people with hypertension, 7 million smokers and 3-4 million diabetic patients in South Africa are at risk of cerebrovascular accident [7]. South Africa has a substantial burden of HIV/AIDS and there is a need to face the burden of preventing the upcoming problem of the complications due to chronic diseases such as hypertension, diabetes mellitus and AIDS.
Rehabilitation (Rehab) and palliative care have emerged as two important parts of comprehensive medical care for patients with advanced disease such as who experienced CVA; the relationship between the two components are important and there is possible role of rehabilitation interventions in the care of patients with residual disabilities after surviving stroke [5]. Rehabilitation programmes comprises physiotherapy, speech therapy and occupational therapy and clinical experience confirms that the application of the fundamental principles of rehabilitation medicine improves the care for stroke survivors. Through rehab care, physical function can be maintained to lessen dependency on others and reduce the burden of care for the caregivers.
After survival from stroke, many patients suffer from residual disability and need rehabilitation to improve their physical function. In addition, those patients suffer from psychosocial or social problems, palliative care play an important role to improve their well-being. “Palliative care is a holistic approach and by involving the multidisciplinary team to enhance good quality of life, dignity in death as well as support for the family-including bereavement care”.
Furthermore, rehabilitation can help patients to regain their functional ability while they are admitted in hospital and as an outpatient. Stroke rehab also contributes to regain the capability to selfcare so that a stroke patient can live independently depending on the extent of their recovery. The rehabilitation process is best achieved by means of multi-disciplinary care by health care professionals who must have ample knowledge and understanding of the precise concerns facing by stroke survivors.
In South Africa, outpatient rehabilitation therapy is difficult to continue for a stroke patient. Sometimes, patients are not able to come for their follow-up at out-patients because of financial difficulties [4]. Consequently, wherever essential and available rehabilitation services are required, in-patient management would be the preferred choice. In-patient rehabilitation facilities in the public sector are available at most of the state hospitals, community health clinics and these are usually located in towns or in township.
There is a rising awareness of the value of palliative care management in patients who are affected by non-malignant diseases, including stroke [8]. Palliative Care Australia describes that stroke patients requiring “palliative care often present with complex and challenging needs in terms of physical care, as well as family” and caregiver concerns. Palliative care and rehabilitation together can deliver the adequate care to the stroke patient.
Palliative care and rehabilitation share common goals to improve the patient’s quality of life. Both disciplines have a multi-disciplinary model of care, which act to improve patients' levels of function and comfort.
By combination of both disciplines, an improved more comprehensive service can be delivered to a stroke survivor to improve the quality of life more effectively. The elements of rehabilitation that are used in managing stroke survivors include physiotherapy, speech, therapy and occupational therapy. Palliative care can also provide additional resources in ensuring management of physical symptoms, psycho-social support and spiritual care.
Palliative care for stroke survival can provide pain relief and can provide psychological as well as spiritual support. Those patients who develop depression or anxiety after surviving stroke can benefit from palliative care counselling. Social worker can also arrange financial support for stroke survivors. Palliative care includes the evaluation and management of bodily functions, social, emotional as well as spiritual needs. Families and caregivers also get support from palliative care personnel. This support is obtainable during the patient’s illness as well as providing bereavement care.
Rehabilitation is an aim orientated processes to facilitate regaining full function (as far as possible) in patients who have had a cerebrovascular accident and who suffer from combination of physical, intellectual and speech problems. In the presence of difficulty with speech or depressive symptoms, there is significant dependence on the family caregiver with challenges to the patient, caregiver and the rehab team.
Palliative care is defined by the WHO (World Health Organization) and it can be delivered over several months including at the end of life. The definition of “Palliative Care” by the World Health Organization in 2002 is:
“An approach that improves the quality of life of patients and their families facing the problems associated with life threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual”20
Methodology
This research work is a cross sectional study using mixed methodsboth quantitative and qualitative-interviewing patients, and family members of patients, who had suffered from a cerebrovascular accident.
The study site was Ladysmith Regional Hospital, which is situated in the UThukela District in Kwa-Zulu-Natal province, South Africa. Stroke patients admitted to medical wards, and who had attended the MOPD (Medical Outpatient Department) at Ladysmith Regional Hospital over 4-month period from the month of April to July 2013, and the members from family who were involved in their care at home.
Inclusion criteria
• Both male and female patients.
• Age: 40 years onwards.
• Those who survive from stroke incidents.
• Family members of these patients.
Exclusion Criteria
• Age over 80 years.
• Debilitated and very sick patients.
Quantitative study
Using the calculation for a single proportion and based on the study by Williams et al. 52% stroke patients had had problems on the SS-QOL [6] and it was expected that a similar proportion of patients would be found. This calculation has a precision of 10% with a sample size of 68, and a 90% confidence level.
The average number of admissions of stroke patients in medical wards per month is 10 to 12 and MOPD consultations amounted to approximately 8 to 10 per month; therefore in 4 months’ time approximately 70 to 75 patients will be eligible for the study. It is uncertain as to the total number of possible stroke patients so, consequently, the statistical calculation has been done using infinite population size.
Assumptions
Precision = 10.00 %
Prevalence = 52.00 %
Population size= infinite
90% Confidence Interval specified limits [42% --62%]
(These limits equal prevalence plus or minus precision)
Estimated sample size: n = 68
Qualitative study
Patients with speech capacity and family members of aphasic patients were included for purposive sampling. It was estimated that 10 patients out of total 72 participants would provide qualitative data and that recruitment would continue to data saturation.
Estimated sample size: n=10
Quantitative study
The data-collection tool was the SS-QOL Scale, which was used as questionnaire administered as a structured interview with stroke patients. This SS-QOL tool was developed in the USA. This is a consistent and effective tool for measuring self-reported quality of bodily health, set equal to amongst people with mild to moderate stroke.
The “Stroke Specific-Quality of Life (SS-QOL)” Scale is an effective tool for measuring and to evaluate the quality of life in patients after survival from an acute stroke.
The SS-QOL questionnaires were available in the website and there was no permission needed to use those questionnaires as tools to identify the patient’s quality of life after surviving stroke. These were used in few other countries as well and there was validity of questionnaires. It has been validated in Denmark [7], Turkey [8], and the Netherlands [9], although not in South Africa. From the previous research articles, it is revealed that the “Stroke Specific Quality of Life Scale (SS-QOL)” is an appropriate tool to check the quality of life after survival from stroke.
The questions were simple and related to the daily activities of life after surviving from stroke. Questionnaires were used for SS-QOL tool interpreted and translated into isiZulu language for the participants by the research assistant nurse. Even a set of questionnaires was in isiZulu language for isiZulu speaking participants specifically. All four-research assistant could speak and understand both isiZulu and English.
The research assistants were qualified professional nurse both from MOPD as well as from Medical ward. Research assistants were trained by PI how to do correct interpretation and not to deviate from the original questions. Simple terms were used to explain the questionnaires to the participants.
Answered questionnaires are options to score such as 5 ("no help needed/no trouble at all/strongly disagrees”), 4 ("a little help/a little trouble/moderately disagree”), 3 ("some help/some trouble/neither agree nor disagree”), 2 ("a lot of help/a lot of trouble/moderately agree”), and 1 ("total help/could not do it at all/strongly agree”). Stroke Specific Quality of Life scales offer score for each domain as well as a total score, with higher scores indicating restored functions.
Qualitative study
An interview guide was designed which includes a questionnaire and an information sheet to elicit the patient’s experience of stroke and care needs. The questionnaire was designed in discussion with the research supervisor and drawing on the literature regarding the experience of stroke and the researcher’s experiences in stroke care. There were six open ended questions in the interview guide questionnaires which reflect the daily life needs for a stroke patient.
The PI asked the questions in English and the research assistant used the isiZulu translations to ask the questions of isiZulu participants. The answers provided by the patients or relatives were noted by research assistant and at the same time, the research assistant interpreted all the answers in English to the PI for documentation. After finishing each patient interview, the PI and research assistant verified the answers of respective questionnaires together.
There were a few patients or family members who chose to withdraw from the interview process, this was accepted. Depending on the reason for stopping the interview, such as tiredness, an opportunity to complete the interview was offered at a later stage, especially if the participant had indicated that he or she would like to complete the interview later. This ensures that the data were collected from patients who were low functioning, as well as those who were high functioning after the cerebrovascular event. Attention was paid to non-verbal responses, as well as to verbal responses.
Confidentiality was strictly maintained at all times by all members of the research team. Study databases were password protected. Names were not used, and the questionnaires were marked with numbers. Master copy of the names and study number kept separately.
The quantitative data were analysed statistically. The questionnaires were comprised three
Sections: Section 1/A contained the Demographic details; section 1/B had the Medical and other history of the patient: and section 1/C comprised the Functional assessment scales, known as SS-QOL scales. Altogether 12 areas of questionnaires were subdivided into three groups according to the protocol for SS-QOL as follows:
Physical functions: Energy, Mobility, Self-care, Upper extremity function (UEF), Vision, Language, work.
Social function: Family role, Social role.
Emotional functions: Mood, Personality, and Thinking.
There are 12 variables in SS-QOL questionnaires therefore 3 factors were used to analysis the data and from three factors patients’ functional capability were revealed in result. Factor analysis is a statistical technique used to identify factors that statistically and encompasses generating one or more unobserved independent variables that correlate with the observed measures. Commonly used in survey research and other applications, factor analysis can be measured a data reduction technique because it reduces a large number of variables that often correspondence to a smaller number of factors.
Significance and reliability of data collected from SS-QOL scores were measured by using Cronbach's alpha. Before summated scores (calculated as either the sum or the average of responses to a set of items) can be analysed it has to be determined whether they are reliable [10]. The statistic used for this is Cronbach's alpha. The recommended interpretation intervals are: 0.60 to 0.69 acceptable; 0-70 to 0.79 good; 0.80+ excellent [11].
The qualitative data described from the in-depth interview were analysed through a process of thematic analysis. The following steps were used in the analysis of qualitative data: 1) immersion in the data – the transcripts were read and re-read to ensure 2) familiarisation with the data. During this period the PI held back from analysis and simply focused on getting to know the data; 3) identifying the topics or issues that seemed important to the participants and highlighting these in order to refer to them in collating the qualitative data; 4) coding the emerging themes and subthemes to organise the data.
Ethical approval of the research work was obtained from HREC (Human Research Ethics Committee) at UCT and reference number was 588/212. Thereafter, ethical approval was obtained from Provincial Heath Department (Ref: HRKM 089/13) and also from the facility where the study was conducted, respectively.
Results
Demographic results
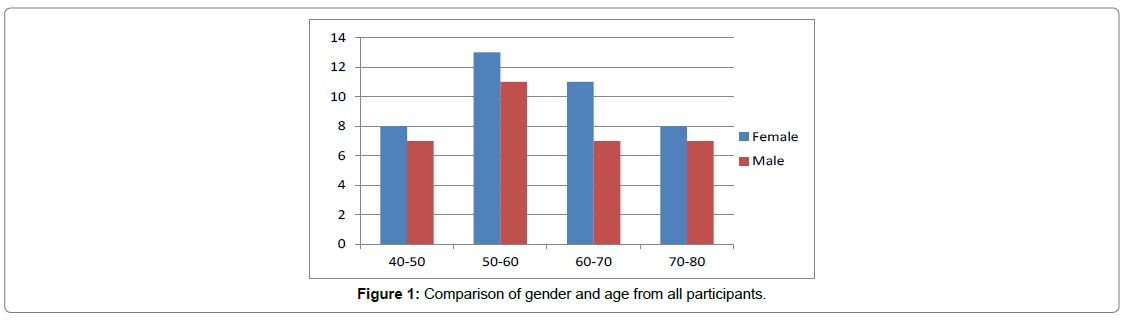
A total of 72 participants were interviewed of whom 31(43%) were male and 41(57%) female patients who had a stroke. The participants’ ages ranged from 40 to 80 years and majority were 50 to 60 years of age. Majority of the participants were married and had family size of 4-5 persons. It also reveals that the majority of participants were black African population. Participants were interviewed both at MOPD and in-patient ward (Table 1 and Figure 1)
| Variable | Category | Frequency n and % |
|
|---|---|---|---|
| Gender | Male | 32 | 44% |
| Female | 40 | 56% | |
| Marital status | Single | 3 | 4% |
| Married | 33 | 46% | |
| Widow/Widower | 26 | 36% | |
| Others | 10 | 14% | |
| Age | 40 – 50 | 15 | 21% |
| 50 – 60 | 24 | 33% | |
| 60 – 70 | 18 | 25% | |
| 70 – 80 | 15 | 21% | |
| Ethnicity | African | 65 | 91% |
| Indian | 4 | 5% | |
| Coloured | 2 | 3% | |
| White | 1 | 1% | |
| Family size | Single | 0 | 0% |
| 2-3 | 12 | 17% | |
| 4-5 | 24 | 33% | |
| 6-7 | 22 | 30% | |
| 7 and up | 14 | 20% | |
Table 1: Demographics of patients.
Figure 1 show that most of the participants were female and majority of patients were between 50 to 60 years of age.
Co-morbidity
The main co-morbidities reported among all participants, hypertension 58(81%) and diabetes 28(61%). Some patients also had both hypertension and diabetes.
Few participants were suffering from other chronic diseases as well, such as arthritis, epilepsy and HIV diseases. It was found that majority of the patients were suffering from hypertension before they had a CVA (Table 2).
| Variable | Category | Frequency n and % |
|
|---|---|---|---|
| Hypertension | Yes | 58 | 81% |
| No | 14 | 19% | |
| Diabetes | Yes | 28 | 39% |
| No | 44 | 61% | |
Table 2: Co-morbidities for participants.
Out of 72 patients 26 have been suffering from anxiety and 36 patients were suffering from depression (Table 3).
| Variable | Category | Frequency n and % |
|
|---|---|---|---|
| Anxiety | Yes | 26 | 36% |
| No | 36 | 44% | |
| Depression | Yes | 36 | 44% |
| No | 26 | 36% | |
Table 3: Psychological level of participants.
The majority 68 (94%) of the participants responded that they do have a spiritual belief. Few patients (8 out of 72 participants) had knowledge about palliative care. Most patients had also seen by other doctor before at MOPD during their previous consultations for poststroke management (Table 4).
| Variable | Category | Frequency n and % |
|
|---|---|---|---|
| Spiritual belief | Yes | 68 | 94% |
| No | 4 | 6% | |
| Knows about palliative care | Yes | 8 | 11% |
| No | 64 | 89% | |
| Seen by other doctor | Yes | 70 | 97% |
| No | 2 | 3% | |
Table 4: Other history.
Stroke specific quality of life scale (SS-QOL)
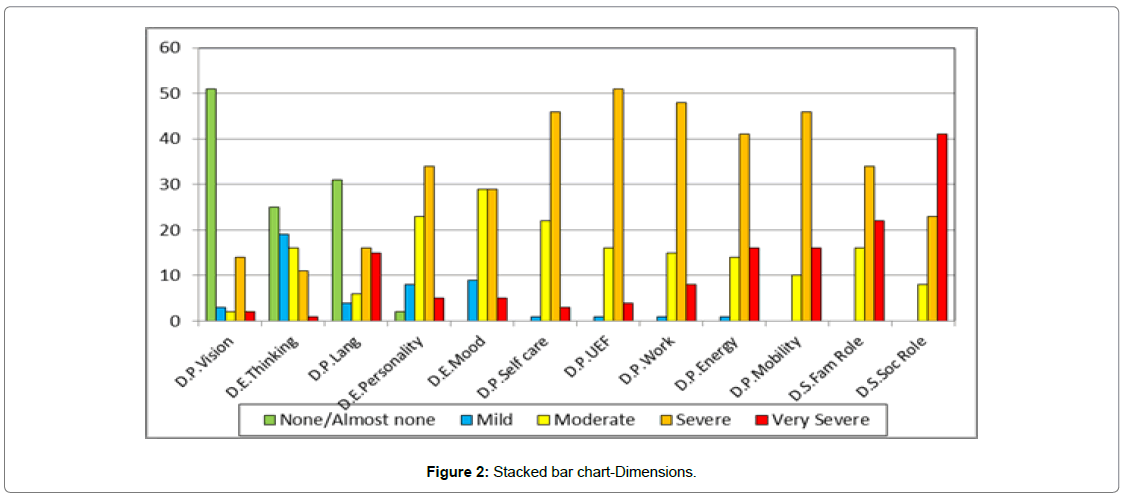
The results identified that which functional disabilities are mostly affected and influencing their daily activities in life. Participants were more concern about their physical functional disabilities and which influence patients’ daily activities in life. Participants were also psychologically distressed, with some participants expressing their concern with tears in the eyes.
From the findings of SS-QOL questionnaires’ it was also revealed that how severe the residual disabilities were after surviving stroke and how the patients were coping with those morbidities. All the findings are stipulated with statistical manner in tables and figures. Both descriptive statistics and dimensional statistic were used to explain their functional capability from mild to severe in nature. Because of their functional disabilities Social and Emotional factors both were affected.
Table 5, describes the mean and the range of functional disability of the participants.
| Mean | S.D. | Minimum | Quartile 1 | Median | Quartile 3 | Maximum | |
|---|---|---|---|---|---|---|---|
| D.S.Soc Role | 1.60 | 0.58 | 1.00 | 1.15 | 1.40 | 2.00 | 3.00 |
| D.S.Fam Role | 1.93 | 0.63 | 1.00 | 1.33 | 1.67 | 2.33 | 3.33 |
| D.P.Mobility | 1.95 | 0.52 | 1.00 | 1.67 | 2.00 | 2.00 | 3.00 |
| D.P.Energy | 2.01 | 0.67 | 1.00 | 1.67 | 2.00 | 2.33 | 4.00 |
| D.P.Work | 2.13 | 0.56 | 1.00 1.00 |
2.00 | 2.00 | 2.33 | 4.00 |
| D.P.UEF | 2.14 | 0.55 | 1.60 | 2.00 | 2.40 | 3.60 | |
| D.P.Self care | 2.24 | 0.59 | 1.00 | 1.80 | 2.00 | 2.60 | 3.80 |
| D.E.Mood | 2.56 | 0.78 | 1.00 | 2.00 | 2.60 | 3.20 | 4.40 |
| D.E.Personality | 2.62 | 0.89 | 1.00 | 2.00 | 2.33 | 3.33 | 4.67 |
| D.P.Lang | 3.26 | 1.68 | 1.00 | 1.80 | 3.00 | 5.00 | 5.00 |
| D.E.Thinking | 3.76 | 1.06 | 1.33 | 3.00 | 3.84 | 5.00 | 5.00 |
| D.P.Vision | 4.21 | 1.26 | 1.00 | 3.38 | 5.00 | 5.00 | 5.00 |
| F.Social | 1.77 | 0.53 | 1.00 | 1.27 | 1.70 | 2.15 | 3.00 |
| F.Physical | 2.56 | 0.55 | 1.56 | 2.18 | 2.60 | 2.94 | 3.89 |
| F.Emotional | 2.98 | 0.77 | 1.44 | 2.32 | 2.95 | 3.56 | 4.58 |
| F.Total | 2.44 | 0.55 | 1.34 | 1.97 | 2.42 | 2.83 | 3.73 |
Table 5: Descriptive statistics: D.P. Social role to F. Total (n = 72).
Table 6 shows the frequency distribution functional disability from very severe to none.
| Very/Severe | Moderate | Mild / None | ||||
|---|---|---|---|---|---|---|
| D.S.SocRole.C | 64 | 89% | 8 | 11% | 0 | 0% |
| D.P.Mobility.C | 62 | 86% | 10 | 14% | 0 | 0% |
| D.P.Energy.C | 57 | 79% | 14 | 19% | 1 | 1% |
| D.S.FamRole.C | 56 | 78% | 16 | 22% | 0 | 0% |
| D.P.Work.C | 56 | 78% | 15 | 21% | 1 | 1% |
| D.P.UEF.C | 55 | 76% | 16 | 22% | 1 | 1% |
| D.P.Selfcare.C | 49 | 68% | 22 | 31% | 1 | 1% |
| D.E.Personality.C | 39 | 54% | 23 | 32% | 10 | 14% |
| D.E.Mood.C | 34 | 47% | 29 | 40% | 9 | 13% |
| D.P.Lang.C | 31 | 43% | 6 | 8% | 35 | 49% |
| D.P.Vision.C | 16 | 22% | 2 | 3% | 54 | 75% |
| D.E.Thinking.C | 12 | 17% | 16 | 22% | 44 | 61% |
| F.Social.C | 65 | 90% | 7 | 10% | 0 | 0% |
| F.Physical.C | 32 | 44% | 37 | 51% | 3 | 4% |
| F.Emotional.C | 24 | 33% | 26 | 36% | 22 | 31% |
| F.Total.C | 42 | 58% | 27 | 38% | 3 | 4% |
Table 6: Frequency Distributions of functional disability: D.P. Social role C to F. Total. C(n = 72).
Figure 2 shows the severity of functional disability of participants for SS-QOL survey.
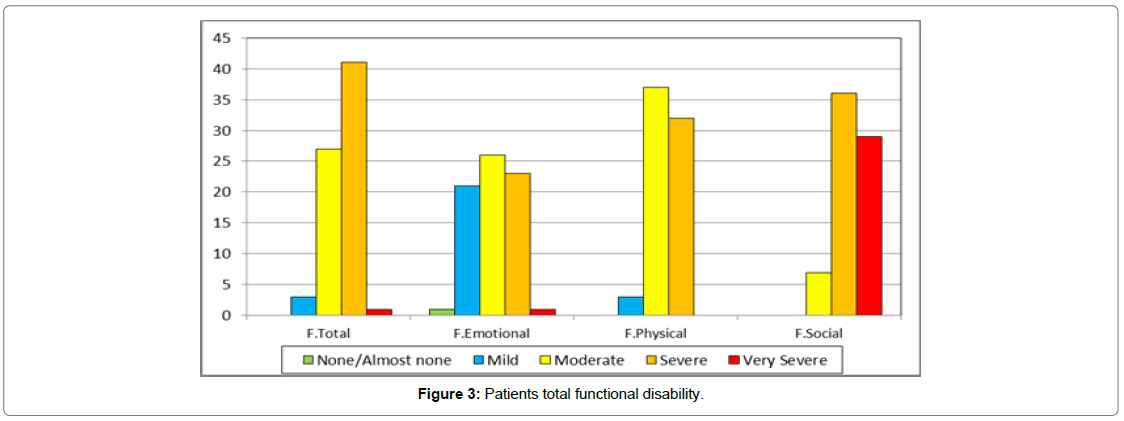
Figure 3 shows that 41% patients out of 72 participants had severe total functional disability that is physical, emotional and social. Thirty two percent of patients had severe physical functional disability and 33% patients had severe emotional functional disability after survival from stroke.
Table 7 shows the statistical analysis inferential ranking of the 12 dimensions of functional disabilities. The mean and standard deviation was calculated to determine the statistically significant of different dimensions.
| 95% Conf.Interval | ||||||
|---|---|---|---|---|---|---|
| Dimension | Rank | Significance Group |
Mean | SD | Low | High |
| D.S.Soc Role | 1 | 1 | 1.60 | 0.58 | 1.46 | 1.73 |
| D.S.Fam Role | 2 | 2 | 1.93 | 0.63 | 1.79 | 2.07 |
| D.P.Mobility | 2 | 2 | 1.95 | 0.52 | 1.83 | 2.07 |
| D.P.Energy | 2 | 2 | 2.01 | 0.67 | 1.86 | 2.16 |
| D.P.Work | 5 | 3 | 2.13 | 0.56 | 2.00 | 2.25 |
| D.P.UEF | 5 | 3 | 2.14 | 0.55 | 2.01 | 2.27 |
| D.P.Self care | 5 | 3 | 2.24 | 0.59 | 2.10 | 2.38 |
| D.E.Mood | 8 | 4 | 2.56 | 0.78 | 2.38 | 2.74 |
| D.E.Personality | 8 | 4 | 2.62 | 0.89 | 2.41 | 2.82 |
| D.P.Lang | 10 | 5 | 3.26 | 1.68 | 2.87 | 3.65 |
| D.E.Thinking | 11 | 6 | 3.76 | 1.06 | 3.52 | 4.01 |
| D.P.Vision | 12 | 7 | 4.21 | 1.26 | 3.92 | 4.50 |
Table 7: Inferential Ranking of Dimensions (n=72).
Table 8 reveals that the social functions are affected more than the emotional functions.
| 95% Conf.Interval | |||||||
|---|---|---|---|---|---|---|---|
| Factor | Rank | Significance Group |
Mean | SD | Low | High | |
| F.Social | 1 | 1 | 1.77 | 0.53 | 1.65 | 1.89 | |
| F.Physical | 2 | 2 | 2.56 | 0.55 | 2.43 | 2.69 | |
| F.Emotional | 3 | 3 | 2.98 | 0.77 | 2.80 | 3.16 | |
Table 8: Inferential Ranking of Factors (n=72).
(Table 9) Pearson Product Moment Correlations-Dimensions (n = 72)
| Factor | F. Emotional |
F. Physical |
F. Social |
|---|---|---|---|
| F.Emotional | - | .653 | .760 |
| F.Physical | .653 | - | .697 |
| F.Social | .760 | .697 | - |
Table 9: Pearson Product Moment Correlations -Between the factors (n = 72).
Correlations are Statistically significant at 0.05 level for n = 72 if |r| >= .232
Practically significant if |r| >= .300
In Table 10, sample t-Test was done for classification of different dimensions of functional disabilities. The dimensions from above table show most of them were statistically significant with a p-value of <. 0005. Sample size was adequate to statistically analysis of the data.
| Dimension | Mean | SD | H0 | t-value | p-value | Cohen's d | Category |
|---|---|---|---|---|---|---|---|
| D.S.Soc Role | 1.60 | 0.58 | ?? 2.51 | -13.36 | <.0005 | 1.57 | Severe |
| D.S.Fam Role | 1.93 | 0.63 | ?? 2.51 | -7.86 | <.0005 | 0.93 | Severe |
| D.P.Mobility | 1.95 | 0.52 | ?? 2.51 | -9.22 | <.0005 | 1.09 | Severe |
| D.P.Energy | 2.01 | 0.67 | ?? 2.51 | -6.37 | <.0005 | 0.75 | Severe |
| D.P.Work | 2.13 | 0.56 | ?? 2.51 | -5.83 | <.0005 | 0.69 | Severe |
| D.P.UEF | 2.14 | 0.55 | ?? 2.51 | -5.73 | <.0005 | 0.68 | Severe |
| D.P.Self care | 2.24 | 0.59 | ?? 2.51 | -3.88 | <.0005 | 0.46 | Severe |
| D.E.Mood | 2.56 | 0.78 | ?? 2.51 | 0.56 | .578 | n/a | Severe or Moderate |
| D.E.Personality | 2.62 | 0.89 | ?? 2.51 | 1.05 | .297 | n/a | Severe or Moderate |
| D.P.Lang | 3.26 | 1.68 | ?? 2.51 | 3.79 | <.0005 | 0.45 | Moderate |
| D.E.Thinking | 3.76 | 1.06 | ?? 3.49 | 2.20 | .031 | 0.26 | Mild/ Almost none |
| D.P.Vision | 4.21 | 1.26 | ?? 3.49 | 4.84 | <.0005 | 0.57 | Mild/ Almost none |
Table 10: One-sample t-Test (d.f.=71) Classification of Dimensions.
Table 11 shows that both social and emotional factors p-value <0.0005 are significantly compromised.
| Factor | Mean | SD | H0 | t-value | d.f. | p-value | Cohen's d | Category | |
|---|---|---|---|---|---|---|---|---|---|
| F.Social | 1.77 | 0.53 | ? | ≠ 2.51 | -11.95 | 71 | <.0005 | 1.41 | Severe |
| F.Physical | 2.56 | 0.55 | ? | ≠ 2.51 | 0.79 | 71 | .433 | n/a | Severe or Moderate |
| F.Emotional | 2.98 | 0.77 | ? | ≠ 2.51 | 5.23 | 71 | <.0005 | 0.62 | Moderate |
Table 11: One-sample t-Test (d.f. =71) Classification of Dimensions variables.
Table 12 shows Thematic analysis developed the following themes: The first theme dealt with the life changing effect of the stroke. The second theme dealt impact on quality of life after stroke. The third theme dealt with holistic care needs. The fourth theme dealt with loss of independence after surviving from a stroke. The fifth theme dealt with spiritual aspects of patient’s experience.
| THEME ONE | THEME TWO | THEME THREE | THEME FOUR | THEME FIVE |
|---|---|---|---|---|
| 1.Life changing | 2. Impact on quality of life | 3. Holistic care Needs |
4. Loss of independence | 5. Spiritual aspects |
| 1.1 Experiencing the effect of disability |
2.1Experiencing Bad quality of life |
3.1 Understanding a holistic care approach |
4.1 Isolation | 5.1 Spiritual Concerns |
| 1.2 Awareness about Post-stroke disability |
2.2 Hope for good quality life | 4.2 Loss of physical ability |
Table 12: Table of themes and sub-themes developed in data analysis.
Summary
The SS-QOL survey identified physical, emotional and social dysfunctions were the major concern of the participants. The severity of dysfunctions also stipulated in the SS-QOL survey.
This study detects the different levels of patients need and where to focus care after surviving from stroke to improve their quality of life. The questionnaires used had satisfactory core reliability with Cronbach's α coefficients greater than 0.60 for all scales and greater than 0.70 for five [12].
Measures of reliability were acceptable in this study; Cronbach's α correlation coefficient was more than 0.60 for all scales. The patients’ functional abilities are diminished, and this correlated with the limitations in performing activities for daily living.
The interview guide was designed to elicit the patient’s experience of stroke, post-stroke complications and the care needs. Ten patients (n=10) were recruited to participate in the qualitative study out of total seventy-two (n =72) participants for the whole study.
It was found that all ten participants could speak and understand English and they were interviewed during their follow-up consultation in presence of family members or the care givers at MOPD (Medical Outpatient Department).
Thematic analysis developed the following themes: The first theme dealt with the life changing effect of the stroke. The second theme dealt impact on quality of life after stroke. The third theme dealt with holistic care needs. The fourth theme dealt with loss of independence after surviving from a stroke. The fifth theme dealt with spiritual aspects of patient’s experience.
Discussion
Palliative care is ‘an approach that improves the quality of life of patients and their families who are facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification, proper assessment, and the treatment of pain and other problems: physical, psychosocial and spiritual.
This study highlights the impact on physical, emotional and social functions determined Stroke Specific Quality of Life of stroke survivors. It also considers their personal experiences described in individual interviews. The SS-QOL survey conducted in this study helps in understanding the psychological and social impact of the illness as well the physical needs and impact on activities of daily living. SS-QOL survey identified that physical, emotional and social dysfunctions were all major concerns of the participants.
Functional disabilities may lead to dependence on a wheelchair or sometimes the need for residential care with the help of rehabilitation team. A severe stroke can place a great burden on the coping abilities of care givers and family, as well as on the patients themselves.
Frustration is a common response to problems with all the disabilities after a stroke. Losing one’s independence is hard to accept. It is easy to imagine needing someone’s help to bath or to tie a shoelace: and trying to complete even simple tasks can be very frustrating and humiliating. Therefore, many patients required counselling by clinical psychologist.
In this research study, patients expressed their view about the benefit of counselling by clinical psychologist. During qualitative data collection interview, the majority of the participants expressed their concern about quality of life, psychological upset and spiritual thinking.
As described by Wee et al 33 effective palliative care can be delivered to stroke patients by a holistic approach to those who need it, including physical, psychological, social, and spiritual well-being. One of the significant findings from this study is that the knowledge of palliative care among patients, caregivers and family members was not adequate and it is necessary to empower potentials users with the knowledge about palliative care and stroke related complications for the patients. From literature review, it was found that the multidisciplinary approach of palliative care together with rehabilitation programme could improve the quality of life among stroke survivors with their residual disability.
Palliative care teams consist of professionals from different discipline such as physicians, palliative care specialists, physiotherapists, social workers, psychologists, counsellors including spiritual counsellors, dieticians and other allied health workers. This approach addresses the physical, emotional and social dysfunctions that were the major concern of the study participants as reflected in SS-QOL survey.
From SS-QOL survey significant prevalence of severe emotional disability was found. During the interview with patients those who reported about psychological problem, such as depression, anxiety and which was related with the lifestyle changes after survive from stroke.
Emotional distress was identified through the SS-QOL questionnaires asking about mood and personality. It is important to diagnose correctly and treat the patient with significant anxiety and depression, while adequately addressing other common concerns such as “demoralization, grief, social role, and family conflict”. This requires skilled assessment and psychological support by the clinical psychologist, social workers and non-clinical people such as a priest.
Stroke patients need to aware about their possible complications which can give them disability. The health care team should provide adequate support and to empower the patient and the family by providing information about stroke complications. The majority of the surviving patients live with the morbidities from post stroke complications; as well as weakness or paralysis, some patients may also experience trouble with speaking or understanding of speech, headaches, inappropriate behaviour, memory difficulties, visual problems and emotional problems.
The concept of spirituality is often misunderstood. Spirituality can be defined as “spiritual needs are the needs and expectations that human beings have to find meaning and purpose in life; such needs maybe specifically religious but even people who have no religious faith or who are not members of an organised religion have belief systems relating to meaning and purpose [13] Despite the clinical management of patients with stroke, there was a need to identify the holistic approach of palliative care to support patients and family members encompassing spiritual care.
After surviving acute stroke, some patients start thinking about or develop a fear of death, recognising they might have died from this event. During interview with the participants of this study, 20% patients spoke about the fear of death. Spiritual counselling can help stroke patients to explore the issues raised by these fears and to bring some comfort to the patients.
Because of existing functional disabilities only few participants in this research were attending their religious places for pray and this was a concern. Patients received the counselling from respective religious priest of different religions even at their home. A patient’s spiritual distress may be more than fears about dying. Existential concerns of meaning, purpose and connection, can all affect spiritual well-being and require spiritual counselling.
Palliative care can help with communication and may improve relationships at different levels, including those between patients and family members and between patients, family members and health care team. It is important to document, as appropriate, discussions with the patient, family and other care-providers to ensure a good flow of information within and between organisations involved in service delivery. The palliative care team must also be skilled in the care of stroke patients.
Palliative care can be initiated as early as possible during the illness and which can give comfort to the patient. However, many health professionals believe that the palliative care mainly focuses on the end of life. This view may be re-enforced by studies such as Bacquiere’s which focused on artificial feeding. There is lack of evidence about how the palliative care needs of acute stroke patients and family members should be addressed. This was also identified by Wee and Team.
A major limitation of the study is that not all participants could speak and express their views directly. Therefore, close family members were interviewed on behalf of many of the participants. Interviewing the relative or caregivers rather than directly interviewing patients may have led to some information being omitted in the collection of data.
Conclusion
It is suggested that to integration of the palliative care into the management plan together with other management plan for stroke patients, which may benefit the patient in the long term with a positive impact with their residual disabilities and co-morbidities. Integration of palliative care, rehabilitation and therapeutic management can deliver an improved service to stroke patients and their family members.
References
- Sydney M and Feldman DR (2012) Palliative Care and Rehabilitation for Stroke Survivors: Managing Symptoms and Burden, Maximizing Function. J Gen Intern Med 27: 760-762.
- Mortality and causes of death in South Africa, 2014: Findings from death notification / Statistics South Africa, Published by Statistics South Africa, Private Bag X44, Pretoria 0001
- Shahri M (2002) The Future of palliative care in the Islamic world. West J Med 176: 60-61.
- Connor MD (2007) A racial and urban-rural comparison of the nature of stroke in South Africa. Diss. Faculty of Health Sciences, University of the Witwatersrand.
- Sydney M, Dorianne R Feldman (2012). Palliative Care and Rehabilitation for Stroke Survivors: Managing Symptoms and Burden, Maximizing Function. J Gen Intern Med 27: 760-762.
- Williams LS, Weinberger M, Harris LE, Clark DO, Biller J, et al. (1999) Development of a stroke-specific quality of life scale. Stroke 30: 1362-1369.
- Muus I, Williams LS, Ringsberg KC (2007) Validation of the Stroke Specific Quality of Life Scale (SS-QOL): test of reliability and validity of the Danish version (SS-QOL-DK). Clinical Rehabilitation 21: 620-627.
- Hakverdioğlu Yönt G, Khorshid L (2012) Turkish version of the Stroke-Specific Quality of Life Scale. Int Nurs Rev 59: 274-280.
- Boosman H, Passier PE, Visser-Meily JM, Rinkel GJ, Post WM, et al. (2010) Validation of the Stroke Specific Quality of Life scale in patients with aneurysmal subarachnoid haemorrhage. Journal of Neurology, Neurosurgery & Psychiatry 81: 485-489.
- Ryman A and Bell E (2007) Business research methods. 2nd Edition. Oxford: Oxford University Press
- Nunnally J (1978) Psychometric theory. 2nd Edition McGraw-Hill, New York 85-94.
- Klein P (1993) The handbook of psychological testing. London: Routledge.
- Institute of Medicine (1999). Approaching death, improving care at the end of life. Washington DC: National Academy Press, 1999.
Citation: Hossain MJ (2020) To Investigate the Need for Palliative Care in Cerebrovascular Accident (Stroke) Patients at Ladysmith Regional Hospital. J Palliat Care Med 10: 368. DOI: 10.4172/2165-7386.1000368
Copyright: © 2020 Hossain MJ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2618
- [From(publication date): 0-2020 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1870
- PDF downloads: 748