To Evaluate Restoration of Functional Anatomy of Ankle Joint after Management of Ankle Fracture Dislocation
Received: 13-Dec-2018 / Accepted Date: 18-Feb-2019 / Published Date: 25-Feb-2019
Abstract
Introduction: Ankle injuries are common and account for more than five million emergency department consultations annually. Ankle fractures are an increasing problem due to the increasing aging population. The aim of the present study was to evaluate clinical and functional outcomes of Ankle fractures in the patients who have been managed operatively.
Materials and methods: A hospital based prospective observational study was performed for the duration of 2 years on 25 patients with ankle fracture dislocation to assess clinical and functional outcomes of ankle injuries in patients who have been managed operatively at one month, three months and six months interval.
Results: Ankle fractures were classified on the basis of Laughen Hansen classification, maximum number of cases i.e., 9 (36%), were classified as pronation external rotation injury followed by; 7 (28%) cases, which were pronation abduction injury. The preoperative radiological and functional assessment was done as per Kirstensen Criteria and scoring system respectively. There was improved functional outcome in the follow up period. There is a significant improvement in all parameters of Kirstensen criteria and scoring system confirmed by statistical analysis. After clinical and radiological evaluation, most effective and stable ankle was found after the follow-up period of six months.
Conclusion: Early treatment without delay, anatomical reduction and fracture fixation, stringent postoperative mobilization and rehabilitation should help improve outcome in an operated ankle fracture. Immediate open reduction and internal fixation in ankle fractures yield good results in terms of anatomical reduction, stability and postoperative functional return. Early return of ankle movements postoperative with proper rehabilitation improved functional outcome.
Keywords: Ankle fracture dislocation; Functional anatomy of ankle joint; Musculoskeletal injuries
Introduction
Among musculoskeletal injuries, the incidence of ankle sprains is between 15% and 20% of sports injuries [1,2]. The ankle is supported laterally by the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL), whilst the medial aspect is supported by the deltoid ligament [3]. Ankle sprains can be either acute sprains, which can be further classified into three grades depending on the severity of the injury, or chronic instability [4].
Ankle injuries are common and account for more than five million emergency department consultations annually [5]. Interestingly, 85% of these ankle injuries are ankle sprains and the remaining 15% are ankle fractures [6]. Overall ankle fractures constitute 9% of fractures and are the most common injuries involving articular surface of a weight bearing joint [7,8]. There has been a three-fold rise in incidence in the older females over the past three decades because of an aging population [7,9]. There has also been a surge in the number of open ankle fractures amongst the elderly following low energy trauma such as a falls from standing height. Ankle fractures are an increasing problem due to the increasing aging population [7].
A high proportion of patients with ankle fractures are at risk of developing post traumatic ankle osteoarthritis in addition to other complications. This can significantly impact the quality of life and lead to increased mortality in the most severe cases [10]. Therefore, the primary intervention is to restore the normal anatomy. Currently operative treatment dominates the literature on ankle fractures; however, conservative treatment of stable ankle fractures is gaining more interest. Studies comparing operative and conservative treatment are dated and contradicted in their conclusions. The decision whether to operate or not is often based upon the Arbeitsgemeinschaft Osteosynthesefragen (AO) modifications of Weber’s classification and the Lauge-Hansen classification [11], but is also highly dependent upon the surgeon’s individual judgment on displacement. There is consensus that undisplaced Weber A-type fractures rarely require operative treatment, and that Weber C-type or grossly displaced fractures are unstable by nature and therefore require surgery. The grey area of treatment lies mainly with the minimally displaced Weber Btype ankle fractures.
Hence the present study was done at our tertiary care centre to assess the functional outcome of ankle joint after malleolar fracture and to evaluate clinical and functional outcomes of Ankle Injuries in the patients who have been managed operatively.
Materials and Methods
A hospital based cross sectional study to assess clinical and functional outcomes of ankle injuries in patients who have been managed conservatively and operatively in Department of Orthopaedics, Acharya Vinobha Bhave rural hospital, DMIMS (DU) from August 2016 to July 2018. Initially, 29 patients with ankle fractures, attending the orthopaedic outpatients, inpatients and casualty of department of orthopaedics were shortlisted for our study, diagnosed on history, clinical examination and X-ray findings. After applying inclusion criteria (Age group: 18-75 years, all cases of fracture dislocation and fracture of ankle, patients who are willing to give consent, Patient managed conservatively as well as with surgical intervention) and exclusion criteria (Pathological fracture, neglected ankle injuries, patient not willing to give written consent, compound fractures of ankle), 25 patients were found suitable and were enrolled for our study. The enrolled patients were examined in the casualty and in the out-patient department of orthopaedics. History was recorded and a thorough clinical examination was done. Patients were stabilized haemodynamically and were administered adequate analgesia. A below knee splint age either with a malleable splint or a plaster of paris posterior slab was applied.
X-rays were done with mortise, anteroposterior and lateral radiograms of injuries around ankle. The fractures classification was according to the Lauge-Hansen and Weber’s classifications and graded as per Kirstensen criteria. Treatment was based upon patient characteristics (co-morbidities, level of activity), fracture characteristics (number of fractured malleoli, displacement, and stability) and on surgeons preference concerning the threshold of displacement of the distal fibular fragment and shortening of the fibula, which was usually at 2 mm. Most fractures were initially treated in a non-weight bearing plaster backslap and evaluated at the outpatient department within 1 week.
Following the radiological evaluation, patients were counselled regarding the need for operative treatment and were investigated with routine investigations for the surgical procedure. Patients with comorbid medical illnesses were treated appropriately with the help of general physicians. Evaluation by anesthesiologists was done. Consent for the surgical procedure was obtained. Conservative treatment concerned immobilization in a below-knee plaster cast usually for 6 weeks. During the application of the cast, a manual reduction was tried by reversing the trauma-mechanism using the Lauge-Hansen classification. Immediately after application of the cast at the Emergency Department, radiographs were taken to confirm that reduction was adequate. All patients received preoperative antibiotic prophylaxis (i.e., third generation cephalosporin). After surgery, the ankle was usually immobilized with a below-knee plaster cast for 6 weeks. Weight bearing in the cast was usually allowed after 2 weeks.
In both treatment groups, radiographs were taken at 2 and 6 weeks to ensure that there was no loss of reduction and to monitor fracture healing. During immobilization in plaster cast, all patients were treated with low-molecular weight heparin, once daily, as thrombosis prophylaxis. After cast removal, patients commenced weight bearing under supervision of a physiotherapist. Radiographic data were obtained from the radiographs taken immediately after the injury and immediately after operative repair. Dislocation was measured as lateral displacement of the fibula at the level of the tibial plafond and the distal anteromedial border of the fibula (Mueller nose), and at the Medial Clear Space (MCS) at 10 mm below the tibial plafond. Fracture classification according to Lauge-Hansen was performed by two observers (ES, TS). In case of differences consensus was met after discussion. MCS and dislocation at the Mueller nose as measure of lateral displacement of the fibula were calculated on the same radiographs. The question related to alignment and range of motion was completed by a physician based upon patient files and radiographs; the other questions were completed by the patient. A Visual Analog Scale was used to measure overall satisfaction of patients with outcome (range 0-10). Results were assessed for clinical, functional and radiological outcome. Association among the study groups is assessed with the help of Fisher test, student‘t’ test and Chi- Square test. ‘p’ value less than 0.05 is taken as significant.
Results
Majority of the patients (32%) were in the age group of 21-30 years followed by 24% in the age group of 41-50 years. The mean age of the patients was 43.24 ± 15.79 years. There was male preponderance (76%). 19 (76%) patients were farmer while 6 (24%) patients were housewives by occupation. The mode of injury in 13 (52%) patients was slip & fall while 12 (48%) patients were involved in Road Traffic Accident (RTA). 12 (48%) patients had fractured their left ankle while 13 (52%) patients had fractured their right ankle. Majority of the patients (40%) were admitted in the q within 3-4 hours of injury. The mean time from injury to hospital admission of patients was 3.64 ± 1.52 hours. Most of the patients (72%) were operated at >24 hours after being admitted in the hospital. On the basis of Lauge Hansen classification, 9 (36%) cases were classified as pronation external rotation, 7 (28%) were pronation abduction, 6 (24%) were supination external rotation and 3 (12%) were supination adduction injury (Table 1).
| Age in years | |
| 21-30 | 8 (32%) |
| 31-40 | 3 (12%) |
| 41-50 | 6 (24%) |
| 51-60 | 5 (20%) |
| 61-70 | 1 (4%) |
| 71-75 | 2 (8%) |
| Mean ± SD | 43.24 ± 15.79 |
| Sex | |
| Male | 19 (76%) |
| Female | 6 (24%) |
| Occupation | |
| Farmer | 19 (76%) |
| Housewife | 6 (24%) |
| Mode of injury | |
| Slip and fall | 13 (52%) |
| RTA | 12 (48%) |
| Laterality | |
| Right | 12 (48%) |
| Left | 13 (52%) |
| Time from injury to hospital admission | |
| 1-2 hours | 8 (32%) |
| 3-4 hours | 10 (40%) |
| 5-6 hours | 7 (28%) |
| Type of injury Lauge Hansen Classification | |
| Pronation abduction | 7 (28%) |
| Pronation external rotation | 9 (36%) |
| Supination adduction | 3 (12%) |
| Supination external rotation | 6 (24%) |
Table 1: Baseline characteristics.
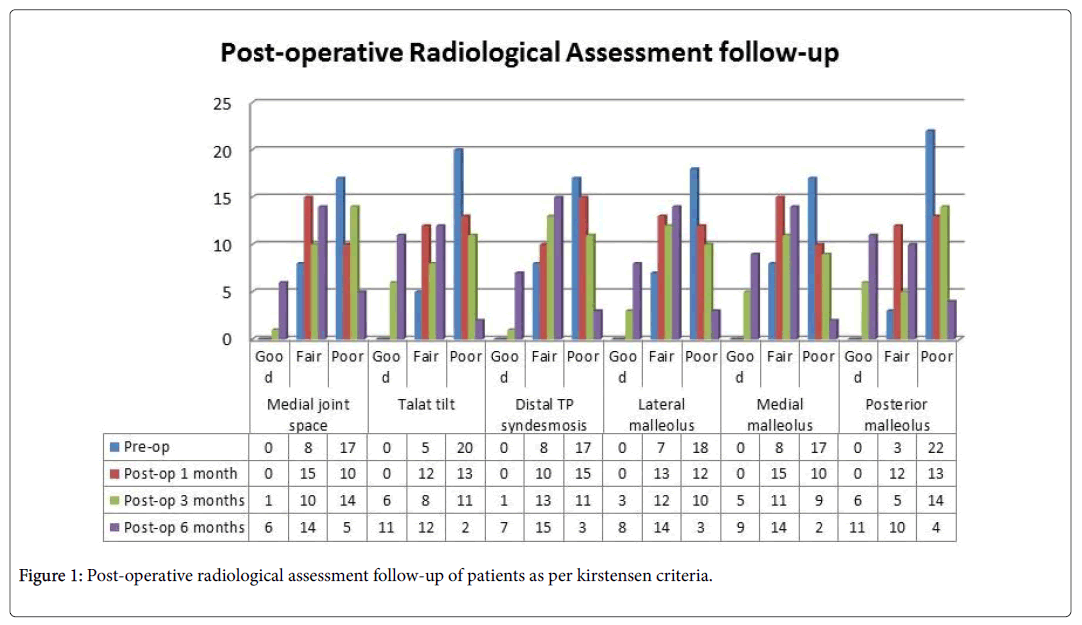
The pre-operative radiological assessment as per Kirstensen Criteria showed fair and poor results in Medial joint space, Distal TP syndesmosis and Medial malleolus criteria for 8 (32%) and 17 (68%) patients respectively while 5 (20%) and 20 (80%) patients showed fair and poor results respectively in Talar tilt criteria. Fair and poor results were observed in 7 (28%) and 18 (72%) patients for Lateral malleolus criteria and in 3 (12%) and 22 (88%) patients for Posterior malleolus criteria. The pre-operative functional assessment as per Scoring System showed 9 (36%) and 16 (64%) patients had pain with weight bearing and pain after any activity and at rest respectively. All patients showed instability during daily activity and were unable to walk, climb stairs and run.In the Range of Motion, all patients showed difference >15° in dorsiflexion. 3 (12%) showed no difference from normal side while 22 (88%) patients showed difference <20° in plantar flexion. There was difference in pronation/supination ROM. All patients also reported antalgic limp. Only 1 (4%) patient out of 25 (100%) underwent conservative management rest 24 (96%) patients were treated surgically. It was observed that at post-operative 6 months there was significant improvement in all parameters of Kirstensen Criteria (Medial joint space, Talar tilt, Distal TP syndesmosis, Lateral malleolus, Medial malleolus and Posterior malleolus) as per Chi- Square test (p<0.05) (Table 2 and Figure 1).
| Kirstensen Criteria | Pre-op | Post-op 1 month | Post-op 3 months | Post-op 6 months | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |||
| Medial joint space | Good | 0 | - | 0 | - | 1 | 4% | 6 | 24% | <0.05 |
| Fair | 8 | 32% | 15 | 60% | 10 | 40% | 14 | 56% | ||
| Poor | 17 | 68% | 10 | 40% | 14 | 56% | 5 | 20% | ||
| Talar tilt | Good | 0 | - | 0 | - | 6 | 24% | 11 | 44% | <0.05 |
| Fair | 5 | 20% | 12 | 48% | 8 | 32% | 12 | 48% | ||
| Poor | 20 | 80% | 13 | 52% | 11 | 44% | 2 | 8% | ||
| Distal TP syndesmosis | Good | 0 | - | 0 | - | 1 | 4% | 7 | 28% | <0.05 |
| Fair | 8 | 32% | 10 | 40% | 13 | 52% | 15 | 60% | ||
| Poor | 17 | 68% | 15 | 60% | 11 | 44% | 3 | 12% | ||
| Lateral malleolus | Good | 0 | - | 0 | - | 3 | 12% | 8 | 32% | <0.05 |
| Fair | 7 | 28% | 13 | 52% | 12 | 48% | 14 | 56% | ||
| Poor | 18 | 72% | 12 | 48% | 10 | 40% | 3 | 12% | ||
| Medial malleolus | Good | 0 | - | 0 | - | 5 | 20% | 9 | 36% | <0.05 |
| Fair | 8 | 32% | 15 | 60% | 11 | 44% | 14 | 56% | ||
| Poor | 17 | 68% | 10 | 40% | 9 | 36% | 2 | 8% | ||
| Posterior malleolus | Good | 0 | - | 0 | - | 6 | 24% | 11 | 44% | <0.05 |
| Fair | 3 | 12% | 12 | 48% | 5 | 20% | 10 | 40% | ||
| Poor | 22 | 88% | 13 | 52% | 14 | 56% | 4 | 16% | ||
Table 2: Post-operative radiological assessment follow-up of patients as per Kirstensen criteria.
It was observed that at post-operative 6 months there was significant improvement in all parameters of Scoring System (Pain, Articular Function, Range of Motion and Gait Analysis) as per Chi- Square test (p<0.05) (Tables 3-6 and Figure 2). It was observed that 1 (4%) patient each had wound dehiscence and stiffness of ankle joint at post-operative 1 month period while 3 (12%) had stiffness of ankle joint at post-operative 3 months period. At post-operative 6 months period, 1 (4%) patient each had stiffness of ankle joint and arthritis. There was no significant difference in complications during the postoperative follow-up period as per Chi-Square test (p>0.05).
| Scoring System–Pain | Pre-op | Post-op 1 month | Post-op 3 months | Post-op 6 months | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| No pain | 0 | - | 0 | - | 0 | - | 15 | 60% | <0.05 |
| Mild pain with heavy activity | 0 | - | 0 | - | 9 | 36% | 10 | 40% | |
| Mild pain with daily activity | 0 | - | 0 | - | 9 | 36% | 0 | - | |
| Pain with weight bearing | 9 | 36% | 24 | 96% | 7 | 28% | 0 | - | |
| Pain after any activity and at rest | 16 | 64% | 1 | 4% | 0 | - | 0 | - | |
Table 3: Post-operative functional assessment follow-up of patients as per scoring system-Pain.
| Scoring system-Articular Function | Pre-op | Post-op 1 month | Post-op 3 months | Post-op 6 months | p-value | |||||
| N | % | N | % | N | % | N | % | |||
| Stability of Ankle joint | No Instability | 0 | - | 0 | - | 0 | - | 25 | 100% | <0.05 |
| Instability during heavy activity (running, sports) | 0 | - | 24 | 96% | 25 | 100% | 0 | - | ||
| Instability during daily activity | 25 | 100% | 1 | 4% | 0 | - | 0 | - | ||
| Ability to Walk | Ability to walk unlimited distances without pain or limp | 0 | - | 0 | - | 0 | - | 19 | 76% | <0.05 |
| Ability to walk unlimited distances; mild pain or limp after long distances | 0 | - | 0 | - | 0 | - | 6 | 24% | ||
| Able to walk; moderate pain or limp after short distances | 0 | - | 0 | - | 17 | 68% | 0 | - | ||
| Able to walk short distances only; 1 cane | 0 | - | 17 | 68% | 8 | 32% | 0 | - | ||
| Unable to walk | 25 | 100% | 8 | 32% | 0 | - | 0 | - | ||
| Ability on Stair Climbing | Able to climb stairs | 0 | - | 0 | - | 0 | - | 17 | 68% | <0.05 |
| Able to climb stairs with some difficulty | 0 | - | 0 | - | 17 | 68% | 8 | 32% | ||
| Required aid of banister | 0 | - | 16 | 64% | 8 | 32% | 0 | - | ||
| Unable to climb stairs | 25 | 100% | 9 | 36% | 0 | - | 0 | - | ||
| Ability to run | Able to run; mild pain after long distances | 0 | - | 0 | - | 0 | - | 14 | 56% | <0.05 |
| Able to run; moderate pain after short distances | 0 | - | 0 | - | 15 | 60% | 11 | 44% | ||
| Unable to run | 25 | 100% | 25 | 100% | 10 | 40% | 0 | - | ||
Table 4: Post-operative functional assessment follow-up of patients as per scoring system–Articular function.
| Scoring System - Range of Motion | Pre-op | Post-op 1 month | Post-op 3 months | Post-op 6 months | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |||
| Dorsiflexion | No difference from normal side | 0 | - | 0 | - | 25 | 100% | 25 | 100% | <0.05 |
| Difference <15° | 0 | - | 25 | 100% | 0 | - | 0 | - | ||
| Difference >15° | 25 | 100% | 0 | - | 0 | - | 0 | - | ||
| Plantar Flexion | No difference from normal side | 3 | 12% | 0 | - | 25 | 100% | 25 | 100% | <0.05 |
| Difference <20° | 22 | 88% | 25 | 100% | 0 | - | 0 | - | ||
| Pronation / Supination | No difference from normal side | 0 | - | 25 | 100% | 25 | 100% | 25 | 100% | <0.05 |
| Difference | 25 | 100% | 0 | - | 0 | - | 0 | - | ||
Table 5: Post-operative functional assessment follow-up of patients as per scoring system–Range of motion.
| Scoring System - Gait Analysis | Pre-op | Post-op 1 month | Post-op 3 months | Post-op 6 months | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Normal gait | 0 | - | 16 | 64% | 25 | 100% | 25 | 100% | <0.05 |
| External rotation gait | 0 | - | 3 | 12% | 0 | - | 0 | - | |
| Antalgic limp | 25 | 100% | 6 | 24% | 0 | - | 0 | - | |
Table 6: Post-operative functional assessment follow-up of patients as per scoring system–Gait analysis.
Discussion
A hospital based prospective cross sectional study was done with 25 patients to assess clinical and functional outcomes of ankle injuries in patients who have been managed conservatively and operatively. The annual incidence of ankle fractures (AF) is approximately 122-184/100,000 person years (1:800) [12-14]. The two age groups most commonly affected are young active men with high‑energy trauma, and older women with low energy trauma [9,12-14]. The earliest description of AF was given by Pott [15] and Dupuytren [16]. Although many classification systems are proposed, two most widely used ones are the Weber [17] and the Lauge‑Hansen classification [18-20]. The former is based on the relationship of the level of the distal fibular fracture with the syndesmosis, in an attempt to quantify stability. The latter is based on a cadaveric study involving two aspects the position of the foot at the time of injury and the direction of the applied deforming force.
There has been gradual evolution in management of ankle fractures due to improved analysis of biomechanics, improvement in fixation techniques and analysis of results of recent studies. The goal of treatment is to provide fracture union with painless full motion of ankle and with anatomical restoration of the injured ankle. Closed method of treatment is often inadequate in restoring the anatomy and biomechanics of ankle in unstable malleolar ankle fractures. Conversely, open reduction with internal fixation is an excellent method for restoration of normal anatomy of the joint. Several studies indicated that, internal fixation of displaced malleolar fractures of ankle provides good results [21-24].
In the present study, majority of the patients (32%) were in the age group of 21-30 years followed by 24% in the age group of 41-50 years. The mean age of the patients was 43.24 ± 15.79 years. There was male preponderance (76%) in the study while female patients constituted 24% of the study group. 19 (76%) patients were farmer while 6 (24%) patients were housewives. This is similar to the studies of Jhatoth [25], Van der Weert, et al. [26], Tantigate, et al. [27] and Mohan Kumar, et al. [28].
Jhatoth [25] study assessing different surgical methods of stabilization and comparing the results of non-operative treatment of bimalleolar fracture of ankle joint found 214 cases of ankle joints of either sex with age ranging from 11-50 years. There was male preponderance (77.77%) in the study. The average age for the whole group was 30.10 years. Tantigate, et al. [27] in a retrospective chart review comparing short-term functional outcome after open reduction and internal fixation (ORIF) in ankle fractures with and without dislocation found mean age was 48.5 ± 17.56 years (range, 19-85) and majority of the patients 61.3% (38 patients) were female.
In our study, the mode of injury in 13 (52%) patients was slip & fall while 12 (48%) patients were involved in Road Traffic Accident (RTA). This is comparable to the studies of Mohan Kumar, et al. [28] and Jhatoth [25]. Mohan Kumar, et al. [28] in a prospective randomized study reported most common mode of injury was road traffic accidents.
It was observed in our study that 12 (48%) patients had fractured their left ankle while 13 (52%) patients had fractured their right ankle. This is concordant to the studies of Jhatoth [25], Van der Weert, et al. [26], Tantigate, et al. [27] and Mohan Kumar, et al. [28].
Jhatoth [25] study assessing different surgical methods of stabilization and comparing the results of non-operative treatment of bimalleolar fracture of ankle joint reported left side to be more often injured than right side. On the other hand, Van der Weert et al. [26] observed right side was involved in 51% of the fractures.
It was observed in the present study that majority of the patients (40%) were admitted in the hospital within 3-4 hours of injury. The mean time from injury to hospital admission of patients was 3.64 ±1.52 hours. Majority of the patients (72%) were operated at >24 hours after being admitted in the hospital.
Tantigate, et al. [27] in a retrospective chart review comparing short-term functional outcome after open reduction and internal fixation (ORIF) in ankle fractures with and without dislocation reported mean time from injury to surgery was 9 hours (5-13 hours) in non-dislocation and in Fracture-dislocation it was 5 hours (3-8 hours).
In our study, on the basis of Lauge Hansen classification, 9 (36%) cases were classified as pronation external rotation, 7 (28%) were pronation abduction, 6 (24%) were supination external rotation and 3 (12%) were supination adduction. Mohan Kumar, et al. [28] reported most common injury pattern seen was supination external rotation followed by supination adduction and pronation external rotation.
In the present study, the pre-operative radiological assessment as per Kirstensen Criteria showed fair and poor results in Medial joint space, Distal TP syndesmosis and Medial malleolus criteria for 8 (32%) and 17 (68%) patients respectively while 5 (20%) and 20 (80%) patients showed fair and poor results respectively in Talar tilt criteria. Fair and poor results were observed in 7 (28%) and 18 (72%) patients for Lateral malleolus criteria and in 3 (12%) and 22 (88%) patients for Posterior malleolus criteria.
Van der Weert, et al. [26] retrospective cohort study determining the clinical and functional outcome after AO-Weber B-type ankle fractures in operatively and conservatively treated patients and which factors influenced outcome reported in conservatively treated group, most fractures involved were type AO-B1.1 (61%) and LH-SER2 (81.7%). In 92.7%, there was only unimalleolar involvement. The median fibular dislocation was 0 mm. In the operatively treated group most injuries were type AO-B1.2 (35%) and LH-SER4 (50.5%) fractures. Fibular displacement was frequently a reason for ORIF (median 1.39 mm).
In our study, the pre-operative functional assessment as per Scoring System showed 9 (36%) and 16 (64%) patients had pain with weight bearing and pain after any activity and at rest respectively. All patients showed instability during daily activity and were unable to walk, climb stairs and run. In the Range of Motion, all patients showed difference >15° in dorsiflexion. 3 (12%) showed no difference from normal side while 22 (88%) patients showed difference <20° in plantar flexion. There was difference in pronation/supination ROM. All patients also reported antalgic limp. These findings were consistent with the studies of Tantigate, et al. [27] and Jhatoth [25].
Tantigate, et al. [27] in a retrospective chart review comparing short-term functional outcome after open reduction and internal fixation (ORIF) in ankle fractures with and without dislocation reported comparison of FAOS score between surgery <14 and ≥ 14 Days as symptoms of pain, reduced activities of daily living and sports and unsatisfactory quality of life. Jhatoth [25] study assessing different surgical methods of stabilization and comparing the results of nonoperative treatment of bimalleolar fracture of ankle joint reported out of 27 cases n=22 (81.4%) cases were displaced fractures and failure to reduce cases were n=5 (18.5%) and non-union cases were NIL. Open reduction and internal fixation was done in n=22 (81.4%) displaced fractures and dislocated ankles. Open reduction for Non-Union was NIL.
It was observed in our study that at post-operative 6 months there was significant improvement in all parameters of Kirstensen Criteria (Medial joint space, Talar tilt, Distal TP syndesmosis, Latera malleolus, Medial malleolus and Posterior malleolus) as per Chi- Square test (p<0.05). At post-operative 6 months there was significant improvement in all parameters of Scoring System (Pain, Articular Function, Range of Motion and Gait Analysis) as per Chi-Square test (p<0.05). Mohan Kumar et al. [28] in a prospective randomized study assessed the clinical outcome of ankle fractures with regards to the demographic variables and the quality of reduction of the fractures reported mean Olreud and Molander Ankle score at 3rd month post op was 47.5 ± 17.9 and at 6th month post op was 81.7 ± 16.2. There was a statistically significant improvement in the scores from 3rd month to 6th month post-op (p-value 0.000). Relationship between age of the patient and the olreud and molander ankle score, it was noted that there is a significant association between age and the OMA score with advanced age being associated with a lower OMA score both at 3rd month and 6th month post-op (p-value 0.002).
Conclusion
Early treatment, anatomical reduction and fracture fixation, stringent postoperative mobilization and rehabilitation should help improve outcome in an operated ankle fracture. The overall functional outcome was better with early return of ankle movements post operatively with proper rehabilitation.
References
- Ekstrand J, Gillquist J (1983) Soccer injuries and their mechanisms: A prospective study. Med Sci Sports Exerc 15: 267-270.
- Junge A, Engebretsen L, Mountjoy ML, Alonso JM, Renström PA, et al. (2009) Sports injuries during the summer olympic games 2008. Am J Sports Med 37: 2165-2172.
- Bozkurt M, Doral MN (2006) Anatomic factors and biomechanics in ankle instability. Foot Ankle Clin 11: 451-463.
- Clanton TO, Coughlin MJ, Mann RA (1999) Athletic injuries to the soft tissues of the foot and ankle. Surgery of the Foot and Ankle 7th edn pp: 1101-1106.
- Buddecke DE, Mandracchia VJ, Pendarvis J (1998) Is this just a sprained ankle? Hosp Med 34: 46-52.
- Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: A review. Injury 37: 691-697.
- Phillips WA, Schwartz HS, Keller CS (1985) A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg Am 67: 67-78.
- Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M (2002) Increasing number and incidence of low-trauma ankle fractures in elderly people. Finnish statistics during 1970-2000 and projections for the future. Bone 31: 430-433.
- Mehta SS, Rees K, Cutler L, Mangwani J (2014) Understanding risks and complications in the management of ankle fractures. Indian J Orthop 48: 445-452.
- Tunturi T, Kemppainen K, Patiala H, Suokas M, Tamminen O, et al. (1983) Importance of anatomical reduction for subjective recovery after ankle fracture. Acta Orthop Scand 54: 641–647.
- Donken CC, Al‑Khateeb H, Verhofstad MH, van Laarhoven CJ (2012) Surgical versus conservative interventions for treating ankle fractures in adults. Cochrane Database Syst Rev 8: CD008470.
- Court Brown CM, McBirnie J, Wilson G (1998) Adult ankle fractures: An increasing problem? Acta Orthop Scand 69: 43-47.
- Salai M, Dudkiewicz I, Novikov I Amit Y, Chechick A (2000) The epidemic of ankle fractures in the elderly: Is surgical treatment warranted? Arch Orthop Trauma Surg 120: 511-513.
- https://www.worldcat.org/title/some-few-general-remarks-on-fractures-and-dislocations-by-percivall-pott/oclc/833814293#borrow
- Dupuytren G (1939) Of fractures of the lower extremity of the fibula, and luxations of the foot. Med Classics 4: 151-172.
- https://www.worldcat.org/title/verletzungen-des-oberen-sprunggelenkes/oclc/555462056
- Lauge-Hansen N (1950) Fractures of the ankle: Combined experimental-surgical and experimental roentgenologic investigations. Arch Surg 60: 957-985.
- Lauge-hansen N (1954) Fractures of the ankle genetic roentgenologic diagnosis of fractures of the ankle. Am J Roentgenol Radium Ther Nucl Med 71: 456-471.
- Lauge N (1948) Fractures of the ankle: Analytic historic survey as the basis of new experimental, roentgenologic and clinical investigations. Arch Surg 56: 259-317.
- Beris AE, Kabbani KT, Xenakis TA, Mitsionis G, Soucacos PK, et al. (1997) Surgical treatment of malleolar fractures: A review of 144 patients. Clin Orthop Related Research 341: 90-98.
- Burwell HN, Charnley AD (1965) The treatment of displaced fractures of ankle by rigid internal fixation and early joint movement. J Bone Joint Surg 47: 634-660.
- De Souza LJ, Gustilo RB, Meyer TJ (1985) Results of operative treatment of displaced external rotation-abduction fractures of ankle. J Bone Joint Surg 67: 1066-1074.
- Cimino W, Ichtertz D, Silabaugh P (1991) Early mobilization of ankle fracture after open reduction and internal fixation. Clin Orthop 267: 152-156.
- Jhatoth DS (2017) Evaluation and surgical management of bimalleolar fractures of ankle joint. Int J Ortho Sci 3: 620-623.
- Van der Weert EMV, Van Lieshout EMM, De Vries MR, Van der Elst M, Schepers T (2012) Determinants of outcome in operatively and non-operatively treated Weber-B ankle fractures. Arch Orthop Trauma Surg 132: 257–263.
- Tantigate D, Ho G, Kirschenbaum J Bäcker HC, Asherman B, et al. (2014) Functional outcomes after fracture-dislocation of the ankle. Columbia Orthop 1-11.
- Mohan Kumar CR, Almedia VDR, Thomas Babu A, D'Souza T (2017) To assess the clinical outcome of ankle fractures with regards to the demographic variables and the quality of reduction of the fractures. Int J Orthop Sci 3: 445-448
Citation: Agrawal S, Pisulkar GL (2019) To Evaluate Restoration of Functional Anatomy of Ankle Joint after Management of Malleolar Fractures. Clin Res Foot Ankle 7:285.
Copyright: © 2019 Agrawal S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2566
- [From(publication date): 0-2019 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 1803
- PDF downloads: 763