To Correlate, Rbc Indices in Classifying Spectrum of Aneamia in Adult Females in Tertiory Care Hospital
Received: 17-Feb-2020 / Accepted Date: 02-Mar-2020 / Published Date: 09-Mar-2020 DOI: 10.4172/2161-0681.1000373
Abstract
Aims: To correlate Age, Type, Rbc Indices in deciding the severity of anaemia in adult females in tertiory care hospital.
Settings and designs: A hospital based cross sectional study was done at our tertiary care centre in central clinical laboratory of Dr. D.Y. PATIL Medical College & Hospital and Research Centre, Pimpri, Pune among 1000 adult females to evaluate prevalence of spectrum of anaemia. Considering a confidence level of 95% and confidence interval of 3.1 the number of patients in our study to achieve statistical significance is 999. The Survey System ignores the population size when it is "large" or unknown. Population size is only likely to be a factor when you work with a relatively small and known group of people (e.g., the members of an association). Hence a sample size of 1000 was considered adequate for our study.
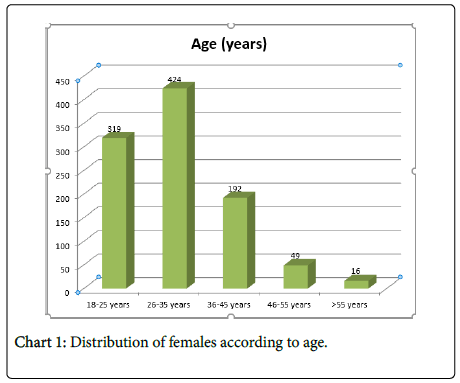
Results: Majority of the females (42.44%) were in the age group of 26-35 years followed by 31.9% in the age group of 18-25 years, 19.2% in the age group of 36-45 years, 4.9% in the age group of 46-55 years and 1.6% in the age group of 56-65 years. 410 (41%) females had mild anemia while 440 (44%) and 150 (15%) females had moderate and severe anemia.
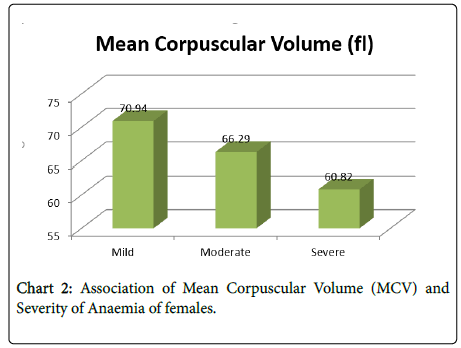
The Mean Corpuscular Volume (MCV) of females with mild anemia was 70.94 ± 1.35 fl while the mean MCV of females with moderate and severe anemia was 66.29 ± 2.43 fl and 60.82 ± 1.77 fl respectively. There was significant decrease in mean corpuscular volume (MCV) with increase in severity of anemia as per ANOVA test (p<0.05).
The mean corpuscular hemoglobin (MCH) of females with mild anemia was 25.74 ± 2.38 pg while the mean MCH of females with moderate and severe anemia was 21.16 ± 2.07 pg and 17.84 ± 1.96 pg respectively. There was significant decrease in mean corpuscular hemoglobin (MCH) with increase in severity of anemia as per ANOVA test (p<0.05).
The mean corpuscular hemoglobin concentration (MCHC) of females with mild anemia was 32.76 ± 3.14 while the mean MCHC of females with moderate and severe anemia was 29.55 ± 2.83 and 26.91 ± 2.34 respectively. There was significant decrease in mean corpuscular hemoglobin concentration (MCHC) with increase in severity of anemia as per ANOVA test (p<0.05).
The mean red cell distribution width (RDW) of females with mild anemia was 17.72 ± 0.87% while the mean RDW of females with moderate and severe anemia was 18.26 ± 1.18% and 20.05 ± 1.37% respectively. There was increase in red cell distribution width (RDW) with increase in severity of anemia but the increase was statistically not significant as per ANOVA test (p>0.05).
Conclusion: Iron deficiency anemia is increasing in females, especially in reproductive age group of developing countries. The hematological parameters can aid in early recognition of type and cause of anemia and thereby improve the outcome. The study confirms that iron deficiency anemia is the most common cause of anemia in pregnancy and is a major health problem in developing and developed countries. Early detection, treatment and prevention of anemia can improve maternal as well as child outcome.
Keywords: Anaemia; Mcv; Mch; Mchc; Rdw
Introduction
Anemia is a major public health problem. Anemia is not a diagnosis but is an objective for presence of disease. It is especially prevalent in women of reproductive age, particularly during pregnancy. Poor nutritional status during pregnancy is associated with inadequate weight gain, anemia, retarded fetal growth low birth weight, still births, preterm delivery, intrauterine growth retardation, morbidity and mortality rates [1].
Anemia is defined as a “Decrease in whole body red cell mass, a definition that precludes relative decreases in red blood cell count, hemoglobin, or hematocrit, which occur when the plasma volume”. In practice, the measurement of red cell mass is not easy, and anemia is usually diagnosed based on a reduction in the hematocrit (the ratio of packed red cells to total blood volume) and the hemoglobin concentration of the blood to levels that are below the normal range [2].
A classification of anemia is based on underlying mechanism and according to alterations in red cell morphology. Morphologic characteristics provide etiology clues such as red cell size (normocytic, microcytic, macrocytic), degree of hemoglobinization, reflected in the color of red cells (normochromic or hypochromic), and shape. In general, microcytic hypochromic anemias are caused by disorders of hemoglobin synthesis (most often iron deficiency) while macrocytic anemias often from abnormalities that impair the maturation of erythroid precursors in the bone marrow. Normochromic, normocytic anemias have diverse etiologies; in some of these anemias, specific abnormalities of red cell shape provide an important clue about cause.
Materials and Methods
A hospital based cross sectional study was done at our tertiary care center in central clinical laboratory of Dr. D.Y. PATIL Medical College & Hospital and Research Centre, Pimpri, Pune among 1000 adult females to evaluate prevalence of spectrum of anemia.
Study design
A hospital based prospective observational cross-sectional study.
Study duration
Data analysis was based on records of the investigations obtained in Central Clinical Laboratory of Dr. D.Y Patil Hospital.
Hospital resources and laboratory data was utilized, and no patient/ hospital funding was required. An institutional ethics committee clearance (IECC) was obtained before the start of the study.
A waiver in patient’s informed and written consent was done.
Study population
1000 consecutive cases of adult females to evaluate prevalence of spectrum of anemia who fulfilled the inclusion criteria.
Sample size
1000 patients.
Considering a confidence level of 95% and confidence interval of 3.1 the number of patients in our study to achieve statistical significance is 999. This was calculated by Survey System (http:// www.surveysystem.com/sscalc.htm#one). The Survey System ignores the population size when it is "large" or unknown. Population size is only likely to be a factor when you work with a relatively small and known group of people (e.g., the members of an association). Hence a sample size of 1000 was considered adequate for our study.
Criteria of anemias
Adult Non-Pregnant Females HB Less Than 12 gm%. Adult Pregnant Females HB Less Than 11 gm%.
Inclusion criteria
Adult females age 18 years or above, anemia in non-pregnant and pregnant adolescent girls.
Exclusion criteria
Adult females who are on treatment of anemia. Females less than 18 yrs.
Institutional ethical committee (iec) clearance was obtained before start of study. The study was carried at Patil medical college, Pune for a period of 2.5 yrs 2017-2019. Total of 1000 cases of adult females that came for ccl were studied. The sample for test was collected in EDTA tube. The slides were prepared, and smears made. The sample was evaluated in the cell counter for various indices. Reports of cell counter and pbs were assessed and types of anemia were observed and noted. Bone marrow findings of all the patients were unavailable.
Results
A hospital based cross sectional study was done among 1000 adult females to evaluate prevalence of spectrum of anemia.
Distribution of females according to age
Majority of the females (42.44%) were in the age group of 26-35 years followed by 31.9% in the age group of 18-25 years, 19.2% in the age group of 36-45 years, 4.9% in the age group of 46-55 years and 1.6% in the age group of 56-65 year (Table 1) (Chart 1).
| Age (years) | N | % |
|---|---|---|
| 18-25 years | 319 | 31.90% |
| 26-35 years | 424 | 42.40% |
| 36-45 years | 192 | 19.20% |
| 46-55 years | 49 | 4.90% |
| >55 years | 16 | 1.60% |
| Total | 1000 | 100% |
Table 1: Distribution of females according to age.
Association of Mean Corpuscular Volume (Mcv) and severity of anemia of females
The mean corpuscular volume (MCV) of females with mild anemia was 70.94 ± 1.35 fl while the mean MCV of females with moderate and severe anemia was 66.29 ± 2.43 fl and 60.82 ± 1.77 fl respectively. There was significant decrease in mean corpuscular volume (MCV) with increase in severity of anemia as per ANOVA test (p<0.05) (Table 2) (Chart 2).
| Severity of Anaemia | Mean Corpuscular Volume (fl) | p Value | |
|---|---|---|---|
| Mean | SD | ||
| Mild | 70.94 | 1.35 | <0.05 |
| Moderate | 66.29 | 2.43 | |
| Severe | 60.82 | 1.77 | |
Table 2: Association of Mean Corpuscular Volume (MCV) and Severity of Anemia of females.
Association of Mean Corpuscular Hemoglobin (Mch) and severity of anaemia of females
The mean corpuscular haemoglobin (MCH) of females with mild anaemia was 25.74 ± 2.38 pg while the mean MCH of females with moderate and severe anaemia was 21.16 ± 2.07 pg and 17.84 ± 1.96 pg respectively. There was significant decrease in mean corpuscular hemoglobin (MCH) with increase in severity of anemia as per ANOVA test (p<0.05).
Association of Mean Corpuscular Hemoglobin Concentration (Mchc) and severity of anemia of females
The mean corpuscular hemoglobin concentration (MCHC) of females with mild anemia was 32.76 ± 3.14 while the mean MCHC of females with moderate and severe anemia was 29.55 ± 2.83 and 26.91 ± 2.34 respectively. There was significant decrease in mean corpuscular hemoglobin concentration (MCHC) with increase in severity of anemia as per ANOVA test (p<0.05).
Association of Red Cell Distribution Width (Rdw) and Severity of Anaemia of Females
The mean red cell distribution width (RDW) of females with mild anemia was 17.72 ± 0.87% while the mean RDW of females with moderate and severe anemia was 18.26 ± 1.18% and 20.05 ± 1.37% respectively. There was increase in red cell distribution width (RDW) with increase in severity of anemia but the increase was statistically not significant as per ANOVA test (p>0.05).
Discussion
A hospital based cross sectional study was done among 1000 adult females to evaluate prevalence of spectrum of anemia. In the present study, majority of the females (42.44%) were in the age group of 26-35 years followed by 31.9% in the age group of 18-25 years, 19.2% in the age group of 36-45 years, 4.9% in the age group of 46-55 years and 1.6% in the age group of 56-65 years [3,4].
The assessing the spectrum and characteristics of admitted patients for anemia found mean age of the patients was 46.92 years (minimum 13 years and maximum 85 years, SD ± 16.80 years) [5].
The study determining the prevalence of anemia among antenatal mothers with a view to develop and evaluate a planned health education program on prevention and management of anemia in pregnancy found (68%) were in the age group of 21-25 years, followed by 21 % in the age group of 26-30 years and 10% of the in the age group of below 20 years [3].
The study assessing the hematological parameters in anemic pregnant women found 70 patients (58.33%) to be anemic i.e. they had hemoglobin concentration less than 11 g%. 42% of these were primi gravida. Out of 70 cases of pregnant anemic women, 7 were less than 20 years of age, 30 women had age between 20-25 and women in age group 26-30 were 33. 58.33% were found to be anemic with hemoglobin less than 11 gm% [4].
In our study, 410 (41%) females had mild anemia while 440 (44%) and 150 (15%) females had moderate and severe anemia [4-8].
The assessing the spectrum and characteristics of admitted patients for anemia found mean hemoglobin was 6.9 gm% (minimum 2.2, maximum 11.9 and SD 2.34). 47% patients had severe anemia [4].
It was observed in the present study that the mean corpuscular volume (MCV) of females with mild anemia was 70.94 ± 1.35 fl while the mean MCV of females with moderate and severe anemia was 66.29 ± 2.43fl and 60.82 ± 1.77 fl respectively. There was significant decrease in Mean Corpuscular Volume (MCV) with increase in severity of anemia as per ANOVA test (p<0.05).
The evaluating the occurrence of Iron deficiency anemia among females of reproductive age group reported mean corpuscular volume (MCV) of females with mild anemia was 62.1-79.9 ± 71.9 while the mean MCV of females with moderate and severe anemia was 58-79.8 ± 68.2 and 53-66 ± 60.3 respectively [7].
The study assessing the prevalence of anemia in adult patients reported high MCV was seen in one case which on peripheral smear showed macrocytosis. Whereas low MCV was seen in 16 patients with microcytic hypochromic, 3 patients had normocytic normochromic, remaining 5 patients showed dimorphic picture [7-10].
It was observed in our study that the mean corpuscular hemoglobin (MCH) of females with mild anemia was 25.74 ± 2.38 pg while the mean MCH of females with moderate and severe anaemia was 21.16 ± 2.07 pg and 17.84 ± 1.96 pg respectively. There was significant decrease in mean corpuscular haemoglobin (MCH) with increase in severity of anaemia as per ANOVA test (p<0.05) [4].
The study assessing the prevalence of anemia in adult patients observed Normal MCH in predominantly normocytic normochromic anemia and few microcytic anemias. High MCH was seen in macrocytic and one case of normocytic normochromic anemia. Low MCH was seen in microcytic hypochromic and some in normocytic normochromic and dimorphic anemia [6].
The study assessing the haematological parameters in anemic pregnant women reported mean value of MCV was 77.11 fl, mean MCH was 26.62 pg, mean MCHC was 32.92 [4].
In our study, the mean corpuscular haemoglobin concentration (MCHC) of females with mild anaemia was 32.76 ± 3.14 while the mean MCHC of females with moderate and severe anaemia was 29.55 ± 2.83 and 26.91 ± 2.34 respectively. There was significant decrease in mean corpuscular haemoglobin concentration (MCHC) with increase in severity of anaemia as per ANOVA test (p<0.05).
The study assessing the prevalence of anemia in adult patients reported normal MCHC in 36 patients. Out of these patients, on peripheral smear examination 31 patients had normocytic normochromic anemia, 3 showed microcytic anemias, 2 showed dimorphic picture. Low MCHC is seen in 15 patients with microcytic anemia, 1 macrocytic and remaining 6 in dimorphic anemia [6].
In the present study, the mean red cell distribution width (RDW) of females with mild anaemia was 17.72 ± 0.87% while the mean RDW of females with moderate and severe anaemia was 18.26 ± 1.18% and 20.05 ± 1.37% respectively. There was increase in red cell distribution width (RDW) with increase in severity of anaemia but the increase was statistically not significant as per ANOVA test (p>0.05) [4,7].
The evaluating the occurrence of Iron deficiency anemia among females of reproductive age group observed mean corpuscular volume (MCV) was much lower in all cases of patients suffering from mild to severe anaemia. Values of Red cell distribution width (RDW) were found to be in variance than the normal values [7].
The study assessing the haematological parameters in anemic pregnant women reported mean red cell distribution width coefficient of variation (RDW CV) was 15.70+1.92% [4].
In the present study, there was significant difference in red cell indices [Packed Cell Volume (PCV), Mean Corpuscular Volume (MCV), Mean Corpuscular Haemoglobin (MCH), Mean Corpuscular Haemoglobin Concentration (MCHC), Red Cell Distribution Width (RDW)] as per ANOVA test (p<0.05).
The study assessing the prevalence of anemia in adult patients reported mean values of Hb, HCT, MCV, MCH, MCHC and RDW correlated with the morphological features on peripheral in all the groups except dimorphic anemias. In few cases MCV and MCH did not correlate with the morphological picture found in the peripheral smear examination. Two cases of microcytic hypochromic anemia had normal MCV and MCH and three cases normocytic normochromic anemia had borderline values of MCV and MCH, which on peripheral smear examination show insignificant number of microcytes [6].
Conclusion
The study assessing the prevalence of anemia in adult patients reported mean values of Hb, HCT, MCV, MCH, MCHC and RDW correlated with the morphological features on peripheral in all the groups except dimorphic anemias. In few cases MCV and MCH did not correlate with the morphological picture found in the peripheral smear examination. Two cases of microcytic hypochromic anemia had normal MCV and MCH and three cases normocytic normochromic anemia had borderline values of MCV and MCH, which on peripheral smear examination show insignificant number of microcytes.
References
- Kansal B, Guleria K, Aggarwal (2004) Effect of maternal nutritional supplementation on foetal growth parameters and doppler flow velocity in growth restricted foetuses. Ind J Nutr Dietet 41: 198-204.
- Kumar V, Abbas AK, Fausto N, Robins, Cotran (2010) Pathologic Basis of Disease (8th edn) Ch. 14. Philadelphia, PA: Saunders Elsevier; p.644
- Uptmore, Connell B (2001) Comparison of the Sysmex XE-2100 to the Abbott cell Dyn 4000, Automated Hematology Analyzer. Sysmex J Int 11: 22-26.
- Rajesh KM, Ramesh BP, Ilahi M (2013) Iron deficiency anemia: An experience with one hundred consecutive hospitalized patients. Med Sci 2.
- Maj Sivapriya S, Lt Col Laxmipriya Parida (2017) A study to assess the knowledge and practices regarding prevention of anaemia among antenatal women attending a tertiary level hospital in Pune. Int J Sci Res NET 4: 1210-1214.
- Sharma AK, Bansal A, Sharma S (2017) Study on diagnostic parameters in women of reproductive age Group suffering from iron deficiency anaemia. Indian J Sci Res 7: 83-89.
- Mowla Ahmed HA, Aljaber NY, Aziz Ahmed EA (2018) The Effect of Developing and Implementing Health Education and Nutrition Training Program on Self-Management Practices among Patients with Iron Deficiency Anemia, Alexandria Main University Hospital, Egypt. Int J Inn Res Med Sci 3.
- Sharma AK, Bansal A, Sharma S (2017) Study on diagnostic parameters in women of reproductive age Group suffering from iron deficiency anaemia. Indian J Sci Res 7: 83-89.
- Chen, Lin-Lin (2018) Effects of processing adjuvants on traditional Chinese herbs. J Food Drug Anal 26: 96-114.
- Alkindi, Salam (2020) Predictors of impending acute chest syndrome in patients with sickle cell anaemia. Scientific Reports 10: 1-6.
Citation: Kour S, Pradhan M, Gore CR (2020) To Correlate, Rbc Indices in Classifying Spectrum of Aneamia in Adult Females in Tertiory Care Hospital. J Clin Exp Pathol 10: 373. DOI: 10.4172/2161-0681.1000373
Copyright: © 2020 Kour S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1862
- [From(publication date): 0-2020 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 1271
- PDF downloads: 591