Thyroiditis heralding Hereditary Hemochromatosis: an unusual initial manifestation and review of literature
Received: 13-Jun-2020 / Accepted Date: 22-Aug-2020 / Published Date: 29-Aug-2020 DOI: 10.4172/2161-069X.1000628
Abstract
The systemic involvement that often manifests in genetic hemochromatosis is well known. Although evidence of iron deposition in endocrine glands has been widely reported, the probable functional changes due to disrupted and altered thyroid in the course of hemochromatosis have not been attributed and defined yet. The deposition of iron in the thyroid gland may directly affect it and the functionality of thyroid may be possibly disrupted by the accumulation of iron in the pituitary gland. The prevalence and the pathogenetic links of primary thyroid disease in patients with genetic hemochromatosis are still largely unknown and need to be studied. Hereby, we describe one patient affected by genetic hemochromatosis who developed Hashimoto's thyroiditis. Considering the possible links occurring among iron overload, thyroid gland damage and thyroid dysfunction, we hypothesize that hemochromatosis could have been an important factor for the development of primary thyroid disease in this patient. We conclude that systematic studies in large and heterogeneous populations should be conducted in order to assess the risk of development of primary thyroid disorders in course of genetic hemochromatosis and, more generally, chronic iron overload conditions. It is our opinion thyroid function should be periodically checked in all patients with chronic iron overload conditions.
Keywords: Breastfeeding, bottle feeding, breast milk substitute, obesity, overweight
Introduction
Hereditary hemochromatosis (HH) is an inherited disease of iron metabolism described by uncontrolled iron retention and absorption that prompts parenchymal iron excess and as a result, leads to widespread organ damage [1]. A defect in the hemochromatosis gene (HFE) is the most common form of HH, also known as the classic form or type 1 (type 1 HH), where the principal mutation is represented by a substitution of tyrosine for cysteine at position 282 of the HFE gene (C282Y) [2]. The most widely recognized endocrinopathies associated with and complications of HH are diabetes mellitus and hypogonadotropic hypogonadism [3]. Excessive iron deposition in the pancreatic Islet cells of Langerhan and in the pituitary gonadotrophs cause defective secretion of the hormones and thus the clinically significant presentation. However an unusual finding and one that is not very well documented and apparent is the significant amounts of iron deposition found on autopsy in the thyroid gland of patients suffering from HH [4]. It is yet to be made concrete whether or not, the extensive iron deposition in the thyroid causes dysfunction of the gland, however there have been a number of case reports documenting that patients with HH were found to be suffering from hypothyroidism, [5,6] the results of studies carried out on a larger scale have been conflicting.
In this case report, we aim to present a patient who had history of thyroiditis of unknown etiology prior to presentation. She then presented with signs of Cirrhosis secondary to hereditary hemochromatosis and a possible association between iron deposition related thyroiditis and hemochromatosis was concluded. Previous case reports have described development of thyroiditis of varying etiology after diagnosis of Hemochromatosis but our case was unique due to thyroiditis presenting prior to other signs of Hemochromatosis.
Case Presentation
30-year-old female, with history significant for hypothyroidism diagnosed 2 years prior, presented with progressively worsening abdominal distension for 1 week. She felt very bloated, had decreased appetite, no abdominal pain but occasional nausea with non-bloody vomiting. She initially thought she had constipation and tried taking laxatives without relief. She was passing gas but denies fevers, chills or diarrhea. She drank alcohol few days per week and did smoke cigarettes. She denied any NSAID, Tylenol, illicit drug, or any herbal supplement use. She was a housewife, mother of 2 healthy children, and denied any occupational exposure. No prior personal or family history of thyroid, kidney, liver, or autoimmune disease.
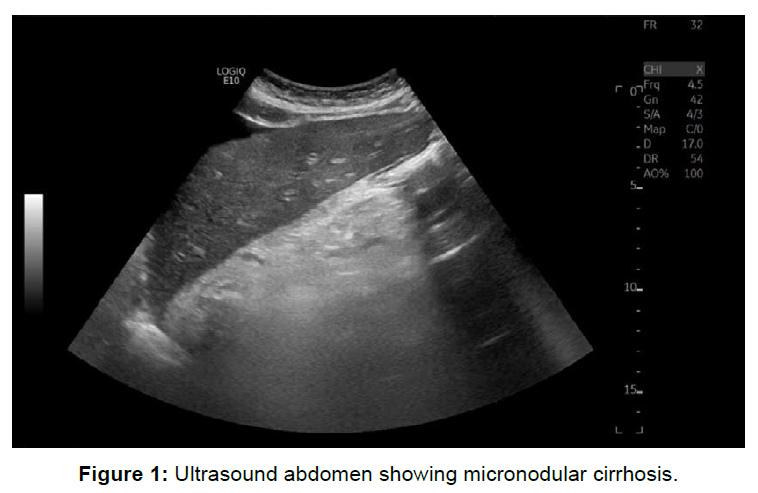
Physical examination revealed afebrile, hemodynamically stable but scleral icterus bilaterally. Abdominal exam revealed distended abdomen with shifting dullness and tympanic percussion note. No abdominal tenderness and normal bowel sounds appreciated. Lab work revealed elevated liver function test, notably elevated AST/ALT ratio, elevated total bilirubin, elevated alkaline phosphatase, elevated INR, low albumin 2.3 alongside severe electrolyte derangement (hyponatremia, hyperkalemia). Abdominal ultrasound showed morphologic features suggestive of cirrhosis with sequelae of portal hypertension including ascites and diminished and retrograde flow in the main portal vein (Figure 1). Abdominal CT of the abdomen revealed significant ascites. Patient underwent paracentesis which revealed transudative effusion.
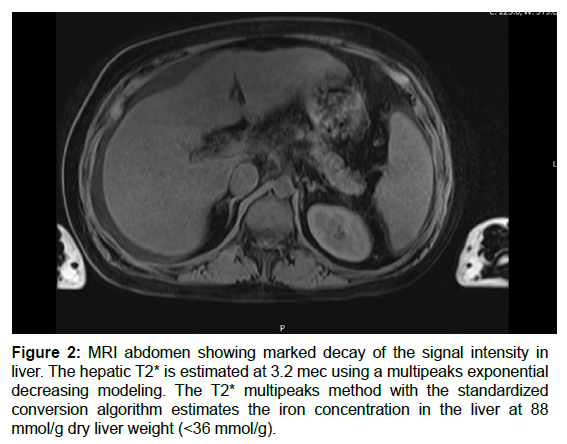
Investigation for cause of cirrhosis revealed ethanol, acetaminophen, aspirin levels were unremarkable. Anti-ANA, antismooth muscles, antimitochondrial antibodies, ANCA were also negative. Ceruloplasmin and alpha 1 antitrypsin levels were normal. Elevated iron and ferritin 1200 with iron saturation 61%. HFE gene testing revealed homozygous for HFE C282Y gene mutation, consistent with Hereditary Hemochromatosis. MRI abdomen revealed Liver iron overload with slight hepatic steatosis but no splenic iron overload (Figure 2).
Figure 2: MRI abdomen showing marked decay of the signal intensity in liver. The hepatic T2* is estimated at 3.2 mec using a multipeaks exponential decreasing modeling. The T2* multipeaks method with the standardized conversion algorithm estimates the iron concentration in the liver at 88 mmol/g dry liver weight (<36 mmol/g).
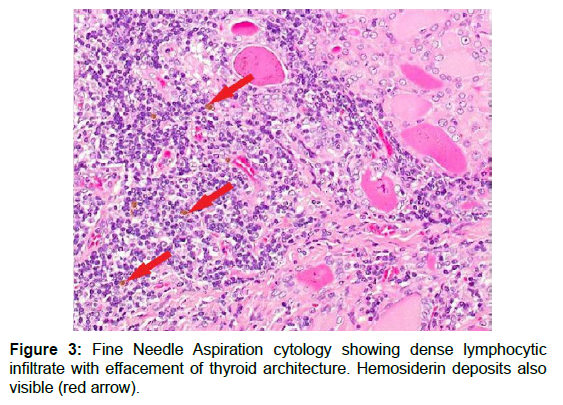
Detailed history revealed that she was diagnosed with Hashimoto thyroiditis 2 years prior without any precipitating factors on routine wellness check and had positive anti Thyroid peroxidase (TPO) antibodies. She did not have any neck swelling nor constitutional symptoms. Thyroid ultrasound did not reveal any nodules. Fine Needle Aspiration Cytology was performed to confirm the diagnosis which revealed lymphocytic infiltrate supporting diagnosis of asymptomatic Hashimoto thyroiditis. Additionally, hemosiderin deposits were also visible but not taken under consideration (Figure 3). Due to recent diagnosis of Hemochromatosis, a possible link was suspected due to iron deposition. TRH measured at the time of diagnosis was normal ruling out hypothyroidism secondary to iron deposition. Patient was started on diuretics and 1.5 liter fluid restriction, as well as prednisolone for possible alcoholic cirrhosis component. Hematology follow-up was planned for phlebotomy to prevent further iron overload and patient did well on 6-month follow up.
Discussion
Multiple studies have proven that the deposition of iron in HH occurs not only in the anterior pituitary but in the thyroid gland as well [4,7]. However it is rare in patients with HH to have thyroid dysfunction, and the detection of abnormal thyroid function is only apparent at a late/end stage when the patient has already developed liver cirrhosis and/or other endocrinopathies entailed with HH [8]. This could be attributed to the fact that unlike the extensive iron deposition that occurs in the gonadotrophs, the deposition of iron is limited to only a small number of thyrotrophs [9]. Abnormalities in the pituitary thyrotrophs are well described and documented in patients with HH, [5,10,11] however primary thyroid dysfunction ultimately leading to hyperthyroidism or hypothyroidism in patients with HH has also been studied and reported; most notably in men with HH type 1 [8].
A possible link between type 1 HH and autoimmune thyroid disease has been suggested, based on the exposure of cellular antigens, like thyroid peroxidase (TPO) and thyroglobulin (Tg), due to iron deposition and damage of the thyroid cell, allowing a subsequent production of anti-thyroid antibody [8,12,13]. However no significant difference in the prevalence of thyroid disease between HH type 1 patients and non-affected controls was found in larger studies and thus they have not confirmed the above hypothesis [14,15]. In a cohort of 150 Irish patients with HH type I, only one case of male primary hypothyroidism (0.6 %), two cases of female subclinical hypothyroidism (1.3 %) and no cases of hyperthyroidism have been described [15]. Similarly in the Hemochromatosis and Iron Overload Screening Study (HEIRS), where serum TSH and free T4 levels were measured in 176 white HFE C282Y homozygote patients and 312 controls, the prevalence of hypothyroidism or hyperthyroidism was very low and did not differ between the two groups (1.7 % in HH and 1.3 % in controls; 0 % in HH and 1.0 % in controls, respectively) [14]. This study did not find any association between the severity of iron overload and primary thyroid dysfunction despite significantly high transferrin levels in patients with type 1 HH. Therefore, it has been reported that patients with primary hypothyroidism and heavy iron overload resulting from transfusion do not have positive titres of antibodies [15]. Anecdotally, an autoimmune thyroiditis has also been described and brought to light in two siblings with type 2 HH, however there is no evidence to form a pathogenic link [16]. Therefore, these studies support the concept that a primary thyroid dysfunction may occasionally occur in all forms of HH and that this association is likely coincidental.
Conclusion
In conclusion, though it is common practice to test for other organ dysfunction in hemochromatosis, the reverse should also be sought. Our case highlights the possible benefit of testing for deposition related diseases, particularly hemochromatosis in case of unknown etiology for thyroiditis. Because of the potential recovery of thyrotroph secretion following iron depletion therapy, thyroxine replacement therapy should be withheld when the patient has been rendered adequately iron deplete, and the thyroid function should be reassessed to determine whether or not recovery of the pituitary-thyroidal axis has occurred.
References
- Milman N (2000) Inheritance of haemochromatosis: family studies. In: Barton JC, Edwards CQ (eds) Haemochromatosis. Cambridge University Press, Cambridge, UK, p:15.
- Pelusi C, Gasparini DI, Bianchi N, Pasquali R (2016) Endocrine dysfunction in hereditary hemochromatosis. J Endocrinol Invest 39(8):837?847.
- McDermott JH, Walsh CH (2005) Hypogonadism in hereditary haemochromatosis. J Clin Endocrinol Metab 90:2451–2455.
- McDonald RA, Mallory GK (1960) Haemochromatosis and hemosiderosis: study of 211 autopsied cases. Arch Int Med 105:52–66.
- Gama R, Smith MJ, Wright J, Marks V (1995) Hypopituitarism in primary haemochromatosis: recovery after iron depletion. Postgrad Med J 71:297–298.
- Wilkinson H (1996) Haemochromatosis associated with arthritis and hypopituitarism. Ann Clin Biochem 33:171–173.
- Bergeron C, Kovacs K (1978) Pituitary siderosis. A histologic, immunocytologic, and ultrastructural study. Am J Pathol 93:295–309.
- Edwards CQ, Kelly TM, Ellwein G, Kushner JP (1983) Thyroid disease in hemochromatosis. Increased incidence in homozygous men. Arch Intern Med 143:1890–1893.
- Tournaire J, Fevre M, Mazenod B, Ponsin G (1974) Effects of clomiphene citrate and synthetic LHRH on serum luteinizing hormone (LH) in men with idiopathic hemochromatosis. J Clin Endocrinol Metab 38:1122–1124.
- McNeil LW, McKee LC Jr, Lorber D, Rabin D (1983) The endocrine manifestations of hemochromatosis. Am J Med Sci 285:7–13.
- Hudec M, Grigerova M, Walsh CH (2008) Secondary hypothyroidism in hereditary hemochromatosis: recovery after iron depletion. Thyroid 18:255–257.
- Williams RS (1959) Increased thyroid function in haemochromatosis. Br Med J 1:1078–1080.
- Tamagno G, De CE, Murialdo G, Scandellari C (2007) A possible link between genetic hemochromatosis and autoimmune thyroiditis. Minerva Med 98:769–77.
- Barton JC, Leiendecker-Foster C, Reboussin DM, Adams PC, Acton RT, et al. (2008) Thyroid-stimulating hormone and free thyroxine levels in persons with HFE C282Y homozygosity, a common hemochromatosis genotype: the HEIRS study. Thyroid 18:831–838.
- Murphy MS, Walsh CH (2004) Thyroid function in haemochromatosis. Ir J Med Sci 173:27–29.
- Barton JC, Rao SV, Pereira NM, Gelbart T, Beutler E, et al. (2002) Juvenile hemochromatosis in the southeastern United States: a report of seven cases in two kinships. Blood Cells Mol Dis 29:104–115.
Citation: Sheikh T, Rehman H, Shuja H (2020) Thyroiditis heralding Hereditary Hemochromatosis: an unusual initial manifestation and review of literature. J Gastrointest Dig Syst 10: 628. DOI: 10.4172/2161-069X.1000628
Copyright: © 2020 Sheikh T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3701
- [From(publication date): 0-2020 - Mar 14, 2025]
- Breakdown by view type
- HTML page views: 3023
- PDF downloads: 678