Case Report Open Access
Thoracic Myelolipoma: A Rare Case of Mistake in Lung Cancer Staging
Ludovic Fournel1,2*, Audrey Mansuet-Lupo1,3, Marie-Pierre Revel1,4 and Jean-François Régnard 1,21Paris Descartes-Paris University, France
2Thoracic Surgery Department, Hôpitaux Universitaire Paris Centre, AP-HP, Paris, France
3Pathology Department, Hôpitaux Universitaire Paris Centre, AP-HP, Paris, France
4Radiology Department, Hôpitaux Universitaire Paris Centre, AP-HP, Paris, France
- *Corresponding Author:
- Ludovic Fournel
Thoracic surgery Department
Cochin Hospital
Hôpitaux Universitaire Paris Centre
Assistance Publique des Hôpitaux de Paris
Paris Descartes University, Paris, France
Tel: 33-6-21890633
Fax number : 33 145012067
E-mail: ludfoul@hotmail.com
Received Date: November 14, 2014; Accepted Date: December 13, 2014; Published December 20, 2014
Citation: Fournel L, Mansuet-Lupo A, Revel MP, Régnard JF (2014) Thoracic Myelolipoma: A Rare Case of Mistake in Lung Cancer Staging. J Clin Exp Pathol 5:202. doi: 10.4172/2161-0681.1000202
Copyright: ©2014 Fournel L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Myelolipomas are benign tumors containing hematopoietic and fatty elements. They are commonly located in the retroperitoneum and mainly characterized by low density and low 18-FDG uptake on computed and positronemission tomography imaging. We report here a very rare case of middle lobe lung carcinoma occurring together with a hyper metabolic right posterior thoracic nodule leading to a diagnosis of metastatic location by mistake. A CTguided core-needle biopsy was then performed and demonstrated the presence of both mature fat and hematopoietic tissue which was highly suggestive of myelolipoma. It allowed for curative treatment of the lung carcinoma and resection of the myelolipoma in the same time.
Keywords
Lung cancer surgery; Lung metastasis; Mediastinum
Case report
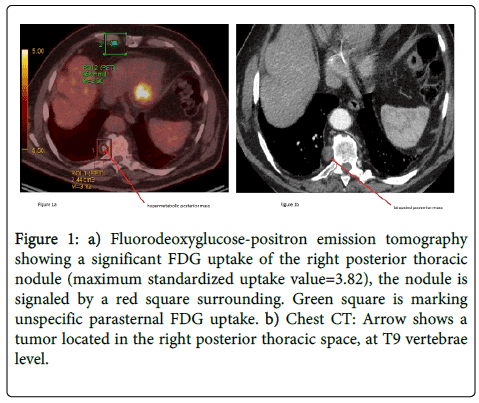
A 76-year-old man was referred to a thoracic department for the surgical management of a right hilar mass. This patient was smoker with no comorbidity except hypertension. Chest CT showed an 8 cm spiculated proximal tumor of the middle lobe associated with an incomplete atelectasis of the same lobe. This mass was associated with a 3 cm right posterior mass, located at T9 level, with incomplete low density, without bone erosion or pleural effusion. 18F-FDG PET/CT revealed a high FDG uptake of the lung tumor (maximum standardized uptake value=17.4) and a significant uptake of the paravertebral nodule (maximum standardized uptake value=3.82) (Figure 1).
Figure 1: a) Fluorodeoxyglucose-positron emission tomography showing a significant FDG uptake of the right posterior thoracic nodule (maximum standardized uptake value=3.82), the nodule is signaled by a red square surrounding. Green square is marking unspecific parasternal FDG uptake. b) Chest CT: Arrow shows a tumor located in the right posterior thoracic space, at T9 vertebrae level.
The diagnosis of lung squamous cell carcinoma was obtained by fiber-optic bronchoscopy. The presence of the paravertebral image led a first thoracic institution to exclude surgical resection of this cT3N0 carcinoma.
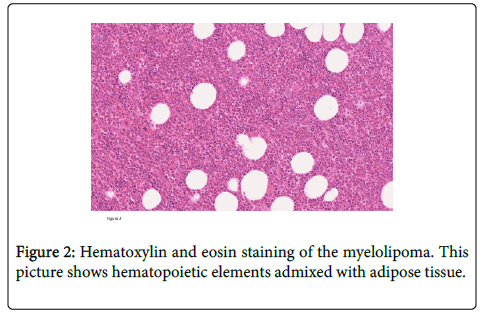
Considering the unusual presentation of this presumed metastasis, our team decided to perform a CT-guided core-needle biopsy of the paravertebral nodule. Macroscopic examination showed a specific pattern with reddish-brown tissue. Microscopic analysis, using hematoxylin and eosin staining, demonstrated the presence of both mature fat (empty holes were likely to be fat cells) and hematopoietic tissue, including myeloid, erythroid, and megakaryocytic elements (Figure 2). At immunohistochemistry, using protein S100 antibodies, these latter cells were positive, which confirmed the presence of adipose tissue. Pathologic findings were consistent with the diagnosis of mediastinal extra-adrenal myelolipoma. No sign of malignancy was observed.
Finally, we performed an open middle lobectomy with mediastinal lymph node dissection together with the resection of the paravertebral nodule.
Permanent pathologic examination confirmed the diagnosis of myelolipoma for the paravertebral mass. The hematopoietic tissue was predominant (70%) compared to mature fat tissue (30%). The middle lobe tumor was staged as a pT3N0 adenocarcinoma. The postoperative course was uneventful.
Discussions
We report here a very rare case of benign hyper metabolic nodule, diagnosed during the staging of a lung carcinoma, which pathologic analysis revealed a mediastinal myelolipoma. Myelolipomas are mesenchymal tumors composed of hematopoietic elements and mature adipose tissue resembling bone marrow, without trabecular bone. This disease was first described in 1905, and was given the name ‘myelolipoma’ in 1929 [1]. Myelolipomas are benign tumors, and most of them are detected in the adrenal glands. About half of all extraadrenal myelolipomas are located in the retroperitoneum and only 3% occur in the mediastinum [2]. These tumors are typically unilateral, asymptomatic and incidentally diagnosed by imaging detection. Rare cases of bilateral multiple mediastinal myelolipomas have been described and may occur [3]. When they are large-sized (>4 cm), they could be responsible for symptoms such as chest pain, compression of adjacent organs or hemorrhage.
There is no specific sign on CT to diagnose myelolipoma, even though presence of a heterogeneous and low density “adipose like” image could be suggestive. In the case we report, presence of a significant 18F-FDG uptake of a paravertebral nodule together with a biopsy-proven middle lobe lung carcinoma was very confusing. The difference between this thoracic myelolipoma and previously reported ones is the simultaneous occurrence of a lung carcinoma and an ipsilateral mediastinal myelolipoma. No similar case is described. Additionaly, myelolipomas commonly show no significant 18F-FDG uptake which isn’t the case in this patient. Increased 18F-FDG uptake is rarely reported in adrenal myelolipomas [4]. In our case, the hematopoietic tissue was predominant, explaining its hyper metabolism on PET imaging. Consequences of this misdiagnosis were major because the patient would not benefit a curative intent treatment of his lung carcinoma if a second review had not been performed.
Finally, the core-needle biopsy allowed us for ruling out a metastatic location of the pulmonary carcinoma. To our knowledge, there are few reports of successful diagnosis of myelolipoma basing on CT or MRI appearances [5]. Main differential diagnosis is a thoracic location of extra medullary hematopoietic tissue. Presence of chronic anaemia due to hematological diseases such as thalassemia or hereditary spherocytosis or medullar deficiency diseases can be used to differentiate myelolipoma to extra medullary haematopoiesis but our patient had no history of hematologic disorder and the blood count was normal.
Even if there is no standard management of mediastinal myelolipoma, we obviously chose to remove it together with the lung carcinoma, in a diagnostic and curative intent. Concerning resection of isolated myelolipomas, small asymptomatic tumors (<4 cm max diameter) are usually monitored, while symptomatic tumors or large myelolipomas (>7 cm max diameter) are much likely to be removed because of a higher possibility of rupture and bleeding.
Conclusion
Presence of a thoracic myelolipoma together with an ipsilateral lung carcinoma is a rare and confusing case.
References
- Oberling C (1929) Les myelolipomatoses. Bull AssocFr Etudes. Cancer 18: 234-246.
- Franiel T, Fleischer B, Raab BW, Füzesi L (2004) Bilateral thoracic extraadrenalmyelolipoma. Eur J CardiothoracSurg 26: 1220-1222.
- Nakagawa M, Kohno T, Mun M, Yoshiya T (2014) Bilateral video-assisted thoracoscopic surgery resection for multiple mediastinalmyelolipoma: report of a case. Korean J ThoracCardiovascSurg 47: 189-192.
- Castinetti F, Verschueren A, Cassagneau P, Brue T, Sebag F (2012) Adrenal myelolipoma: an unusual cause of bilateral highly 18F-FDG-avid adrenal masses. J ClinEndocrinolMetab 97: 2577-2578.
- Kawanami S, Watanabe H, Aoki T, Nakata H, Hayashi T (2000) Mediastinalmyelolipoma: CT and MRI appearances. EurRadiol 10: 691-693.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 15263
- [From(publication date):
specialissue-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10711
- PDF downloads : 4552