Research Article Open Access
Therapeutic Strategies for Post-Osteosynthesis Osteomyelitis
Dell'Aquila AM1*, Finelli CA1, Fernandes HJA1, Reis FB1, Marra AR1, Pereira CAP1 and Morais JF21Federal University of São Paulo, São Paulo, Brazil
2Federal University of Uberlandia, Brazil
- *Corresponding Author:
- Adriana Macêdo Dell’Aquila
Infectious Diseases Discipline, Federal University of São Paulo
Rua Napoleão de Barros, 715, 7andar Vila Clementino
São Paulo, CEP 04024-002, Brazil
Tel: +5511-55764094
E-mail: aaquila@terra.com.br
Received date: November 30, 2016; Accepted date: January 16, 2017; Published date: January 18, 2017
Citation: Dell'Aquila AM, Finelli CA, Fernandes HJA, Reis FB, Marra AR, et al. (2017) Therapeutic Strategies for Post-Osteosynthesis Osteomyelitis. J Infect Dis Ther 5:312. doi:10.4172/2332-0877.1000312
Copyright: © 2017 Dell'Aquila AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Objectives: The main objective in post-osteosynthesis surgical site infection (SSI) is to consolidate the fracture and prevent chronic osteomyelitis. The purpose of this study is to evaluate the risk factors for SSI recurrence in patients treated for osteo-articular infection at the Federal University of São Paulo.
Methods: After retrospectively evaluating all SSI episodes occurring from December 2004 to December 2008 in patients undergoing osteosynthesis at the orthopedics department, 110 of them were included. SSIs were treated with at least 4-6 week antibiotic therapy cycles and followed up for one year with the results being analyzed using univariate and multivariate analysis models.
Results: Most patients were 18-89 years old, with a mean age of 39.8, the majority being male (84.5%). In 37 patients, the causative agent was isolated with Staphylococcus being the most frequently observed (38.8%). In 83 (75.4%) patients, the antimicrobial treatment mostly with ciprofloxacin and clindamycin was started within less than five days from the onset of symptoms. SSI recurrence occurred in 34/110 (30.9%) patients. After one-year follow-up, 19 (17.3%) patients persisted with infection and only 10 (9.1%) did not have their fractures consolidated. The univariate analysis showed the performance of more than one surgery to stabilize the affected limb (OR 3.7 IC95=1.1-12.7 p=0.045), presence of converting osteosynthesis (OR 3.6 IC95=1.1-11.3 p=0.023), internal synthesis (OR 3.0 IC95=0.99-9.2 p=0.043) and longer duration of surgery (OR 0.4 IC95=0.1-1.6 p=0.029) as risk factors for SSI recurrence. In the multivariate analysis, the only variable independently associated with SSI relapse was duration of surgery (OR 1.3 IC95=1.1-1.7 p=0.015).
Conclusions: After one year follow-up, using a specific protocol, most patients showed resolution of infection and only 9.1% had their fractures unconsolidated. The only independent risk factor associated with SSI recurrence was prolonged surgery. It is possible to treat a patient with post-osteosynthesis SSI with a course of 4 to 6 weeks of antibiotic therapy.
Keywords
Surgical wound infection; Fracture fixation; Osteomyelitis; Risk factors; Recurrence
Introduction
According to the World Health Organization figures in 2014, by the year 2050 the number of deaths attributable to antimicrobial multiresistance (AMR) will have reached 10 million [1]. SSI is the third most commmon nosocomial infection which accounts for 14 to 16% of hospitalized patients and 38% of surgical patients [2]. SSI in orthopaedic trauma may vary between 0.9 and 12.5% and the worst complication is osteomyelitis, especially the chronic form [3-6] Chronic osteomyelitis resulting from post-trauma surgical infection can be treated with aggressive debridment and skin dressing together with intravenous antibiotics for 5 to 7 days followed by 6 weeks of oral antibiotics resulting in fracture consolidation without complications [7-9].
With implants, antibiotic should be administered for 3 to 6 months [10] Sometimes it is difficult to define the depth of the post-trauma infection and multiresistent organisms may develop after prolonged antibiotic therapy [11]. However, some patients may benefit from short-term antimicrobial treatment, and risk factors for the orthopaedic device infection recurrence after a 4- 6 week cycle of treatment were assessed.
The objective of this study is to evaluate clinical, microbiological and epidemiological aspects in post osteosynthesis infection and the risk factors for the recurrence of infection after 4 to 6 weeks of treatment.
Materials and Methods
All patients of post-operative orthopaedic trauma and all patients with Osteoarticular infection were follwed up by an infectious disease specialist with twelve years’ experience (AMDA), in the Orthopaedic and Trauma Department of the São Paulo Hospital of the Federal University, Brazil, from December 2004 to December 2008.
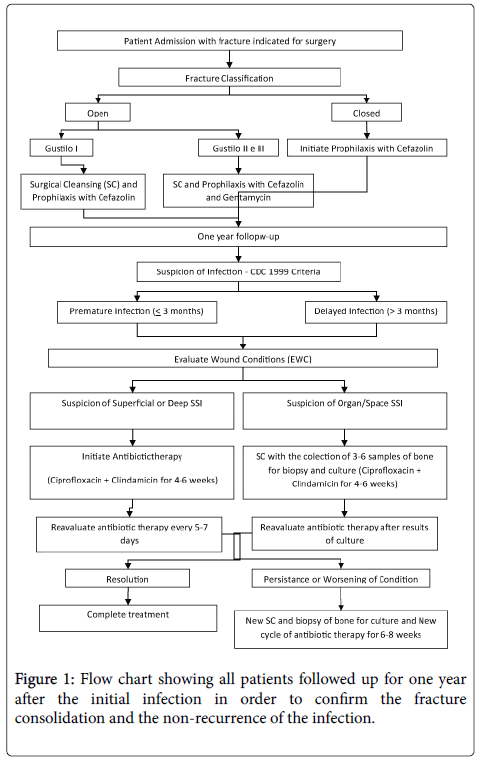
Cases which met the criteria for post-trauma osteosynthesis infection were selected for this retrospective study. The patients included were all over 18 years old, post-trauma, who had undergone ostheosyntesis, wihout prostheses. The orthopaedic traumas where classified as open or closed using Gustilo & Anderson scale (1976). Cefazolin was administered for 48h after surgery and Gentamycin was included for 5 days in open fractures in Gustilo II and III. The patients who developed infection were defined in accordance with CDC criteria, 1999 and biopsies (3 to 6 samples) were performed of bone and surrounding tissue. Infection classified as deep incisional and organ/space were treated with antibiotics for an average of 4 to 6 weeks, the latter underwent surgical cleansing. In the cases of reappearance of infection after at least one month of remission, classified as recurrence, further surgical cleansing was performed together with 6 to 8 weeks of antibiotics. All patients were followed up for one year after the initial infection in order to confirm the fracture consolidation and the non-recurrence of the infection (Figure 1).
Patients with a previous nosocomial infection in a different site, post-operative infection without osteosynthesis, previous history of chronic osteomyelitis or more than one surgical infection site were excluded from the study. The risk factors analyzed for recurrence were age, gender, history of smoking and alcoholism, pre-existing conditions, type of accident, number of bone fractures, articular involvement, type of fracture (open or closed), number of surgical procedures prior to infection, duration of the first osteosynthesis, adequate antimicrobial prophylaxis, type of material used in the osteosynthesis, presence of osteosynthesis conversion prior to infection, time between the initial symptoms and treatment, and time between fracture and osteosynthesis. Microbiological analysis was carried out following the CLSI regulations (2007) and the follow-up of the fracture consolidation and treatment of infection was done over one year. The model of univariate and multivariate logistic regression was used for the analysis of risk factor of post-treatment infection recurrence.
Results
Of all the patients admitted to the Orthopaedic and Trauma Department, 436 patients presented with osteoarticular infection. Of these, 195 (44.7%) were classified as chronic, 117 (26.8%) developed post-osteosynthesis nosocomial infection, 57 (13.1%) had contiguous osteomyelitis, 34 (7.8%) had prosthesis infection, 27 (6.2%) pyogenic arthritis and 6 (1.4%) hematogenous osteomyelitis (Table 1).
| Type of Infection | N | Percentage |
|---|---|---|
| Chronic Osteomyelitis | 195 | 44.7 |
| Post-Osteosynthesis Infection | 117 | 26.8 |
| Contiguous Osteomyelitis | 57 | 13.1 |
| Pyogenic Arthritis | 27 | 6.2 |
| Hip Arthroplasty Infection | 23 | 5.3 |
| Knee Arthroplasty Infection | 8 | 1.8 |
| Hematogenous Osteomyelitis | 6 | 1.4 |
| Shoulder Arthroplasty Infection | 1 | 0.2 |
| Elbow Arthroplasty Infection | 2 | 0.5 |
| Total | 436 | 100 |
Table 1: Distribution of 436 patients presented with Osteoarticular Infection at the Hospital São Paulo between December 2004 to December 2008.
Of the 117 patients with post osteosynthesis infection, 110 between the age of 18 and 89 with a mean age of 39.8 years were included, with the majority (84.5%) being male. Among this group 33.6% were smokers, 9.1% consumed alcohol daily and the majority (73.6%) had no previous disease. Motorcycle accident was the most prevalent cause of trauma (44.5%) and 90% had one or two fractures. Articular involvement was seen in 51.8% of cases and 53.6% were closed fractures. Most of the cases were infection of the tibia and fibula, mainly the proximal segment and the malleolus region (44B3 and 42C2 AO Trauma Classification).
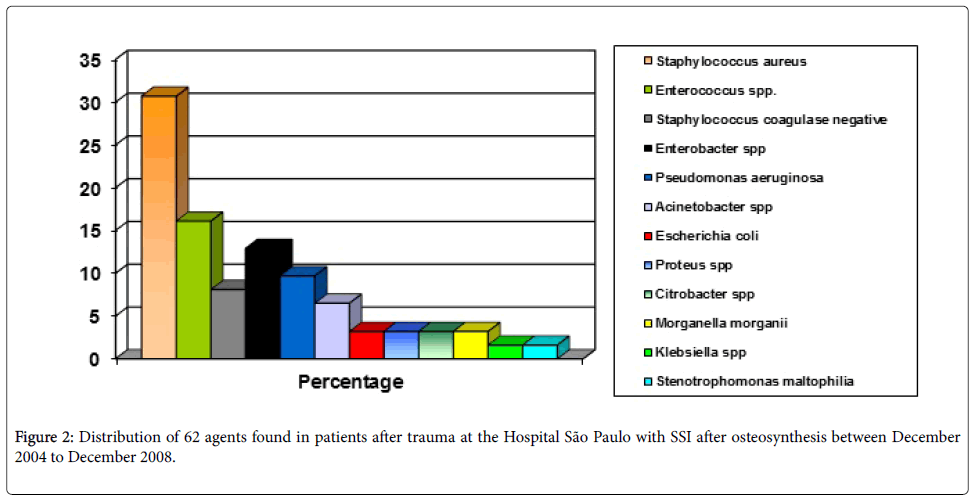
The majority of the patients underwent only one surgery (89.1%), without conversion (87.2%) and 54.5% had plate and screws inserted and duration of surgery greater than 2 h (81.8%). The antibiotic prophylaxis was inadequate in 76.4% and corrective surgery was carried out also on 76.4% within five days of admission. In 37 patients Staphylococcus (S.aureus and SCoN) was the most frequently isolated (38.8%) (Figure 2). In 83 patients (75.4%) antimicrobial treatment of infection was initiated in less than five days from symptoms and ciprofloxacin and clindamycin were the most used (Table 2). The average time between surgery and onset of SSI was 54.5 days with a median of 16 days, 69.49% developed infection within 30 days, 84.75% within 90 days and 88.14% within 180 days.
| Antibiotic | N | Percentage |
|---|---|---|
| Clindamycin | 91 | 82.7 |
| Ciprofloxacin | 91 | 82.7 |
| Vancomycin/Teicoplanin | 31 | 28.2 |
| Cefepime | 16 | 14.5 |
| Imipenem/Meropenem | 13 | 11.8 |
| Cefalotin/Cefalexin | 6 | 5.5 |
| Rifampicin | 5 | 4.5 |
| Ampicillin/Amoxacillin | 4 | 3.6 |
| Sulfamethoxazole/Trimethoprim | 3 | 2.7 |
| Ceftriaxone | 3 | 2.7 |
| Amikacin/Gentamicin | 3 | 2.7 |
| Oxacillin | 2 | 1.8 |
| Ertapenem | 2 | 1.8 |
| Polymyxin B | 2 | 1.8 |
| Levofloxacin/Moxifloxacin | 2 | 1.8 |
| Linezolid | 1 | 0.9 |
Table 2: Antibiotics used in SSI patients at the Hospital São Paulo between December 2004 to December 2008.
Of 110 patients assessed, infection recurred in 34 (30.9%), in 19 (17.3%) the infection persisted at the end of one year follow-up and in 10 (9.1%) the fracture was not consolidated. Univariate analysis showed more than one surgery to stabilize the affected limb (OR 3.7 IC95=1.1-12.7 p=0.045), presence of converting osteosynthesis (OR 3.6 IC95=1.1-11.3 p=0.023), internal synthesis (OR 3.0 IC95=0.99-9.2 p=0.043), and longer duration of surgery (OR 0.4 IC95=0.1-1.6 p=0.029) as risk factors for SSI recurrence (Table 3). In the multivariate analysis, the only variable independently associated with SSI recurrence was duration of surgery (OR 1.3 IC95=1.1-1.7 p=0.015) (Table 4).
| Variables | Recurrence | Non Recurrence | Univariate | ||||
|---|---|---|---|---|---|---|---|
| N (34) | % | N (76) | % | OR | CI 95% | p | |
| Gender | |||||||
| Male | 31 | 91.2 | 62 | 81.6 | 2.333 | 0.624 -8.729 | 0.198 |
| Age | |||||||
| 18 a 44 | 19 | 55.9 | 54 | 71.1 | 0.161 | ||
| 45 a 64 | 9 | 26.5 | 13 | 17.1 | |||
| >64 | 6 | 17,6 | 9 | 11,8 | |||
| Base Disease | |||||||
| Absent | 23 | 67.6 | 58 | 76.3 | 0.649 | 0.266 -1.584 | 0.34 |
| Type of Accident | |||||||
| Traffic Accident | 27 | 79.4 | 47 | 61.8 | 2.38 | 0.919 -6.163 | 0.07 |
| Others | 7 | 20.6 | 29 | 38.2 | |||
| Number of Fracture | |||||||
| 1 | 11 | 32.4 | 39 | 51.3 | 0.454 | 0.194 -1.059 | 0.065 |
| >2 | 23 | 67.6 | 37 | 48.7 | |||
| Articular Involvement | |||||||
| Yes | 15 | 44.1 | 42 | 55.3 | 0.639 | 0.283 -1.443 | 0.28 |
| Type of Fracture | |||||||
| Closed | 19 | 55.9 | 39 | 51.3 | 1.202 | 0.533 -2.709 | 0.658 |
| Open | 15 | 44.1 | 37 | 48.7 | |||
| Type of Synthesis | |||||||
| Internal | 26 | 76.5 | 69 | 90.8 | 3.033 | 0.999 -9.204 | 0.043 |
| External | 8 | 23.5 | 7 | 9.2 | |||
| Number of Surgeries | |||||||
| 1 | 27 | 79.4 | 71 | 93.4 | 3.676 | 1.075 -12.658 | 0.045 |
| >2 | 7 | 20,6 | 5 | 6,6 | |||
| Adequate Prophylixis | |||||||
| Yes | 4 | 11.8 | 22 | 28.9 | 0.327 | 0.103 -1.039 | 0.056 |
| Type of Convertion | |||||||
| Without convertion | 26 | 76.5 | 70 | 92.1 | 3.59 | 1.136 -11.340 | 0.023 |
| With convertion | 8 | 23.5 | 6 | 7.9 | |||
| Lenght of Surgery (hours) | |||||||
| <2 | 4 | 11.7 | 16 | 21.1 | 0.372 | 0.087 -1.563 | 0.029 |
| 2 a 3.9 | 14 | 41.2 | 39 | 51.3 | |||
| 4 a 5.9 | 11 | 32.4 | 15 | 19.7 | |||
| 6 a 7.9 | 2 | 5.9 | 6 | 7.9 | |||
| >8 | 3 | 8.8 | 0 | 0 | |||
| Average +Standard Deviation (SD) | 4.10 + 2.15 | 3.28 + 1.63 | |||||
| Time between Fracture and Surgery (days) | |||||||
| Same day | 11 | 32.4 | 31 | 40.8 | 0.995 | ||
| 1 a 5 | 17 | 50 | 25 | 32.9 | |||
| >5 | 6 | 17.6 | 20 | 26.3 | |||
| Median(Percentil 25-Percentil 75) | 1.5 (0-5) | 1 (0-5) | |||||
| Time between Symptoms and Treatment (days) | |||||||
| 0 - 5 | 25 | 73.5 | 58 | 76.3 | 0.797 | ||
| >5 | 9 | 26.5 | 18 | 23.7 | |||
| Median(Percentil 25-Percentil 75) | 0 (0-6) | 0 (0-3) | |||||
Table 3: Univariate analysis of risk factors for recurrence of SSI of the 110 post-trauma patients at the Hospital São Paulo with SSI after osteosynthesis between December 2004 to December 2008.
| Variables | R | NR | Multivariate | ||||
|---|---|---|---|---|---|---|---|
| N (34) | % | N (76) | % | OR | CI 95% | p | |
| Type of Synthesis | |||||||
| Internal | 26 | 76.5 | 69 | 90.8 | 0.329 | 0.080 -1.361 | 0.125 |
| External | 8 | 23.5 | 7 | 9.2 | |||
| Number of Surgeries | |||||||
| 1 | 27 | 79.4 | 71 | 93.4 | 1.726 | 0.065 -45.882 | 0.744 |
| >2 | 7 | 20.6 | 5 | 6.6 | |||
| Type of Convertion | |||||||
| Without | 26 | 76.5 | 70 | 92.1 | 0.275 | 0.015 -5.113 | 0.386 |
| With | 8 | 23.5 | 6 | 7.9 | |||
| Lenght of Surgery/(hours) | |||||||
| <2 | 4 | 11.7 | 16 | 21.1 | 1.344 | 1.058 -1.709 | 0.015 |
| 2 a 3,9 | 14 | 41.2 | 39 | 51.3 | |||
| 4 a 5,9 | 11 | 32.4 | 15 | 19.7 | |||
| 6 a 7,9 | 2 | 5.9 | 6 | 7.9 | |||
| >8 | 3 | 8.8 | 0 | 0 | |||
| Average + SD | 4.10 + 2.15 | 3.28 + 1.63 | |||||
| NR: Non-Recurrence; R: Recurrence | |||||||
Table 4: Multivariate analysis of risk of SSI recurrence in post-trauma osteosynthesis from December 2004 to December 2008.
Discussion
In the last 30 years, chronic osteomyelitis has been largely undefined with differences among authors of best definition and time of treatment [12].
Of all cases initially seen in the Orthopaedic Department, chronic infection was already present in 50% and post-trauma nosocomial osteosynthesis infection in 30%. The SSI is the most important complication of orthopaedic surgery and can evolve into acute or chronic osteomyelitis.
Despite the fact that antibiotics are only administered for two weeks in skin infection, in this study antibiotics were given between 4 and 6 weeks in order to reduce the risk of recurrence and to avoid the growth of bacteria in the process of revascularization and consolidation, since most fractures consolidate between 6 to 8 weeks [13].
Based on Cierny-Mader classification for osteomyelitis, the antimicrobial treatment could be; stage 1, four weeks (hematogenous and medular, even after removal of intramedullary nailing shaft), stage 2, two weeks following debridement and soft tissue graft, stages 3 and 4, four to six weeks from the last debridement [14,15].
Although this preventative measure was used, infection recurred in 30% of patients with the risk of chronic osteomyelitis. In cases of recurrence, patients underwent further surgical treatment and another 6 week course of antibiotics. One year after the onset, SSI persisted in 17.3% even with treatment of 6 weeks, but in only 9.1% the fracture was not consolidated and considered as a failure, seeing as the most important thing in trauma is the consolidation of the fracture.
In the recurrence of the infection, the same agent was not always identified as had been previously. Even with a prolonged course of antibiotics of 3 to 6 months, recurrence of infection can be seen, with an increase in cost of treatment, since the sequestrum of the bone can require multiple surgical intervention to control the infection [16]. The majority of fractures consolidated even with implants and using short cycles of antibiotics. The cases that did not consolidate were of trauma of the tibia.
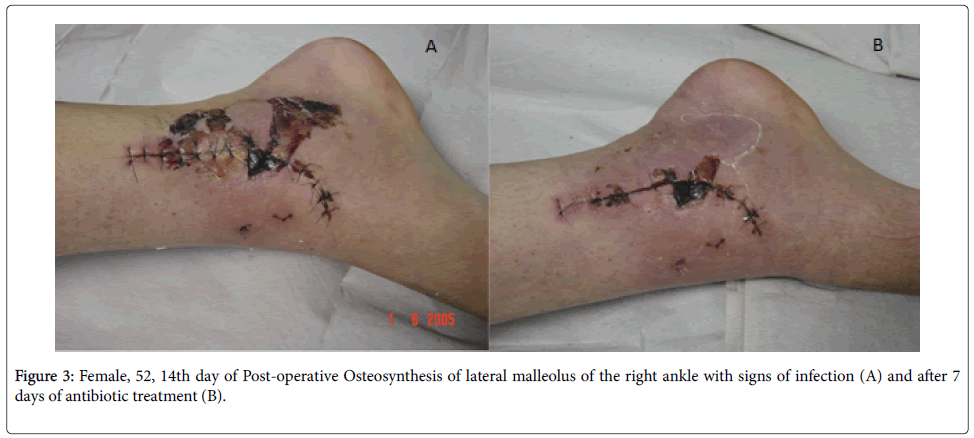
Due to the proximity of the skin to the bone structure and the inflammatory process the diagnosis of osteomyelitis, post-trauma and post-ostesynthesis, is often dubitable. Close supervision of the healing process of post-operative osteosynthesis of the fracture is necessary since the initial aspect of the wound is difficult to distinguish from the onset of infection. It is important to be aware of the presence of pus, increase in devitalized tissue and delay in the healing process (Figure 3). Probably the experience of an infectologist enabled the early initiation of antimicrobial treatment in less than five days from symptoms in the majority of patients.
Even when dealing with cases involving implants, infection appeared in an average of 16 days, 70% being within 30 days and the majority (85%) in three months.
The only independent risk factor for the recurrence of the infection, which could be defined as a risk for the chronic form, was the duration of surgery (OR=1.344), for every hour of surgery beyond the initial two hours, the risk of SSI increases by 4%. The duration of surgery is already a known risk factor for the development of SSI in inumerous procedures, however, this is the first study in which this variable was found to be a risk factor for the recurrence of SSI post-osteosynthesis and the risk can be diminished by the reduction in the time of the surgery.
Some patients temporarily remain with the limb stabilized using external fixation and later undergo conversion to a definitive internal fixation. Diverse factors may influence the presence of the infection such as the prolonged hospital stay, the possibility of bacteria colonization on the pins of the fixation device and the inadequate covering of the soft tissue at the site of fracture.
Staphylococcus spp. are the the most commonly found agents in orthopaedic implant infections [17]. The prolonged use of antimicrobials in treatment can result in resistance as with Staphylococcus aureus with reduced susceptibility to vancomycin such as VISA and hetero-VISA [11,18].
Despite the fact that the prolonged period of hospitalization can cause SSI, an increased risk of recurrence was not seen in this study. The mean length of surgery was high due to the complexity of the surgery and the fact that the study was carried out in a teaching hospital.
The cost of post-operative orthopaedic infection is high and increased further in cases of bone infection and prolonged hospitalization. The proposal of short cycles of antibiotics from 4 to 6 weeks following surgical debridement could be an alternative to the treatment of post-operative infection in orthopaedic trauma and could reduce the number of patients who develop resistance to antibiotics.
After one year of follow-up using this protocol, the majority of patients was cured and in only 9,1% fracture was not consolidated. Recurrence of the infection was seen in one third of patients and the only independent risk factor associated with this was the prolonged duration of surgery. Therefore, victims of orthopaedic trauma with fractures, whenever possible, should have a previously programmed surgery regarding the material of the implant necessary for the procedure, in order to require only one definitive implant without the necessity of surgical conversion. However, the length of surgery should be strictly controlled to a maximum of two hours and should not exceed four hours so as to reduce the risk of post operative infection recurrence and the risk of developing chronic osteomyelitis. When possible, as with cases of closed fractures, the surgery can be delayed for a few days without affecting the development of infection.
Conclusion
After one year follow-up, using a specific protocol, most patients showed resolution of infection and only 9.1% had their fractures unconsolidated. The only independent risk factor associated with SSI recurrence was prolonged surgery. It is possible to treat a patient with post-osteosynthesis SSI with a 4 to 6 week course of antibiotics since the goal is the consolidation of the fracture. However these patients should be closely monitored by an infectologist, since in the relapse, a new cycle of treatment after debridement should be initiated to avoid developing into the chronic form and the non consolidation of the fracture.
References
- https://amr-review.org/
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20: 247-278.
- Thu LT, Dibley MJ, Ewald B, Tien NP, Lam LD (2005) Incidence of surgical site infections and accompanying risk factors in Vietnamese orthopaedic patients. J Hosp Infect 60: 360-367.
- Ochsner PE, Majewski M, Plaass C (2005) Infection after osteosynthesis: a summary of the scientific presentations at the annual Swiss AO meeting 2005 in Liestal. Injury 37: S59-S66.
- Astagneau, Rioux C, Golliot F, Brücker G, INCISO Network Study Group (2001) Morbidity and mortality associated with surgical site infections: results from the 1997-1999 INCISO surveillance. J Hosp Infect 48: 267-274.
- Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, et al. (2009) National Heathcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009. Am J Infect Control 37: 783-805.
- Swiontkowski MF, Hanel DP, Vedder NB, Schwappach JR (1999) A comparison of short and long term intravenous antibiotic therapy in the postoperative management of adult osteomyelitis. J Bone Joint Surg Br 81: 1046-1050.
- Bernard L, Dinh A, Ghout I, Simo D, Zeller V, et al. (2015) Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet 385: 875-882.
- Roblot F, Besnier JM, Juhel L, Vidal C, Ragot S, et al. (2007) Optimal Duration of Antibiotic Therapy in Vertebral Osteomyelitis. Semin Arthritis Rheum 36: 269-277.
- Tande AJ, Patel R (2014) Prosthetic Joint Infection. Clin Microbiol Rev 27: 302-345.
- Ariza J, Pujol M, Cabo J, Peña C, Fernandez N, et al. (1999) Vancomycin in surgical infections due to meticillin-resistant Staphylococcus aureus with heterogeneous resistance to vancomycin. Lancet 353: 1587-1588.
- Lazzarini L, Lipsky BA, Mader JT (2005) Antibiotic treatment of osteomyelitis: what have we learned from 30 years of clinical trials? Intern J Infect Dis 9: 127-138.
- Rüedi TP, Murphy WM, Colton CL, Dell’Oca AF, Holz U, et al. (2000) AO Principles of Fracture Management. AO Publishing.
- Mader JT, Mark S, Calhoun H (1997) Staging and staging application in osteomyelitis. Clinical Infectious Disease 25: 1303-1309.
- Parsons B, Strauss E (2004) Surgical management of chronic osteomyelitis. Am J Surg188: 57S-66S.
- Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ (2002) The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 23: 177-182.
- Lew DP, Waldvogel FA (2004) Osteomyelitis. Lancet 364: 369-379.
- Oliveira GA, Dell’Aquila AM, Masiero RL, Levy CE, Gomes MS, et al. (2001) Isolation in Brazil of nosocomial Staphylococcus aureus with reduced susceptibility to vancomycin. Infect Control Hosp Epidemiol 22: 443-448.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 4259
- [From(publication date):
February-2017 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 3532
- PDF downloads : 727