The Use of Subepithelial Connective Tissue Graft Technique to the Treatment of Class I Miller Recession in Lower Tooth with Abrasion: Case Report
Received: 15-Nov-2017 / Accepted Date: 02-Dec-2017 / Published Date: 09-Dec-2017 DOI: 10.4172/2376-032X.1000218
Abstract
Gingival recession can cause aesthetic problems, discomfort for cervical dentin hypersensitivity and can be treated by connective tissue grafts. This case report used subepithelial connective tissue graft to treatment class I Miller recession in premolar lower with abrasion. The premolar were treated by scaling and root planing chemical modification with 24% ethylenediaminetetraacetic acid (EDTA), bur shaped reconteur of abrasion lesion and subepithelial connective tissue graft combined with coronal flap. The results provide excellent root coverage, improve the root hypersensitivity and abrasion lesion. Although the longevity of this successful treatment depends on the diagnosis and removal of the causative agent, as well as the patient's cooperation in maintained of oral hygiene.
Keywords: Periodontal; Abrasion; Hypersensitivity; Cervical
Introduction
Gingival recession is defined as apical migration of the junctional epithelium [1], occasioned exposure of root surfaces and can be localized or generalized. It should bring on hypersensitivity of the teeth and esthetics problems and also may retain dental plaque, which can cause root caries [2,3].
Gingival recession had classified by Miller [4] which predict the success of root coverage treatment in isolated Miller Class I recession based on absence of bone loss in local areas with apical migration that does not reach mucogingival junction [4].
Periodontal plastic surgical procedures aim to protect and maintain the patient's oral health over his lifetime for adequate function as well as esthetic appearance [5]. Subepithelial connective tissue grafts has been used to the treatment of gingival recession and can improved the high and width of the keratinized tissue providing satisfactory esthetic results for root coverage and it has been indicated in areas with cervical abrasions [3,6-9].
Erosion or abrasion is a common lesion that has founded in cervical areas of tooth. It have been describes a theoretical process according to occlusal forces create stresses in enamel and dentin along the cervical area and predispose it to erosion and abrasion, also bruxism may be the primary cause of angled notches at the CEJ [10]. The role of toothbrush abrasion has been discussed in the etiology of abrasion [10,11].
The purpose of this article is to report the use tissue graft technique combined with the coronally flap on a treatment of Miller Class I gingival recessions associated with abrasions in lower premolar.
Case Presentation
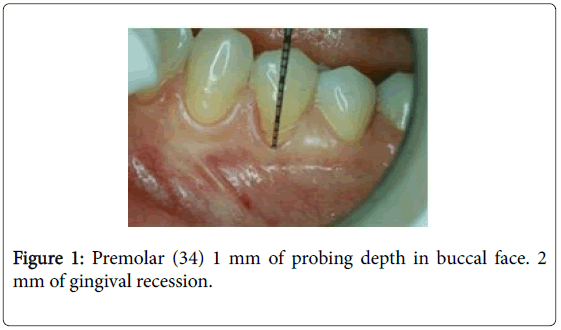
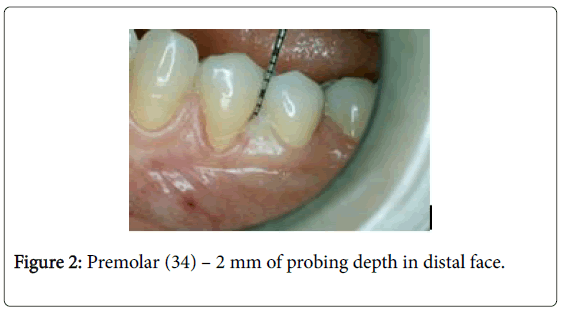
A healthy 18-year-old girl presented with a chief complaint of a hypersensibility in buccal face of lower premolar [10]. A periodontal examination performed reveal 1 mm and 2 mm of probing depth in buccal and distal faces respectively and 2 mm of gingival recession on buccal face with abrasion lesion (Figures 1 and 2) classified as Miller class I.
The gingival line in the mandibular third sextant was found to be thinner width of attached gingiva. Our treatment goal was to minimize gingival recession using subepithelial connective tissue grafts combined with the coronally positioned flap. A thorough extraoral and intraoral examination was performed.
Two treatment options were presented to the patient: subepithelial connective tissue grafts combined with the coronally positioned flap or restoration of Class V lesions with materials. After careful discussion, the patient opted for the subepithelial connective tissue grafts, she reported that she wanted to reestablished gingival margin; she did repeated restorations and generally lost it, each changes restorations she lost a moderate amounts of the remaining tooth structure.
A written informed consent was taken and the patient was instructed about post-surgical complications such as possible pain, post-operative bruising and extraoral swelling.
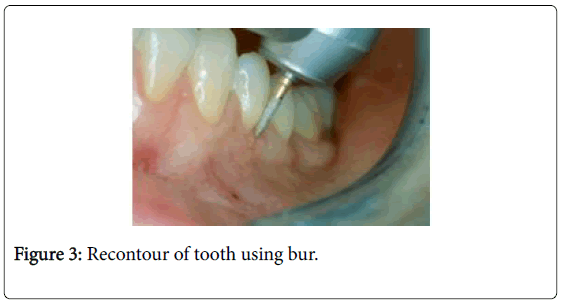
Premedication was used to prepare the patient for anaesthesia and to help provide optimal conditions for surgery. It was administration of antiinflamatory drugs (dexamethasone – 4 mg) unic dosage, 1 hour before surgery. Local anesthetic (Mepivacaine with 1:100.000 adrenalines) was administered in receptor and donor sites. Receptor site were treated by scaling and root planing with Gracey currets and 24% ethylenediaminetetraacetic acid (EDTA) gel application for 2 min, followed by washing with saline solution to chemical modification of the root surface. The bur was used to give new shape to the abrasion lesions in cervical face (Figure 3).
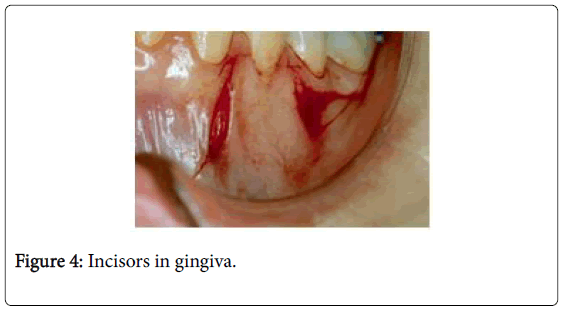
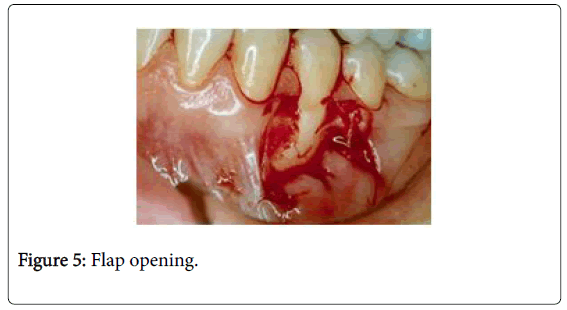
An intrasulcular incision was given on the buccal aspect of the involved tooth. A horizontal right angle incision was then made into the adjacent interdental papilla at or slightly coronal to the level of the cemento-enamel junction (CEJ) of the tooth presenting the defect.
Two divergent vertical incisions were given starting at least 0.5 mm from the gingival margin of the adjacent teeth and extending into the alveolar mucosa. The intrasulcular, horizontal right angle incision and the vertical incisions were connected and a trapezoidal full-thickness flap was raised 3-4 mm apical; from there, a partial-thickness dissection was then performed apically to allow for coronal positioning of the flap [12] (Figures 4 and 5).
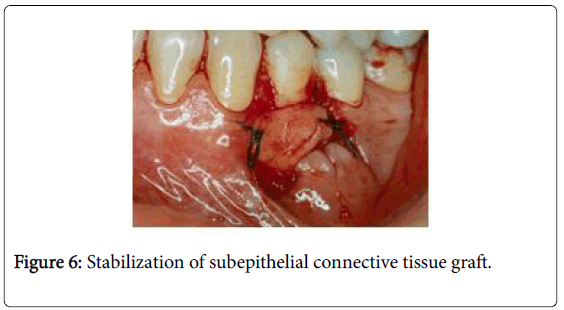
The preparation of the recipient site included the de-epithelization of the papillae adjacent to the defect. Donor site preparation of subepithelial connective tissue graft were prepared from 1.5-2.0 mm from the palate using a no. 15 scalpel blade.
The graft was placed over the recipient site such that its coronal margin was located at the CEJ and its apical margin at least 3.0 mm apically beyond the base of the defect [12] (Figure 6).
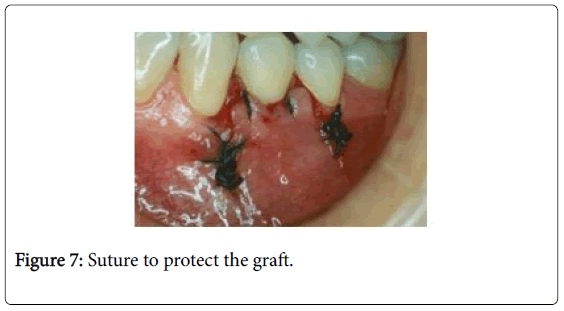
Coronal advancement of the partial-thickness flap was done so as to completely cover the graft without tension. The coronally positioned flap was secured in position by independent sling sutures using 4-0 seda sutures [12] (Figure 7).
Independent interrupted sutures were placed along the vertical incision line for close approximation.The gauze was moistened with saline and performed compression for 5 minutes in the donor area to improve the adaptation of the graft.
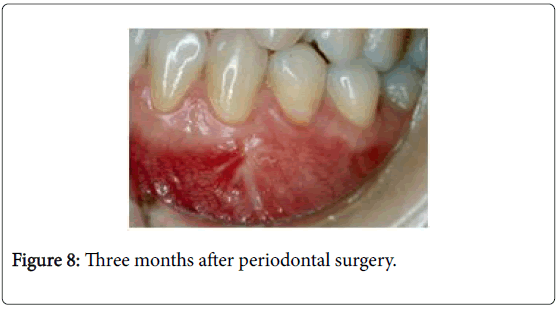
Post-operative instructions included soft diet, limited facial movements, no brushing around the surgical site for 14 days were explained [12]. The patient was instructed to rinse gently with 0.2% chlorhexidine gluconate twice daily for 2 weeks. Postoperative pain control was done with 750 mg of paracetamol during 6/6 hours for 2 days. Sutures were removed 1 week later. Occusal adjustments were performece to eleminate forces that result in flexure and failure of enamel and dentin [10]. After 4 weeks, the patients were instructed in mechanical plaque control and were included in oral hygiene program with visits scheduled once a month during 3 months (Figure 8).
Discussion
Get a predictable level of root coverage has been a goal of periodontal therapy, although some points need to be discussed to achieve this goal. This case reported purpose to use subepithelial connective tissue graft combined with coronal flap to treat class I Miller recession in premolar lower with abrasion. The technique was effective to root coverage and resolve root hypersensitivity and abrasion lesion.
Connective tissue grafts are considered the gold standard for root coverage and it demonstrated the highest success rates with the greatest amount of predictability [13,14]. Wennström [15] in 1996 reported an average of root coverage using connective tissue graft is 89% ranging over 50%-98%. The present case report shows the use of subepithelial tissue graft combined with coronally flap to the treatment of premolar area where it had thin gingiva biotype.
Mutthineni et al. [5] reported that the vitality and high survival potential of subepithelial connective tissue graft are achieved by sources of the blood supply from the gingival flap. In this case coronally flap combined with subepithelial gingival graft provide blood supply and protected the graft. Advantages were recorded by used of coronally flap, the connective tissue was not exposed, and healing was not affected and was predictable. There was a chance for graft epithelium and flap epithelium to heal by primary intention. Only disadvantage of this technique was pain and discomfort of a donor site [16].
In spite of gingiva biotype, Kao et al. [17], Mutthineni et al. [5] and Hoeppner et al. [18] reported that tissue biotype can affected the aesthetic outcomes. Kao et al. [17] reported that thin and thick gingiva tissue and concluded that thicker tissue is relative better to influence the tissue quality during restorative procedures. In this study, after 3 months periodontal therapy improved thick tissue after root coverage in class I Miller recession and were efficient to eliminate the root hypersensitivity.
The purpose of the EDTA conditioning, in this study, was to demineralize the root and removal of smear layer produced due to instrumentation to facilitate fibroblast adhesion and locomotion by collagen exposure [19,20]. The in vitro and in vivo effects of EDTA root biomodification are not consistent evident [20,21].
The abrasion lesion suggests that they could be caused by multifactorial etiology. Abrahamsen [22] suggested that toothbrush abrasion replaced with toothpaste abuse is abrasive enough to cause this type of damage. Shetty et al. [23] suggested that cervical lesions should demonstrated abfraction lesions present primarily at the cervical region of the dentition and are typically wedge-shaped, with sharp internal and external line angles. Subgingival lesions have also been observed.
In theory, the shape and size of the lesion are dictated by the direction, magnitude, frequency, duration and location of forces that arise when teeth come in contact [23]. Abfraction is postulated to be responsible for chronic sensitivity of the teeth to cold foods and liquids [10,24,25]. In this case report, the abrasion area was compatible with abfraction, so we also have been proposed occlusal adjustments and altering toothbrushing techniques.
Oral hygiene program improve stability of periodontal tissue are important to the longevity of the periodontal treatment. Zucchelli and De Sanctis [26] reported the successful root coverage results obtained with the coronally advanced flap for multiple recession defects were well maintained over the 4-year observation period.
The authors suggest negative patient characteristics such as a lack of compliance with a supportive care program and individual susceptibility to gingival recession were significantly associated with the recurrence in gingival recession.
This study accompanied the healing during 3 months and included patient hygiene program to preserve the root coverage [26].
This report is simple case reports of the use of the subepithelial connective tissue graft that can help clinical dentistry indicate surgical procedures and periodontal maintenance.
Conclusion
Based on this case reported the subepithelial connective tissue graft associated with coronally repositioned flap provides an excellent root coverage in case of gingival recessions with abrasion lesion and improved the root hypersensitivity.
References
- Agarwal K, Chandra C, Agarwal K, Kumar N (2013) Lateral sliding bridge flap technique along with platelet rich fibrin and guided tissue regeneration for root coverage. J Indian Soc Periodontol 17: 801-805.
- Do T, Dame-Teixeira N, Naginyte M, Marsh PD (2017) Root surface biofilms and caries. Monogr Oral Sci 26: 26-34.
- Kassab MM, Cohen RE (2003) The etiology and prevalence of gingival recession. J Am Dent Assoc 134: 220-225.
- Miller PD (1985) A classification of marginal tissue recession. Int J Periodontics Restorative Dent 5: 8-13.
- Mutthineni RB, Dudala RB, Ramisetty A (2014) Esthetic root coverage with double papillary subepithelial connective tissue graft: A case report. Case Rep Dent 2014: 509319.
- Borghetti A, Louise F (1994) Controlled clinical evaluation of the subpedicle connective tissue graft for the coverage of gingival recession. J Periodontol Dec 65: 1107-1112.
- Borghetti A, Glise JM, Monnet-Corti V, Dejou J (1999) Comparative clinical study of a bioabsorbable membrane and subepithelial connective tissue graft in the treatment of human gingival recession. J Periodontol 70: 123-130.
- Bouchard P, Etienne D, Ouhayoun JP, Nilvéus R (1994) Subepithelial connective tissue grafts in the treatment of gingival recessions: A comparative study of 2 procedures. J Periodontol 65: 929-936.
- Deliberador TM, Martins TM, Furlaneto FA, Klingenfuss M, Bosco AF (2012) Use of the connective tissue graft for the coverage of composite resin-restored root surfaces in maxillary central incisors. Quintessence Int 43: 597-602.
- Sarode GS, Sarode SC (2013) Abfraction: A review. J Oral Maxillofac Pathol 17: 222-227.
- Naik VK, Jacob CA, Nainar DA (2016) Assessment of non-carious root surface defects in areas of gingival recession: A descriptive study. J Clin Exp Dent 8: e397-e402.
- Kumar GN, Murthy KR (2013) A comparative evaluation of subepithelial connective tissue graft (SCTG) versus platelet concentrate graft (PCG) in the treatment of gingival recession using coronally advanced flap technique: A 12-month study. J Indian Soc Periodontol 17: 771-776.
- Sculean A, Cosgarea R, Katsaros C, Arweiler NB, Miron RJ, et al. (2017) Treatment of single and multiple Miller Class I and III gingival recessions at crown-restored teeth in maxillary esthetic areas. Quintessence Int 48: 777-782.
- Shanmugam M, Sivakumar V, Anitha V, Sivakumar B (2012) Clinical evaluation of alloderm for root coverage and colour match. J Indian Soc Periodontol 16: 218-223.
- Wennström JL (1996) Mucogingival therapy. Ann Periodontol 1: 671-701.
- Ramakrishnan T, Kaur M, Aggarwal K (2011) Root coverage using epithelial embossed connective tissue graft. Indian J Dent Res 22: 726-728.
- Kao RT, Pasquinelli K (2002) Thick vs. thin gingival tissue: A key determinant in tissue response to disease and restorative treatment. J Calif Dent Assoc 30: 521-526.
- Hoeppner MG, Fonseca RB, Pfau EA, Justo FR, Favero A, et al. (2011) Rehabilitation of periodontally compromised teeth with fiber-reinforced composite resin: a case report. Quintessence Int 42: 113-120.
- Girotra N, Vandana KL (2014) Fluorosed fibroblast attachment on fluorosed and nonfluorosed teeth after SRP and EDTA root biomodification. J Indian Soc Periodontol 18: 26-31.
- Blomlof L, Bergman E, Forsgardh A, Foss L, Larsson A, et al. (2000) A clinical study of root surface conditioning with an EDTA gel. I. Nonsurgical periodontal treatment. Int J Periodontics Restorative Dent 20: 560-565.
- Mariotti A (2003) Efficacy of chemical root surface modifiers in the treatment of periodontal disease: A systematic review. Ann Periodontol 8: 205-226.
- Abrahamsen TC(2005) The worn dentition - pathognomonic patterns of abrasion and erosion. Int Dent J 55: 268-276.
- Shetty SM, Shetty RG, Mattigatti S, Managoli NA, Rairam SG, et al. (2013) No carious cervical lesions: Abfraction. J Int Oral Health 5: 143-146.
- Piotrowski BT, Gillette WB, Hancock EB (2001). Examining the prevalence and characteristics of abfraction like cervical lesions in a population of US veterans. J Am Dent Assoc 132: 1694-1701.
- Lee WC, Eakle WS (1994) Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent 52: 374-380.
- Zucchelli G, de Sanctis M (2005). Long-term outcome following treatment of multiple Miller class I and II recession defects in esthetic areas of the mouth. J Periodontol 76: 2286-2292.
Citation: Portero PP, Batista NC, Galhardo Camargo ACG, Poiate IAVP, da Cruz AD, et al. (2017) The Use of Subepithelial Connective Tissue Graft Technique to the Treatment of Class I Miller Recession in Lower Tooth with Abrasion: Case Report. J Interdiscipl Med Dent Sci 5: 218. DOI: 10.4172/2376-032X.1000218
Copyright: © 2017 Portero PP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5803
- [From(publication date): 0-2017 - Feb 26, 2025]
- Breakdown by view type
- HTML page views: 5030
- PDF downloads: 773