The Use of Living Cell Cartilage Matrix Grafts in the Management of Hallux Rgidus: A Case Series
Received: 01-Nov-2022 / Manuscript No. crfa-22-78649 / Editor assigned: 08-Nov-2022 / PreQC No. crfa-22-78649 / Reviewed: 16-Nov-2022 / QC No. crfa-22-78649 / Revised: 21-Nov-2022 / Manuscript No. crfa-22-78649 / Published Date: 30-Nov-2022
Abstract
Hallux rigidus, a condition defined by loss of motion in the first metatarsophalangeal joint and its subsequent progression to arthrosis, is well-documented in the clinical literature. Novel therapies for the management of this condition, such as living-cell cartilage matrix grafts, however, have not been thoroughly investigated. In this study, the authors present two distinct cases of individuals that refused an arthrodesis, but had cartilage damage requiring more than a cheilectomy. Both individuals at 24 months post-surgery remained asymptomatic, and happy with the outcome of their procedure.
Introduction
Hallux rigidus is a degenerative condition occurring in the first metatarsophalangeal (MTP) joint. This pathology presents as a limitation of motion in the first MTP joint which may result in apparent abnormalities in gait [1]. Both conservative and surgical management of hallux rigidus has been thoroughly described in the literature [1-3]. Well-established methods of surgical treatment include joint sparing procedures such as a cheilectomy as well as joint sacrificing procedures such as an arthrodesis of the MTP joint. These interventions have both been shown to have long-term satisfactory patient outcomes [1-3]. Additional procedures, such as the use of silastic implants, have been cited as an effective form of treatment resulting in long-term relief of pain and improvement in range of motion, however, these forms of implants have been shown to sometimes result in subsidence surrounding the implant stem [4-5]. Additional complications such as lymphadenopathy have also been described as a possible complication of silastic implants [6-8]. More recently, an alternative form of treatment using polyvinyl alcohol (PVA) hydrogel implants has been found to be successful in the management of hallux rigidus, however these implants, require the boring of a large hole in the metatarsal head [9]. Similar to previous types of surgical interventions, patients who received PVA hydrogel implants were noted to have an overall improvement of pain and range of motion without the limitations of shoe gear as seen with fusions [9].
A newer alternative to addressing hallux rigidus pain is the use of living-cell, intact, cartilage matrix grafts, such as Prochondrix. These grafts utilize metabolically activated cells to restore the cartilage bridge between subchondral bone and the articular surface. Unlike the PVA hydrogel implants, no large boring of the metatarsal head is required. Additionally the graft is replaced by the host’s own cellular tissue in approximately 18 months [10].
To the best of the authors’ knowledge, very limited data is available for the use of living-cell cartilage matrix grafts, such as Prochondrix, in the management of hallux rigidus. In this study, we present two cases of individuals with moderate arthrosis and hallux rigidus. In both cases, the patients elected to proceed with Prochondrix implants. Each patient exhibited favorable results for 24 months after the procedure.
CASE 1
A 59 year old female with no significant past medical history presented with a chief complaint of worsening pain in the left first metatarsophalangeal joint that was improved by NSAIDs. The described pain o Ik f a “dull ache” had become more constant over the preceding year. The patient had minimal improvement from changes to shoe gear and the use of orthotics. She had presented to another foot and ankle specialist and was advised that she had a “bone in her joint” and would need surgery to remove the bone and fuse the joint. The patient did not want a fusion as it would limit her shoe gear for work, so she sought a second opinion.
A clinical examination revealed the patient had less than 5 degrees of dorsiflexion with pain through approximately 50% of the range of motion. X-rays revealed joint space narrowing, and a prominent dorsal exostosis with what appeared to be fractured osteophytes that had advanced into the first metatarsophalangeal joint blocking range of motion. A high resolution cone beam computed tomography (CBCT) scan of the left foot not only confirmed these findings (Figure 3 A), but also revealed findings suggestive of an osteochondral defect in the dorsal aspect of the left first metatarsal. These findings were discussed with the patient. Conservative measures were continued for 8 weeks with no improvement. The patient elected to undergo surgical intervention for her condition.
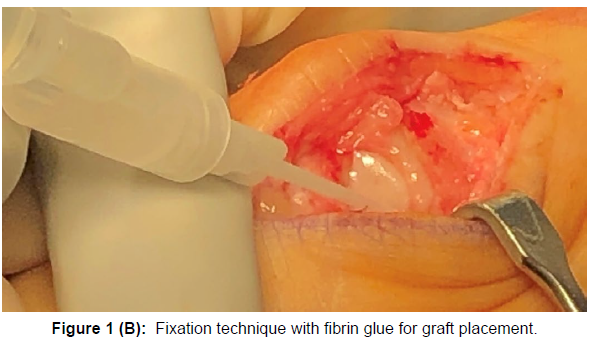
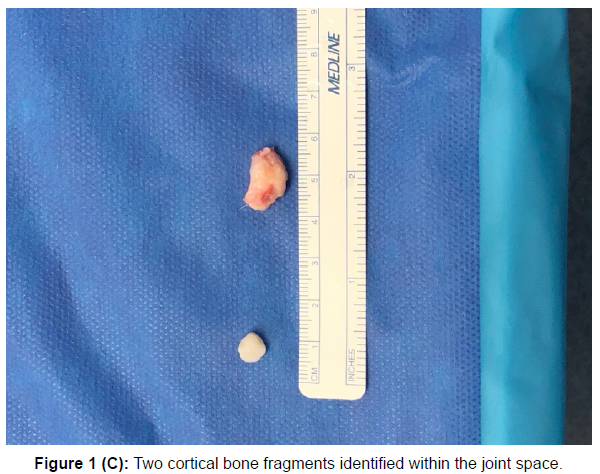
A linear incision was made over the dorsal aspect of the left first metatarsophalangeal joint just medial to the extensor hallucis longus tendon (Figure 1A). Two bone fragments (Figure 1C) were identified and extracted, measuring approximately 1cm and 2cm respectively. A cheilectomy was then performed and dorsiflexion assessed to be approximately 35 degrees. An irregular shaped osteochondral defect was observed. The lesion was gently debrided with a 2mm curette, followed by fenestration of the base of the lesion with a 0.045 k-wire. Using a Prochondrix 8mm graft, a size and shape congruent to the defect was created and affixed with fibrin glue (Figure 1B). The area was gently irrigated and the joint inspected to make sure the graft was congruent to the OCD appreciated prior to graft placement (Figure 1D). The surgical site was then closed with absorbable sutures. There was minimal pain and swelling after the surgery which resolved within 3 days. The patient was placed in a CAM walker for 2 weeks and transitioned to a surgical shoe for 2 weeks. The patient was allowed to return to a rigid soled shoe at one month. She returned to full activity (running and aggressive exercise) 2 months after the surgery.
At the patient’s 2 month follow up visit it was noted that the pain present before the surgery had completely resolved. The patient continued to be pain free at 6, 12, 18, and 24 months postoperatively, maintaining approximately 35 degrees of dorsiflexion of the left hallux.
CASE 2
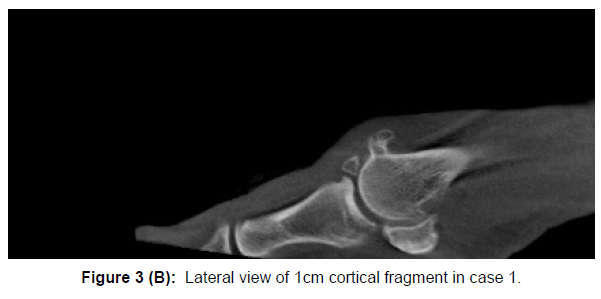
A 52 year old female presented with a chief complaint of pain in the left big toe joint that had been present and worsening over the course of several years. The patient had received a series of steroid injections in the left first metatarsophalangeal joint that only provided temporary pain relief. Orthotics improved the pain, but the dull ache continued even with the use of orthotics (Figure 3B). After exhausting all conservative measures the patient elected to undergo surgical intervention for the management of her condition. The patient refused a joint fusion. On a preoperative clinical exam, the patient had approximately 5 degrees of dorsiflexion with pain on the end range of motion (dorsiflexion) only. Plain film radiographs revealed the presence of a broken osteophyte within the joint. CBCT confirmed the presence of an osteochondral defect on the head of the left first metatarsal bone (Figure 3C).
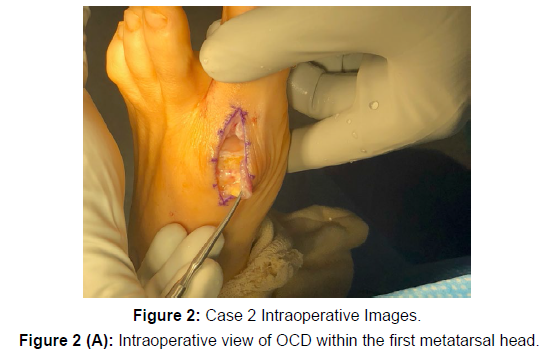
Congruent to the procedure described in Case 1, a cheilectomy was performed after extraction of a 1cm osteophyte revealing an osteochondral defect (Figure 2A). The range of dorsiflexion was confirmed to be 40 degrees. An 8mm Prochondrix graft was then applied to fenestrated bone after curettage of the perimeter of the chondral defect (Figure 2B). The graft was affixed with fibrin glue, the area irrigated, and then closed. The patient noted minimal pain after the procedure. The patient was placed in a CAM walker for 2 weeks and then converted to a surgical shoe for 2 weeks. A shoe with a rigid sole was permitted at 1 month. The patient returned to regular physical activity including running and intense exercise at approximately 2 months after surgery noting resolution of the preoperative pain. The patient continued to show resolution of pain with 40 degrees of dorsiflexion at 6, 12, 18 and 24 months after the procedure.
Discussion
We noted improvement in overall range of motion in both cases 1 and 2 consistent with the findings of the current literature. Although the patients did not acquire the full range of motion at the first MTPJ, we did note resolution of pain after surgical intervention. In both cases, the removal of large osteophytes could have contributed at least partly to the resolution of pain as well as the improvement in range of motion. We feel addressing the large osteochondral defect was of equal importance in the improvement of symptoms.
Similar to the findings of Cansecco et al, our patients exhibited improvement of gait although normal range of motion at the first MTPJ was not achieved [11]. Harrison et al, utilizing the Manchester- Oxford Foot and Ankle Questionnaire (MOXFQ) also demonstrated an improvement of gait and pain scores from the cheilectomy procedure without restoring full range of motion [12]. Unlike the findings of these two studies, our patients exhibited complete resolution of pain. This finding could be contributed to the use of a living-cell cartilage matrix implant to address cartilage loss within the joint, suggesting that a cheilectomy alone will not be sufficient to address symptomatic patients with the known presence of an osteochondral defect.
Conclusion
The advancements in medical technology for the surgical management of hallux rigidus are constantly evolving. More novel, less invasive techniques, such as Prochondrix, should be considered when devising a treatment plan for the surgical management of patients with hallux rigidus and a known or suspected osteochondral defect. It is the hope of the authors of this paper to present two incidences of successful surgical management of hallux rigidus and therefore increase awareness of a new joint sparing surgical alternative. Although our study was limited by the number of subjects, we feel it presents a novel therapeutic alternative to the current joint sparing techniques with practically no need of explantation due to graft resorption. Further research with a greater number of subjects is necessary to thoroughly evaluate the efficacy of this tool in the management of a very common condition.
Conflict of Interest
The authors of this paper have not received any financial support or dividends regarding the clinical outcomes of this study.
References
- Coughlin MJ, Shurnas PS (2003) Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am 85(11): 2072-2088.
- Chraim M, Bock P, Alrabai HM, Trnka HJ (2016) Long-term outcome of first metatarsophalangeal joint fusion in the treatment of severe hallux rigidus. Int Orthop 40(11): 2401-2408.
- Kumar S, Pradhan R, Rosenfeld PF (2010) First metatarsophalangeal arthrodesis using a dorsal plate and a compression screw. Foot Ankle Int 31(9): 797-801.
- Morgan S, Ng A, Clough T (2012) The long-term outcome of silastic implant arthroplasty of the first metatarsophalangeal joint: a retrospective analysis of one hundred and eight feet. Int Orthop36(9): 1865-1869.
- Shereff MJ, Jahss MH (1980) Complications of silastic implants arthroplasty in the hallux. Foot Ankle 1(2): 95-101.
- Cracchiolo A, Weltmer JB, Lian G, Dalseth T, Dorey F (1992) Arthroplasty of the first metatarsophalangeal joint with a double-stem silicone implant: results in patients who have degenerative joint disease failure of previous operations, or rheumatoid arthritis. J Bone Joint Surg 74: 552-563.
- McNearney T, Haque A, Wen J, Lisse J (1996) Inguinal lymph node foreign body granulomas after placement of a silicone rubber (Silflex) implant of the first metatarsophalangeal joint. J Rheumatol 23: 1449-1452.
- Sammarco GJ, Tabatowski K (1992) Silicone lymphadenopathy associated with failed prosthesis of the hallux: a case report and literature review. Foot Ankle 13: 273-276.
- Eble SK, Hansen OB, Chrea B (2020) Clinical Outcomes of the Polyvinyl Alcohol (PVA) Hydrogel Implant for Hallux Rigidus. Foot Ankle Int 41(9): 1056-1064.
- Geraghty S, Kuang J, Yoo D, LeRoux-Williams M, Vangsness CT Jr et al. (2015) A novel, cryopreserved, viable osteochondral allograft designed to augment marrow stimulation for articular cartilage repair. Journal of Orthopaedic Surgery and Research 20: 66-75.
- Canseco K, Long J, Marks R, Khazzam M, Harris G (2009) Quantitative motion analysis in patients with hallux rigidus before and after cheilectomy. J Orthop Res 27(1):128-134.
- Harrison T, Fawzy E, Dinah F, Palmer S (2010) Prospective assessment of dorsal cheilectomy for hallux rigidus using a patient reported outcome score. J Foot Ankle Surg 49(3): 232-237.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Adrian Wright J, Julia Tanaka BA, Jacob Breitkopf BS (2022) The Use of Living Cell Cartilage Matrix Grafts in the Management of Hallux Rigidus: A Case Series. Clin Res Foot Ankle, 10: 376.
Copyright: © 2022 Adrian Wright J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1577
- [From(publication date): 0-2022 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 1237
- PDF downloads: 340