Case Report Open Access
The Use of a Dental Dam during Implant Placement A Novel Case Report and Review
Tory S*
DDS, MSD, MSHPE, Loma Linda University, USA
- *Corresponding Author:
- Tory S
DDS, MSD, MSHPE
Loma Linda University, USA
Tel: +1 909-558-400
E-mail: tsilvestrin@llu.edu
Received date June 18, 2016; Accepted date June 29, 2016; Published date July 01, 2016
Citation: Tory S (2016) The Use of a Dental Dam during Implant Placement – A Novel Case Report and Review. Dent Implants Dentures 1:109. doi:10.4172/2572-4835.1000109
Copyright: © 2016 Tory S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Dental Science and Medicine
Abstract
Background: It is beneficial to reduce the ingestion/aspiration of dental instruments during implant placement. It may be beneficial to reduce the bacterial load during implant placement procedures, as biofilm formation on implants can lead to failure. A dental dam may help reduce ingress of oral bacteria during implant placement. Case Description: This case report demonstrates the use of a dental dam during the surgical placement of a dental implant. A literature review is presented that includes a history and rationale for the use of dental dams during various dental procedures. It also reviews the risks of aspirating/ingesting implant instruments. Practical Implications: Use of a dental dam during implant placement offers operator conveniences, while also providing a safer field with less chance of instrument swallowing and may offer a less bacteria-laden operating field.
Keywords
Dental implants; Endodontics; Endodontic files; Emergencies; Dental dam
Introduction
In 1864 Dr. Sanford C. Barnum introduced rubber dams* to dentistry [1]. Dental dam isolation is accepted as a standard procedure during endodontic treatment and has been endorsed by many professional organizations including the American Association of Endodontists [2], the European Society of Endodontology [3], and the American Academy of Pediatric Dentistry [4]. In a recent ADA News interview with former AAE President Gerald Glickman, the importance of the use of dental dam during endodontic treatment was emphasized [5].
Despite its acceptance in endodontic and other dental disciplines, the use of dental dam is not mentioned in dental implant literature [6]. The benefits in endodontic would be expected to also apply during implant placement: improved visualization and reduced risk of ingestion or aspiration of irrigation solutions and small instruments. Additional benefits would include improved view of the operating field by retraction of soft tissues and enhanced visual contrast, and patients are also better able to keep their mouths open during treatment [7,8].
Case Report
A 60 year-old female patient presented with the chief complaint of a missing tooth that she wanted to have replaced with an implant. She was taking no medications, did not have any known allergies, and had a noncontributory health history. She presented with a nearly full complement of teeth that were in good condition. She was missing her left mandibular second premolar and her left mandibular first molar (#19). A supernumerary premolar occupied the space of the missing molar. The missing left mandibular second premolar had been extracted 20 years earlier due to extensive caries.
The alveolar bone in the extraction site had resorbed and left a marginally compromised horizontal dimension including a buccal concavity. Cone-beam computed tomography (CBCT) however, revealed adequate horizontal (both bucco-lingual and mesio-distal) and vertical bony dimensions to allow for endosseous implant placement. Adequate keratinized tissue was present for the planned procedure. All the risks, benefits, costs and alternative treatments were discussed and the patient approved the treatment plan and signed the consent. The referring dentist had provided a surgical stent stored in 0.12% chlorhexidine gluconate (Peridex®, Zila Pharmaceuticals, USA) allowing for a prosthetically driven implant placement. The stent had been fabricated using a computer aided surgical guide providing a guide tube for proper three-dimensional placement of the implant (Simplant, Dentsply, USA). The patient rinsed preoperatively for 90 seconds with Peridex and was prepared for surgery.
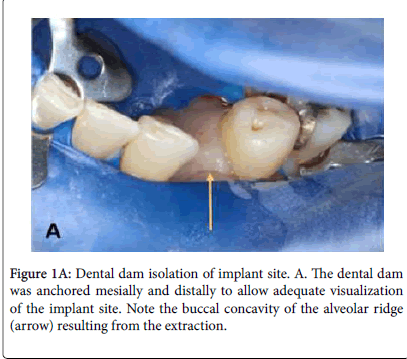
After 2 minutes’ application of topical 5% benzocaine, 3.4 mL 2% lidocaine (Xylocaine, International Medication Systems Limited) with 1:100,000 epinephrine was infiltrated buccally and lingually to the surgery site. A disinfected non-latex dental dam (soaked for 5 minutes in 5.25% sodium hypochlorite and then rinsed with sterile saline) was placed in a split-dam format extending from the supernumerary premolar to the ipsilateral mandibular incisors and secured with #0 clamps (Figure 1A). A rotary soft tissue punch (Rotary Tissue Punch for Latch Type Handpieces, Salvin, USA) was used in a slow-speed handpiece to expose the crestal bone. Tissue remnants were curetted with a spoon excavator. The implant placement was done as a flapless procedure.
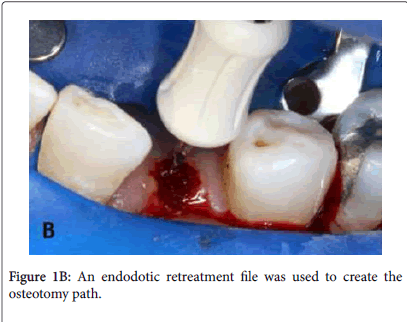
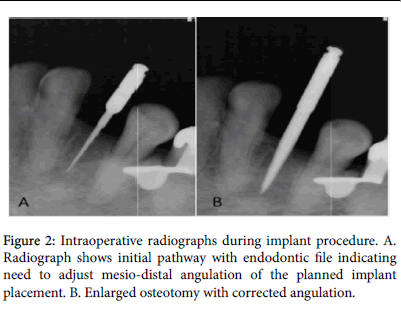
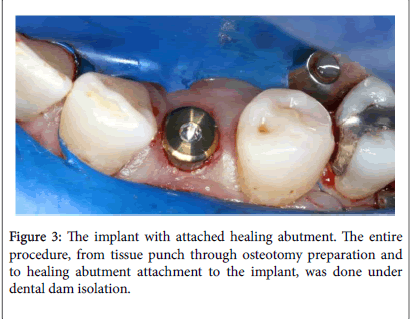
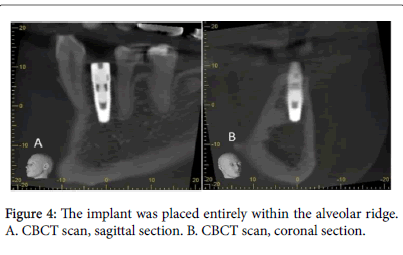
A ProTaper D1 (Tulsa Dental Specialties, USA) retreatment file was used to create the initial pathway into the bone (Figure 1B). A radiograph was taken of the file (Figure 2A) and it revealed the need to redirect the angulation in the mesio-distal plane to properly localize the osteotomy. At this point, use of the guide was discontinued due to the improper angulation and the rest of the procedure was completed without the use of the guide. A pilot drill (Nobel Biocare, Switzerland) was then used to enlarge the properly angulated pathway (Figure 2B) following which the osteotomy was completed to allow placement of a 4.3 x 11.5 mm Nobel Select Replace implant (Nobel Biocare, Switzerland). The implant was placed with a hand torque driver to 35 Ncm and a healing abutment was hand tightened. A clinical view of the implant in place with the cover screw attached and the site still isolated with the dental dam can is shown in Figure 3. The implant was placed completely within the bony envelope, as can be seen in the postoperative CBCT scan (Figure 4A and 4B).
Prescriptions for the postoperative care included 21 tabs 500 mg amoxicillin (t.i.d. for 7 days), 10 tabs 5/325 mg hydrocodone/ acetaminophen (Norco, Watson Pharmaceuticals, USA) 1-2 tabs every 6 hours as needed for pain, and one bottle Peridex® to rinse the mouth with one capful twice daily for 2 weeks. The postoperative evaluation showed satisfactory healing and no adverse signs or symptoms.
Discussion
Benefits of dental dams
Use of a dental dam provides infection control by decreasing bacterial and viral laden aerosols [9]. Failure to use a dam during nonsurgical endodontic procedures can result in aspiration or ingestion of dropped dental instruments with subsequent medical problems [9].
Oral microorganisms play an essential role in the pathogenesis of apical periodontitis [10,11] a concept universally accepted in endodontics. It is also recognized in other disciplines. Goldfein et al. evaluated the outcomes in patients who had posts placed either with or without use of a dental dam and the success rate was 20% lower in the group without dental dam versus the group with dental dam; the difference was statistically significant [12]. Apparently bacteria can, through salivary contamination, infect canal spaces even in the short periods of time during post placement and affect the treatment outcome. Could the same be true during placement of dental implants?
Dental implants are susceptible to oral biofilm, similarly to teeth in periodontal disease [13]. The presence of bacterial lipopolysaccharide and bacterial biofilms lead to periimplant mucositis and periimplantitis [13]. Reducing the bacterial load in the surgical field appears to be beneficial because bacteria are able to form biofilms on the surface of many implant materials and that can lead to implant failures [14-16].
A recent report on the effect of dental dam usage on the survival of 517,234 endodontically treated teeth showed that after a mean observation period of 3.43 years, teeth treated with dental dam isolation had a higher survival probability (90.3%) than those treated without (88.8%) [17]. Given the large sample size the difference is statistically significant.
Others have also provided data about outcomes from clinical procedures completed with or without the use of dam isolation [18,19] de Lourdes Rodrigues Accorinte et al. evaluated histologically the inflammatory response of human pulp-capped teeth when dental dams or cotton rolls were used for isolation [18]. They found more severe inflammation when cotton rolls were used compared to dental dam isolation. van Nieuwenhuysen et al. found that retreatment outcomes were significantly improved in teeth isolated with a dental dam compared with cotton roll isolation [19]. Possibly, difficulty in using a dental dam as well as the location of the treated tooth may have played a role in choosing a dental dam or cotton rolls. An interesting study from Australia showed that continued pain after root canal treatment was less frequent in patients when dental dam was used versus not used [20].
Confidence in the protective benefits of the dental dam may be one explanation why dentists who frequently use dental dam also use higher concentrations of sodium hypochlorite and more often use ethylene diamine tetraacetic acid (EDTA) compared to dentist who do not [21,22].
Prevalence of dental dam usage
Dental dam usage during endodontic and restorative procedures is widely taught in dental schools [23]. When dental students were polled regarding their plans about using dental dam after graduation, 100% predicted using it for endodontic therapy in adults and 98.5% predicted using it for endodontic treatment in children [24]. Despite learning to use dental dams during root canal treatment and expecting to routinely use dental dams after graduation, the rates of its use among dental school graduates are significantly lower in practice [24-26].
A recent investigation found that only 44% of general dentists used a dental dam for all root canals procedures, 24% used it 51-99% of the time, 17% used it less than 50% of the time and 15% never used it [26]. Another survey found 11% of general dentists never used dental dam during root canal treatment and only 58% used it for every root canal treatment [27]. Ireland described the poor rate of dental dam usage thus: “Probably no other technique, treatment, or instrument used in dentistry is so universally accepted and advocated by the recognized authorities and so ignored by the practicing dentists” [25].
The use of dental dam does not seem to be related to frequency or level of postgraduate training of general dentists [26,27]. The use of the dental dam also appears unrelated to the tooth being treated [28] or the gender of the dentist [29,30]. Interestingly, use of dental dam has been reported to be more frequent in group practices than solo practices, and also by dentists who received extensive undergraduate education in dental dam usage [22,26].
Common reasons for resistance to the use of a dental dam routinely include increased chair time necessary to apply the dam, lack of patient acceptance, insufficient training in its use leading to difficulty in its application, cost of equipment as well as no increase in treatment fees [9,31-33]. Ahmad proposed other secondary disincentives for dental dam usage: Patients and practitioners view the dental dam as unnecessary, taking radiographs is difficult, staff is unfamiliar with its use, patients have difficulty swallowing, communication with the patient is restricted, and lack of peer use of dental dams [7].
Avoiding the use of dental dam due to lack of patient acceptance has been challenged. Reuter noted that patients actually prefer the use of a dental dam for restorative procedures [34] and others have found that many patients prefer dams for dental treatment based on previous favorable experiences with them [35,36] Positive attitudes about dental dam usage by dentists and increased patient experience are major factors that could lead to increased acceptance [37].
Another negative view that dentists have about the use of dental dam is often expressed in terms of being a ‘waste of time’ rather than a valuable component of high quality dental treatment [24] The application of a dental dam takes mere minutes-even in the hands of an inexperienced clinician and the loss of time is compensated for by the many advantages inherent in the use of a dental dam, including increased visibility, decreased salivary contamination of the site, as well as retraction of soft tissues [34].
Use of dental dam during surgical implant placement
In this case report the use of a dental dam during the surgical placement of a dental implant provided convenient access to the surgical field, decreased the risk of aspiration or ingestion of a dropped instrument, and maintained a less contaminated environment. The dental dam did not present a problem during the exposure of treatment radiographs.
Use of a dental dam during implant placement does require the presence of proximal teeth for dental dam clamps. Further, a dental dam may not provide a fluid-tight osteotomy site – similar to that accomplished during endodontic procedures – but that problem can be addressed using a sealant such as OraSeal® Calk and Putty (Ultradent Products, South Jordan, UT) along the edges of the dam.
It has been pointed out that there are situations in which the use of a dental dam may not be feasible during a dental procedure [35]. Such a situation would be expected in an edentulous patient. If, however, the value of having a dam in place during the implant placement is important, one could consider providing dental dam clamp anchor by temporarily placing orthodontic mini screws in suitable alveolar ridge locations.
While one would expect improved implant outcomes by reducing bacterial contamination with dental dam isolation, no study could be found addressing this issue. The value of reducing the risk of accidental swallowing/aspiration of small instruments can be recognized in that such events would open the dentist to litigation as well as dealing with the economic cost to remedy the acute and long-standing issues attributed to an accident [37]. Recently, a patient sued her dentist after swallowing an untethered implant screwdriver that she was not able to regurgitate. In addition, the dentist failed to immediately refer the patient to a hospital emergency department and subsequent surgery to remove it required a week-long hospital stay [38]. Treatment related to aspiration or ingestion of a dental instrument can be very costly [39] so increasing the use of dental dams should help prevent the untoward occurrence of aspirated or ingested instruments [40].
In response to the complaint that it is time-consuming to place a dental dam, Cragg pointed out that the most time-consuming aspect about dental dam usage is the amount of time necessary to convince dentists to use it [1]. Many advantages exist and this case report presents an example of its use during surgical endosseous implant placement. Preventing complications can best be accomplished with routine use of a dental dam, but a throat screen when a dental dam is not possible and tethering floss through feasible dental instruments for retrieval if misplaced are alternative options [36]. As was highlighted by Heling and Heling, ‘Primum non nocere seeundum curare: First prevent further damage and then treat the initial problem’ [41]. This saying applies not only to the ethics of the dental profession as a whole, but also illustrates the driving principle behind the use of the dental dam.
Previous investigations have shown that regional infiltration anesthesia is as effective as nerve blocks for implant placement [42]. That type of anesthesia was used in this case, and the patient was comfortable throughout the procedure.
Periapical radiographs are often exposed intra-operatively to assess the direction of the osteotomy procedure. Both the osteotomy depth and its mesial-distal angulation can conveniently be evaluated using periapical exposures, but the facial-lingual position of the implant is not depicted adequately on two-dimensional periapical radiographs.
A postoperative CBCT scan was obtained to verify accurate alveolar bony housing of the implant. The value of postoperative CBCT scans must be weighed against the need to observe the principle of keeping patient radiation dose ‘As Low as Reasonably Achievable’ (ALARA) [43]. This principle was part of the pre-treatment planning and it was discussed with the patient.
Another unique procedure demonstrated in this case report was the use of an endodontic rotary file to create the initial osteotomy pathway. It served as the pilot drill allowing both the initial osteotomy and the final preparation to be done while conserving bone. It should be noted that use of the file in this manner is not in accord with manufacturer’s recommended use, but it provided a more conservative initial osteotomy than a typical implant pilot drill.
Conclusion
Dental dam isolation during surgical implant placement provides a clean operating field allowing clear visualization of the crystal alveolar bone and may prevent ingress of saliva and bacteria from contaminating the osteotomy site. It can also prevent aspiration or ingestion of small instruments.
Until recent decades, the dams were made from latex rubber, but have in recent years been changed to non-latex vinyl to prevent latex allergy reactions and are now more accurately referred to as ‘dental dams.’
References
- Cragg TK (1972) The use of rubber dam in endodontics. J Can Dent Assn 38: 376-377.
- (2010) American Association of Endodontists. AAE position statement: Dental dams.
- European Society of Endodontology. (2006) Quality guidelines for endodontic treatment: Consensus report of the European Society of Endodontology. IntEndod J 39: 921-930.
- American Academy of Pediatric Dentistry. (2014) Guideline on pulp therapy for primary and young permanent teeth. Reference Manual 37:244-252.
- Manchir M (2015) AAE reminder: Dental dams help ensure patient safety. ADA News.
- Schindler W (2008) Endodontic instruments and armamentarium. A. Dental dam and its application. In: Ingle's Endodontics. 6th ed. Ingle JI, Bakland LK, Baumgartner JC, editors. Shelton CT 791-799.
- Ahmad IA (2009) Rubber dam usage for endodontic treatment: a review. IntEndod J 42:963-972.
- Bhuva BCB, Patel S (2008) Rubber dam in clinical practice. EndodPract Today 2:131-141.
- Lynch CD, McConnell RJ (2007) Attitudes and use of rubber dam by Irish general dental practitioners. IntEndod J 40: 427-432.
- Paterson RC, Pountney SK (1987) The response of the dental pulp to mechanical exposure in gnotobiotic rats mono-infected with a strain of Streptococcus mutans. IntEndod J 20: 159-168.
- Kakehashi S, Stanley HR, Fitzgerald RJ (1965) The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol Oral Radiol 20: 340-349.
- Goldfein J, Speirs C, Finkelman M, Amato R (2013) Rubber dam use during post placement influences the success of root canal-treated teeth. J Endod 39:1481-1484.
- Buddula A (2013) Bacteria and dental implants: A review. J Dent Implants 3:58-61.
- Young MP, Korachi M, Carter DH, Worthington HV, McCord JF, et al. (2002) The effects of an immediately pre-surgical chlorhexidine oral rinse on the bacterial contaminants of bone debris collected during dental implant surgery. Clin Oral Implants Res 13:20-29.
- Hahnel S, Wieser A, Lang R, Rosentritt M (2015) Biofilm formation on the surface of modern implant abutment materials. Clin Oral Implants Res 26:1297-1301.
- Raval NC, Wadhwani CP, Jain S, Darveau RP (2015) The interaction of implant luting cements and oral bacteria linked to peri-implant disease: An in vitro analysis of planktonic and biofilm growth - a preliminary study. Clin Implant Dent Relat Res 17:1029-1035.
- Lin PY, Huang SH, Chang HJ, Chi LY (2014) The effect of rubber dam usage on the survival rate of teeth receiving initial root canal treatment: A nationwide population-based study. J Endod 40:1733-1737.
- de Lourdes Rodrigues Accorinte M, Reis A, DouradoLoguercio A, Cavalcanti de Araujo V, Muench A (2006) Influence of rubber dam isolation on human pulp responses after capping with calcium hydroxide and an adhesive system. Quintessence Int 37: 205-212.
- van Nieuwenhuysen JP, Aouar M, D'Hoore W (1994) Retreatment or radiographic monitoring in endodontics. IntEndod J 27: 75-81.
- Abbott PV (1994) Factors associated with continuing pain in endodontics. Aust Dent J 39:157-161.
- Saunders WP, Chestnutt IG, Saunders EM (1999) Factors influencing the diagnosis and management of teeth with pulpal and periradicular disease by general dental practitioners. Part 1. Br Dent J 187: 492-497.
- Koshy S, Chandler NP (2002) Use of rubber dam and its association with other endodontic procedures in New Zealand. N Z Dent J 98: 12-16.
- Smith GE, Richeson JS (1981) Teaching of rubber dam technique in North America. Oper Dent6: 124-127.
- Ryan W, O'Connel A (2007) The attitudes of undergraduate dental students to the use of the rubber dam. J Ir Dent Assoc 53: 87-91.
- Ireland EJ (1962) The rubber dam -- its advantages and application. Tex Dent J 80:10.
- Hagge MS, Pierson WP, Mayhew RB, Cowan RD, Duke ES (1984) Use of rubber dam among general dentists in the United States Air Force dental service. Oper Dent 9: 122-129.
- Joynt RB, Davis EL, Schreier PH (1989) Rubber dam usage among practicing dentists. Oper Dent 14: 176-181.
- Mala S, Lynch CD, Burke FM, Dummer PM (2009) Attitudes of final year dental students to the use of rubber dam. IntEndod J 42: 632-638.
- Marshall K, Page J (1990) The use of rubber dam in the UK. A survey. Br Dent J 169: 286-291.
- Palmer NO, Ahmed M, Grieveson B(2009) An investigation of current endodontic practice and training needs in primary care in the north west of England. Br Dent J 206: E22; discussion 584-585.
- Brookman DJ (1991) Vocational trainees' views of their undergraduate endodontic training and their vocational training experience. IntEndod J 24: 178-186.
- Going RE, Sowinski VJ (1967) Frequency of use of the rubber dam: a survey. J Am Dent Assoc 75:158-166.
- Hill EE, Rubel BS (2008) Do dental educators need to improve their approach to teaching rubber dam use? J Dent Educ 72: 1177-1181.
- Reuter JE (1983) The isolation of teeth and the protection of the patient during endodontic treatment. IntEndod J 16:173-181.
- Stewardson DA (2002) Endodontics and new graduates: Part I, Practice vs. training. Eur J ProsthodontRestor Dent 10:131-137.
- Wilcox CW, Wilwerding TM (1999) Aid for preventing aspiration/ingestion of single crowns. J Prosthet Dent 81: 370-371.
- Fields RT, Jr., Schow SR (1998) Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: a review of the literature and report of five cases. J Oral Maxillofac Surg 56:1091-1098.
- Dental Tribune International. News item. Dental patients receive $35 million in compensation. July 22, 2013.
- Santos Tde S, Antunes AA, Vajgel A, Cavalcanti TB, Nogueira LR, et al. (2012) Foreign body ingestion during dental implant procedures. J Craniofac Surg 23: e119-123.
- Zitzmann NU, Elsasser S, Fried R, Marinello CP (1999) Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol 88: 657-660.
- Heling B, Heling I (1977) Endodontic procedu res must never be performed without the rubber dam. Oral Surg Oral Med Oral Pathol 43: 464-466.
- Etoz OA, Er N, Demirbas AE (2011) Is supraperiosteal infiltration anesthesia safe enough to prevent inferior alveolar nerve during posterior mandibular implant surgery? Med Oral Patol Oral Cir Bucal 16: e386-389.
- United States Nuclear Regulatory Commission.Glossary of Terms: ALARA.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 15906
- [From(publication date):
December-2016 - Apr 08, 2025] - Breakdown by view type
- HTML page views : 13614
- PDF downloads : 2292