Case Report Open Access
The Treatment Strategy of an Oblique Complicated Crown-root Fracture: Case Report
Rachid Fawzi1* and El Mehdi Hariri2
1Professor and Department’s chief in Pediatric Dentistry, Faculty of Dentistry, Center of Dental treatment and Consultation of Rabat, University of Mohammed V Rabat, Military hospital Mohammed V in Rabat Morocco.
2Resident doctor in Pediatric Dentistry, Faculty of Dentistry, Center of Consultation and Dental treatment of Rabat University of Mohammed V Rabat, Military hospital Mohammed V in Rabat Morocco.
- *Corresponding Author:
- Rachid F
Faculty of Dentistry
Center of Dental treatment and Consultation of Rabat
Pediatric Dentistry department
University Mohamed V Rabat Morocco
B.P: 6212-Rabat Institute Rabat Morocco
Tel: +212661208830
E-mail: fawzirachid@yahoo.fr
Received Date: June 02, 2016; Accepted Date: June 08, 2016; Published Date: June 17, 2016
Citation: Fawzi R, Hariri M (2016) The Treatment Strategy of an Oblique Complicated Crown-root Fracture: Case Report. Pediatr Dent Care 1:110. doi:10.4172/pdc.1000110
Copyright: © 2016 Rachid F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
A complicated crown-root fracture is defined as a fracture involving enamel; dentin and root cementum extends longitudinally to the sub-gingival area and sometimes compromises the biologic width. This case report describes an oblique complicated crown-root fracture with an irreversible pulpitis of the maxillary right central and lateral incisors in a young patient who has 13 years old. The treatment strategy included endodontic therapy followed by reattachment of fractured fragment reinforcing with a prefabricated post. After 4 years of following-up, the reattached fragment presents satisfying esthetics, excellent function and good state of periodontal health.
Keywords
Crown-root fracture; Sub-gingival; Reattachment, Osteotomy
Introduction
Maxillary incisors are the most common teeth involved in dental trauma and, sometimes, a complicated crown-root fracture occurs. It’s characterized by a fracture involving enamel, dentin, cementum with pulpal involvement [1-3]. Esthetical and functional rehabilitation of crown-root fractures of the anterior maxillary is one of the greatest challenges to the dentist. Depending upon the extent of fracture line, different treatment approaches have been indicated. It’s including orthodontic or surgical extrusion, gingivectomy and osteotomy/ osteoplasty, intentional replantation or extraction [4]. However, when the tooth fragment is available and there is no or minimal invasion of the biological width, the best treatment option for managing coronal is the reattachment of the fractured tooth fragment, especially in young patients [4-6].
The objective of the present paper is to describe the management of a complicated crown-root fracture that extended subgingivally in an anterior tooth by osteotomy and reattachment of the fractured tooth fragment, with 4 years of follow-up.
Case Report
A 13 year-old male patient presented at to the Department of Pediatric Dentistry and Prevention of Rabat University, for hard and spontaneous pain on touching his maxillary incisors. The patient reported that the fracture occurred by a bicycle accident 48 hours prior to his attendance.
The general dental practitioner carried out clinical and radiological examination and performed emergency treatment, restored only with a composite splint.
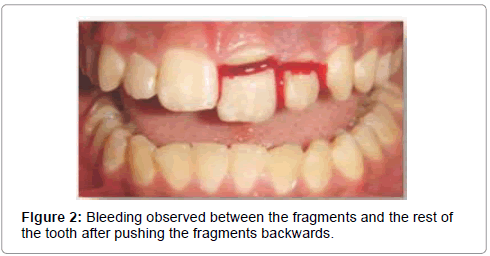
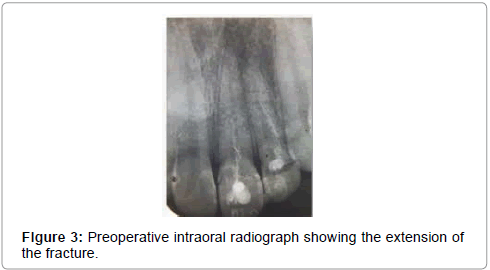
Past medical history was reviewed and there was no remarkable report. The initial clinical examination did not reveal any soft tissue, temporomandibular joint and osseous structures injury. Intraoral examination revealed that right maxillary central and lateral incisors were broken, and the vestibular surface showed a composite splint (Figure 1). After removing the splint, the coronal fragments of the tooth were mobile but they were still attached labially by fragile soft tissue. Bleeding was observed between the fragments and the rest of the tooth (Figure 2). Pulp vitality of the right maxillary incisors was checked using a sensibility testing (cold test). They showed intense pain response and no sign of mobility. Intraoral periapical radiographic investigation taken from different angles revealed an oblique crownroot fracture, no endodontic filling, complete root formation on the both incisors, intact periodontal ligament space and there was no additional root fracture (Figure 3). Pushing gently backwards the fragments and displacing them slightly toward the palate, we discovered a fissure of the whole groove that expanded below the gingival level at the palatal surface of the both tooth. Based on the clinical and radiographic findings, a diagnosis of oblique crown-root fracture and irreversible pulpitis was made. After discussing with the patient and his father the available treatment options with their respective advantages, drawbacks, limitations, prognosis, and cost of each treatment, we opted for the reattachment of the crowns by using fiber-reinforced posts.
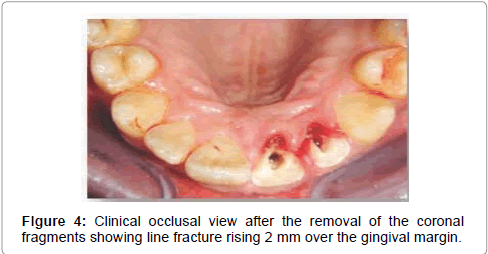
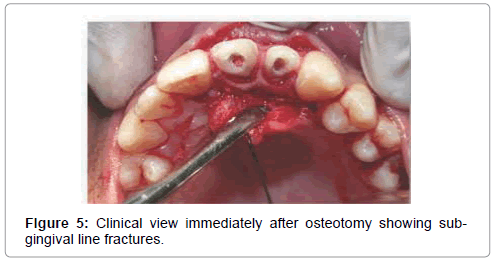
Under local anesthesia, the fragments were removed to clinically evaluate the extends deepness of the fracture line which confirmed that the line extended below the cemento-enamel junction on the palatal aspect. Pulp exposure was observed confirming the need for endodontic treatment (Figure 4). Both fractured fragments were in good condition, retaining complete morphology. Stored in sterile saline solution to dissolve the remaining pulp tissue and to prevent discoloration and dehydration, they were used in the next appointment in accordance with the restorative procedure. As the fracture lines in both teeth could not have been accessed, an incision was made from the gingival margin from the distal of the upper premolar to the distal of the upper lateral incisor. The gingival attachment and mucoperiosteal flaps were reflected on palatal aspect carefully separating soft tissues from the fractured tooth.
Given that our treatment first aim was to expose the fractured margins, we removed sharp bony structures over the fracture line until the whole fracture line was 2 mm above the bone (Figure 5). The tooth fragments were inserted until the fracture lines met to check if they were in continuity. They were adapted completely to each other along the fracture line with no visible gap in between. Root-canal therapy was carried out in a single session. Due the line of the fracture, the endodontic therapy could not be performed with the rubber dam. The pulp was extirpated and the root canal was cleaned, shaped and filled. Post space was prepared by partially removing the filling.
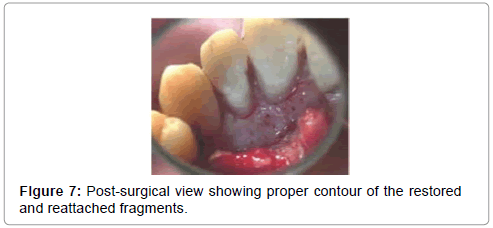
The positioning of fiber posts of corresponding size was checked radiographically. Post space was prepared in both the radicular portions of the tooth and the fractured crown fragments and post was selected in according to excellent esthetic and other advantages such as better translucency, ability to bond to tooth structure and having modulus of elasticity comparable to that of dentin. Adequate isolation was maintained throughout the procedure by means of cotton rolls and a saliva ejector. After etching the coronal fragment with a 37% phosphoric acid gel for 20 s, the crown was rinsed under running water for another 20 s. And after hemorrhage control, a thin adhesive system was applied to both the coronal and the root fragments. By using a dual-curing luting composite, the coronal fragment was reattached to the root fragment and then polymerized (Figures 6 and 7). Excess cement was removed. The margins were polished with the composite polishing kit and the access to the tooth was restored with a composite resin.
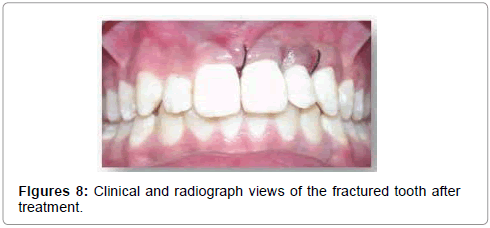
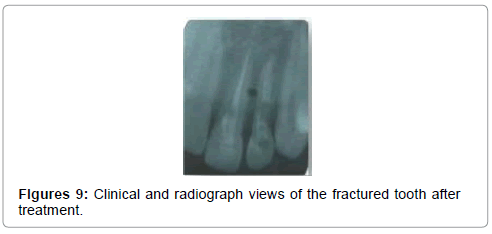
After finishing and polishing, the restoration was checked radiographically for occlusal interferences and the flap was then reapproximated to its original position and esthetically sutured (Figures 8 and 9). Then we prescribed 0.2% chlorhexidine daily rinses during the first week following suture removal and informed the patient about the importance of maintaining meticulous oral hygiene and regularly returning for clinical and radiograph monitoring.
The patient was seen 1week and 1month later, he was asymptomatic. Clinical examination revealed a stable reattachment of crown fragments, a normal mobility, and radiographic examination showed a stable reattachment of the fragments and good periodontal health.
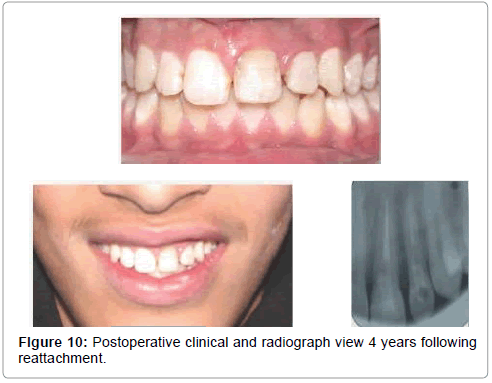
At 6 months, the esthetic and functional outcomes remained satisfactory and periodontal health was stable, with no radiologic signs. After 4 years, reattachment of the fragment was still stable with a good esthetics with good periodontal health and no signs of root resorption (Figure 10).
Discussion
A crown-root fracture is a type of dental trauma, usually resulting from horizontal impact, which involves enamel, dentin and cementum, it occurs below the gingival margin and depending on pulp involvement, it may be classified as complicated or uncomplicated [1,3]. Extraction of traumatized tooth followed by surgical implants placement, crown lengthening by gingivectomy and ostectomy or orthodontic extrusion, intentional replantation and reattachment of the coronal fragment to the root surface are the main treatment modalities proposed to address this problem presenting each proper advantages, disadvantages, limitation, prognosis and cost [3,6-10]. As a result, each case of trauma should be evaluated on an individual basis. In making a treatment decision related to young patients, risks and benefits of each treatment option should be carefully evaluated taking into consideration the patient’s age, the root development stage, the morphology of the lesion, the potential’s eruption and the patient’s/parents’ preference [9]. In our case, there were some possible options for the treatment: extraction should not be an option of treatment because it leads to loss of bone in in the anterior area, compromising future treatment with eventual implants. Moreover, placement of implant during childhood is contraindicated before the end of the alveolar growth. Orthodontic extrusion is an alternative for the treatment of subgingival fractures. Nevertheless this alternative affects esthetics and occlusion and requires longer time considering the period of extrusion and stabilization [10,11]. When intact fragments are available, reattachment would be the best option of the treatment, it may offer many advantages: better esthetics, less time consuming and positive emotional and social response from the patient for the preservation of natural tooth structure [4,9,10,12]. It is the best method of reinstating the fragment’s natural shape, contour, surface texture, preservation of incisal translucency preservation of identically occlusal contacts and colorstability [9]. It eliminates the problems of differential wear of restorative materials and offers excellent esthetic and functional results [13]. Also, this procedure is relatively simple, atraumatic and inexpensive. Site of fracture, size of fractured remnants, periodontal status, pulpal involvement, maturity of the root formation, biological width invasion, occlusion, material used for reattachment and use of post are the main factors that influence reattachment success [14,15].
The treatment described in the present case report is relatively simple and atraumatic adopting a very conservative approach. It included endodontic therapy followed by reattachment of fractured fragment. Developments in restorative materials and techniques have facilitated reattachment of fractured teeth, nonetheless, one of the difficulties of treatment, is to expose the fractured margins, and to conduct restoration procedures without contamination with blood and saliva compromising the adhesion [16].
The fracture site was subgingival and intraosseous, surgical techniques with an elevation of a tissue flap, clinical crown-lengthening surgery with removal of alveolar bone for access to the fractured site wasthen necessary [9,17,18].
A dry and clean working field and the proper use of bonding protocol and materials is the key for achieving success in adhesivedentistry [19]. In this case, clinical examination revealed pulpal involvement confirming that endodontic treatment was required. Fiber posts were placed to achieve retention form and serve to protect the bond from rotational and twisting forces, which might reduce thepotential for success. The use of post increases retention and disperses the stress along the root. Supported by the glass fiber post the fractured crown can be permanently bonded to the root connecting the fiber post with the resin cement, increasing the retention of segment and providing a monoblock effect [13,20].
Reports and clinical experience indicate that the reattachment of fractured coronal fragments results in successful short- and mediumterm outcomes [8,14]. According to some authors, the reattachment could be considered a transitional restoration for a young patient who may need definitive prosthetic rehabilitations such as direct adhesive veneers or crowns in the event of reattachment failure. The patient should be informed of the possible interim nature of the treatment. This conservative approach will not compromise or complicate alternative treatment options in the future [15,17].
As with all traumatic injuries, following-up is of critical importance. The patient should be seen at 3, 6, and 12 months and yearly for 5 years. Esthetics and periodontal status should be confirmed both clinically and radiographically at these control visits.
In this case after 4 years, clinical and radiograph examinations revealed good esthetic, functional outcomes and integrity of periodontal health.
Conclusion
The treatment strategy of complicated crown-root fracture is complex, due to sub-gingival position of the fracture margin encroached on the biological width. The reattachment of the fractured tooth fragment after surgical exposure of the fracture margin by osteotomy may be an alternative option. In This case report, the success was obtained, with 4 years of follow-up. This technique is relatively easy to perform and the tooth can be restored soon after injury. It should be considered when treating patients with fractures of the anterior teeth, especially younger patient.
References
- Spinas E, Altana MA (2002) new classification for crown fractures of teeth. J Clin Pediatr Dent 26:225–231.
- Tapias MA, Jiménez-García R, Lamas F and Gil AA (2003) Prevalence of traumatic crown fractures to permanent incisors in a childhood population: Móstoles, Spain. Dent Traumatol, 19: 119-122.
- Andreasen JO, Andreasen FM, Tsukiboshi M. (2007) Crown-root frac- tures. In: Andreasen JO, Andreasen FM, Andersson L, Eds. Text book and Color Atlas of Traumatic Injuries to the Teeth. (4th edn) Copenhagen: Blackwell Munksgaard, INDIA.
- Pallav P, Deshraj J and Gaurav GA (2010) Holistic approach to management of fractured teeth fragments: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109: 70-74.
- Neha S, Manmohan B (2015) A new clinical approach for rehabilitation of crown fracture by fragment reattachment - A case report. International Journal of Dental Science and Research 1-5.
- Poi WR, Cardoso LC, De Castro JC, Cintra LT, Gulinelli JL, et al. (2007) Multidisciplinary treatment approach for crown fracture and crown-root fractured: a case report. Dent Traumatol 23: 51-55.
- Meiers JC, Freilich MA (2001) Chairside prefabricated fiber- reinforced resin composite fixed partial dentures. Quintessence Int 32: 99-104.
- Reis A, Loguercio AD, Kraul A and Matson E (2004) Reattachment of fractured teeth: A review of literature regarding techniques and materials. Oper Dent. 29: 226-233.
- Andreasen JO, Bakland LK and Andreasen FM (2006) Traumatic intrusion of permanent teeth. Part 3. A clinical study of the effect of treatment variables such as treatment delay, method of repositioning, type of splint, length of splinting and antibiotics on 140 teeth. Dent Traumatol 22: 99-111.
- Kudou Y, Kubota M (2003) Replantation with intentional rotation of a complete vertically fractured root using adhesive resin cement. Dent Traumatol 19: 115-117.
- Emerich PK, Sawicki L, Bodal M and Adamowicz KB (2005) Forced eruption after crown/root fracture with a simple and aesthetic method using the fractured crown. Dent Traumatol 21: 165-169.
- Terata R, Minami K and Kubota M (2005) Conservative treatment for root fracture located very close to gingiva. Dent Traumatol 21: 111-114.
- Murali M, Mahesh G, Shashidhar MP (2015) Clinical evaluation of the fiber post and direct composite resin restoration for fixed single crowns on endodontically treated teeth. Medical journal armed forces India 71 259-264.
- Grandini S, Goracci C, Tay FR, Grandini R and Ferrari M (2005) Clinical evaluation of the use of fiber posts and direct resin restorations for endodontically treated teeth. Int J Prosthodont. sepeoct; 18: 399-404.
- Lassila VJL, Tanner J and Le Bell AM (2004) Flexural properties of fiber reinforced root canal posts. Dent Mater 20: 29-36.
- Tay FR and Pashley DH (2007) Monoblocks in root canals: A hypothetical or tangible goal. J Endod 33: 391-398.
- Sandra RF, Rivail AS, Luciana MS, MURAD FS and Rivail ASF (2011) Clinical Management of a Complicated Crown-Root Fracture: A Case Report. Braz Dent J 22: 258-262.
- Sanjay V, Deepak JP, Saloni P (2013) Multidisciplinary Approach to the Rehabilitation of Maxillary Incisors with Complicated Crown-Root Fracture: 6 Months Follow Up. J Res Adv Dent 2: 59-64.
- Tamotsu T, Sakurako M, Yoshimi K, Kinuyo O, Yusuke Sand Bunnai O (2012) Esthetic and endodontic management of a deep crown-root fracture of a maxillary central incisor. Journal of Oral Science, 54: 359-362
- Dede DO, Emine ST, Ahmet U, Güler S, Yazicioglu et al. (2013) Multidisciplinary approach to a subgingivally fractured incisor tooth: A case report, Journal of Dental Sciences 1: 1-5
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 15096
- [From(publication date):
specialissue-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 14201
- PDF downloads : 895