Review Article Open Access
The Surgical Treatment of Trigeminal Neuralgia
Sergio Zeme*
Department of Neurosciences, Neurosurgical Treatment of Pain and Spasticity Unit, University of Turin, Pain Theray and Palliative Care Division, Italy
- *Corresponding Author:
- Sergio Zeme
Department of Neurosciences, Neurosurgical Treatment of Pain and Spasticity Unit
University of Turin, Pain Therapy and Palliative Care Division, ”Rita Levi Montalcini”-Molinette Hospital
AOU “Città della Salute e della Scienza”, Via Cherasco, Torino, 15-10126, Italy
Tel: +39-11677078
Email: sergio.zeme@unito.it
Received date: August 10, 2016; Accepted date: August 16, 2016; Published date: August 19, 2016
Citation: Zeme S (2016) The Surgical Treatment of Trigeminal Neuralgia. J Pain Relief S4:006. doi:10.4172/2167-0846.S4-006
Copyright: © 2016 Zeme S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Trigeminal Neuralgia is a clinical presentation of different diseases, defined in the last edition of the International Classification of Headache Disorders (ICHD-3) as “Classical Trigeminal Neuralgia” and “Painful Trigeminal Neuropathy”. In both groups typical and atypical clinical findings are present. They must be taking into consideration for defining a correct clinical diagnosis. In addition MRI findings and other objective signs allow to disclose the Etiology of the Trigeminal Neuralgia. The surgical treatment offers many options: open surgery in posterior fossa, neuroablative procedures on the trigeminal nerve, neuromodulation techniques on the trigeminal pathways. Open surgery and neuroablative procedures are the treatments chosen in Classical Trigeminal Neuralgia and in Painful Trigeminal Neuropathy showing pure or prevalent typical clinical findings. Instead in Painful Trigeminal Neuropathy with pure or prevalent atypical clinical findings the neuromodulation techniques are the treatments to be chosen. Looking at the Literature reports and at our own experience, techniques, results, and indications of microvascular decompression, radiofrequency thermocoagulation, glycerol rhizolysis, balloon microcompression, and sterotactic radiosurgery of the trigeminal root are reported and discussed
Keywords
Trigeminal neuralgia; Surgical treatment; Microvascular decompression; Radiofrequency thermocoagulation; Glycerol rhizolysis; Balloon microcompression; Sterotactic radiosurgery
Introduction
Trigeminal neuralgia is a painful condition of the face usually having a clear-cut clinical presentation: evoked paroxysmal pain in one or more unilateral trigeminal branches. The surgical treatment has gained a chance of success superior to that applied to any other types of chronic pain and is much more effective than the medical treatment [1-3]. But at the condition that it is delivered to the right patient.
Actually Trigeminal Neuralgia (TN) is a clinical presentation of different diseases, whose taxonomy has been widely discussed and recently summarized in the last edition of the International Classification of Headache Disorders (ICHD-3) [4]. Two subgroups of TN are firstly indicated: Classical Trigeminal Neuralgia (CTN) and Painful Trigeminal Neuropathy (PTN).
CTN is further divided in CTN purely paroxysmal and CTN with concomitant persistent facial pain. This denomination encompasses the cases classified before as primary, essential, and idiopathic trigeminal neuralgia. Actually the surgical exploration of the trigeminal nerve in the posterior fossa and the improvement of neuroimaging by MRI has shown that there is an often recognizable etiology: the neurovascular conflict.
PTN identifies the cases classified before as secondary trigeminal neuralgia. The following subgroups are indicated: PTN attributed to acute herpes zoster, post-herpetic trigeminal neuropathy, posttraumatic trigeminal neuropathy, PTN attributed to Multiple Sclerosis (MS) plaque, to space-occupying lesion, and to other disorders.
The clinical diagnostic criteria of CTN are clearly defined in a six point list, summarizing the well-known clinical findings reported in the literature starting from the ancient descriptions of the XVII-XVIII century [5]:
At least three attacks of unilateral facial pain fulfilling criteria B and C.
Occurring in one or more divisions of the trigeminal nerve, with no radiation beyond the trigeminal distribution
• Pain has at least three of the following four characteristics:
• recurring in paroxysmal attacks lasting from fraction of a second to 2 minutes
• severe intensity
• electric shock-like, shooting, stabbing or sharp in quality
• precipitated by innocuous stimuli to the affected side of the face
• No clinically evident neurological deficit
• Not better accounted for by another ICHD-3 diagnosis.
These are the so called “typical clinical findings”, to whom are usually added other features: completely pain-free periods after the attacks, refractory period after the painful paroxysms, spontaneous prolonged periods of remissions of the pain attacks for weeks or months, abolition of pain by antiepileptic drugs (mainly carbamazepine and oxacarbazepine).
It is well accepted that in some patient at the beginning or during the history of the disease other so called “atypical clinical findings” can appear: spontaneous pain attacks, prolonged pain aching or burning after the paroxysms, sensory deficits in the area of pain, resistance to the antiepileptic drugs.
For this reasons the ICHD committee introduced the definition of “CTN purely paroxysmal” and “CTN with concomitant persistent facial pain” in the substitution of the previous denomination of trigeminal neuralgia type 1 and type 2 [6].
The ICDH-3 characters of CTN are related to the cases of TN “developing without apparent cause other than neurovascular compression”. Recently Cruccu and co-workers criticized this definition [7]. They stressed that, although TN is a prototype of neuropathic pain, the cases in which the conflict is absent or cannot be demonstrated do not completely fit the grading system for the diagnosis of definite neuropathic pain [8]. Then they proposed to maintain in these cases the definition of “idiopathic trigeminal neuralgia”, characterized by a “clinically established TN” diagnosis. CTN diagnosis should be reserved to the “Etiology established TN” in which the neurovascular conflict has been demonstrated. This is relevant for the Neurosurgeon, first of all because most of the patients are referred by the Neurologists or the Pain Therapists and it is essential to have the same language. Moreover a very important question for the Neurosurgeon arises: is it still justified the posterior fossa exploration when MRI does not clearly show the neurovascular conflict? We are still waiting for a convincing answer.
The same clinical findings of CTN can appear in the PTN, mainly in the cases attributed to MS or space-occupying lesions. But it is well recognized that in these diseases the atypical clinical findings are more often present, and sometimes prevalent, especially in post-herpetic and post-traumatic trigeminal neuropathies. The grading system for the diagnosis of definite neuropathic pain in these cases is completely satisfied because “objective signs or tests that reveal an underlying lesion or disease of the nervous system” [8] can be easily found.
Finally the ICHD-3 classification clearly keeps separated the TN from the “Persistent idiopathic facial pain (PFIP)”. In this disease, previously defined as “atypical facial pain”, any surgical procedure is contraindicated, because it is either useless or making the pain worse.
The surgical treatment of TN offers various procedures
Open surgical operations for removing the compression of the trigeminal nerve, by eliminating the neurovascular conflict or the tumor;
Neuroablative operations for reducing the trigeminal input: percutaneous procedures or stereotactic radiosurgery on the retrogasserian trigeminal root. Open surgical trigeminal rhizotomy and tractotomy are nowadays rarely performed;
Neuromodulation procedures, such direct electrostimulation of the peripheral trigeminal branches, the gasserian ganglion, the motor cortex or the spinal cord [9,10], transcranial magnetic or electric stimulation of the motor cortex [11], intrathecal drugs delivery [12], and pulsed radiofrequency of peripheral trigeminal branches or gasserian ganglion [13].
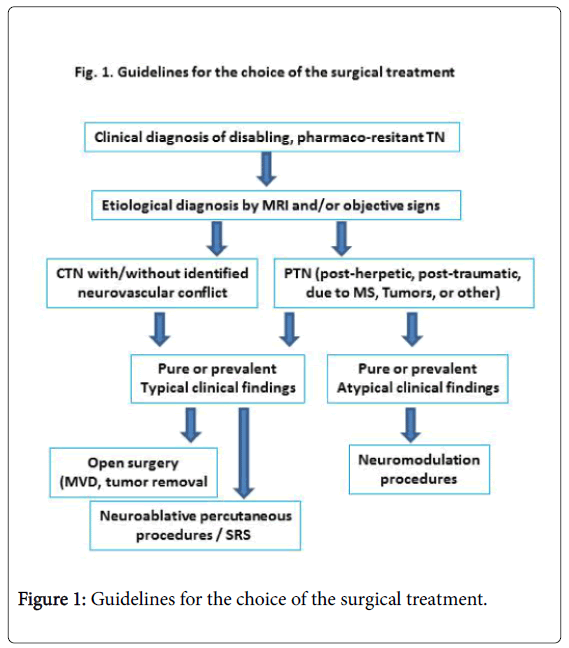
The pathophysiology, the clinical presentation and the etiology of the TN give the guidelines to the surgeon for choosing the more useful procedure in any particular case (Figure 1).
As a general rule, microvascular decompression, percutaneous neuroablative procedures and stereotactic radiosurgery are as much effective as the typical clinical findings of TN are prevalent. When atypical clinical findings, that are the clinical signs of severe trigeminal neuropathy, are the only or the prevalent elements, neuromodulation procedures must be preferred. They will not be described in this revue.
In this paper we will report the technique, the indications and the results of the surgical procedures, looking at the Literature and at our experience regarding 1,041 patients operated on by 1,197 procedures at the Neurosurgical Department of the University and at the Pain Therapy Division of the Molinette Hospital in Turin (Table 1).
| Procedures | N. of procedures (n. of patients) |
Age min-max (mean) years | Period | Notes |
|---|---|---|---|---|
| MVD | 245 (239) | 18-76 (56) | 1981-2015 | CNT: 240 (235) MS: 5 (5) |
| PCA Tumor removal | 23 (23) | 22-76 (53) | 1982-2015 | Epidermoid: 7 Acoustic neu: 9 Meningioma: 5 AAV: 1 |
| PMC | 565 (498) | 34-94 (68) | 1982-2015 | CTN: 420 (354) PTNMS: 136 (116) PTNTu: 8 (7) |
| RFT | 57 (54) | 42-89 (64) | 1975-1989 | CTN: 51 (50) PTNMS: 6 (4) |
| GR | 27 (27) | 55-84 (65) | 1982-1985 | CTN: 25 |
| Cryolysis | 222 (158) | 21-84 (63) | 1977-1991 | CTN: 138 (196) PTNMS: 20 (26) |
| PDRF peripheral branches | 58 (42) | 36-85 (58) | 2010-2015 | PHTN: 39 (30) PPTTN: 19 (12) |
| Total | 1197 (1041) | 18-94 (65) | - | - |
MVD: Microvascular decompression, CPA: cerebello-pontine angle, PBC: Percutaneous Balloon microcompression, RFT: Radiofrequency Thermocoagulation, GR: Glucerol rhizolysis, PDRF: Pulse-Dose Radiofrequency.
CTN: Classical trigeminal neuralgia, PTNMS: Painful trigeminal neuropathy attributed to multiple sclerosis, PTNTu: Painful trigeminal neuropathy attributed to tumor, PHTN: Post-herpetic trigeminal neuropathy, PPTTN: Painful post-traumatic trigeminal neuropathy.
Table 1: Personal series: patients operated on and/or followed up by the author at the Neurosurgical Department of the University and at the Pain Therapy Division of the Molinette Hospital in Turin.
Pathophysiological Basis of Surgical Treatment
The pathophysiological basis of the surgical treatment relies on our knowledge about the pathophysiology of trigeminal neuralgia. It has been extensively studied mainly in classical trigeminal neuralgia [14-18]. The growing knowledge about the mechanisms of neuropathic pain has clarified the pathophysiology of the painful trigeminal neuropathies too [19].
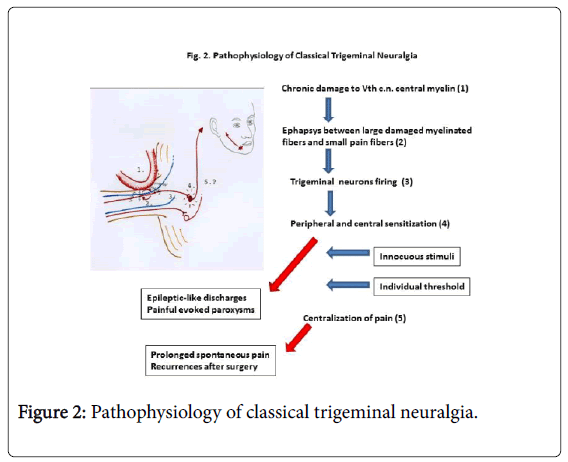
According to most of the Authors, the pathophysiology of CTN is a process following different steps (Figure 2). The first step is a damage to the central myelin of the trigeminal fibers either in the dorsal root entry zone (by neurovascular conflict or cerebello-pontine angle tumors) or in the pons (by multiple sclerosis plaque). The second step is the production of “ephapsys”, allowing that tactile, proprioceptive, and thermal stimuli conveyed by the damaged myelinated fibers be transmitted to the pain fibers.
The third step is the sensitization of the trigeminal neurons, chronically “fired” by this exaggerated number of painful stimuli. These neurons become hyperexcitable and the process of peripheral and central sensitization progresses (fourth step). Following the individual threshold, having a high inter- and intra-individual variability, the hyperexcitable trigeminal neurons can be activated by further non-painful stimuli and they respond by a simil-epileptic discharge, causing the painful attacks. As the trigeminal damage progresses the paroxysmal attacks subside to the prolonged neuropathic pain and the fifth step is likely to be achieved: a selfsustaining centralization of pain.
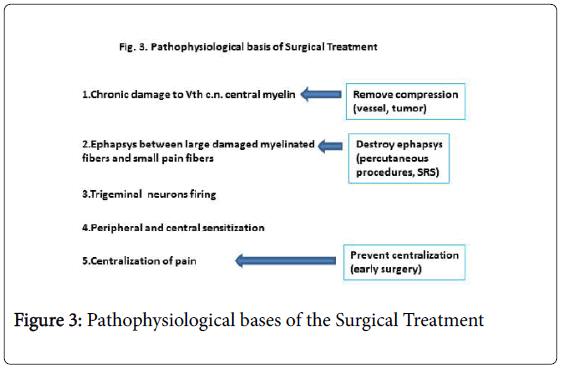
According to this schematization the pathophysiological bases of the surgical treatment are summarized in the (Figure 3).
The surgical removal of offending vessels (and tumors) from the posterior trigeminal root blocks this process at its first step. A progressive damage to the root is prevented and a natural repair of the damaged trigeminal fibers is allowed in most cases. The patient can be cured from his CTN, without additional damage to the trigeminal nerve. CTN recurs only in case of either self-sustaining central sensitization of trigeminal neurons or a new conflict.
Percutaneous techniques on the gasserian ganglion act at the second step of the CTN pathophysiological process, producing a suitable limited deafferentation of the trigeminal root. Balloon compression and glycerol rhizolysis could selectively destroy the damaged large myelinated fibers originating the ephapsys. In fact the large A myelinated fibers, mainly if damaged, are more sensitive to the ischemic or chemical damage than the small B or C pain fibers [20,21]. The painful attacks can be abolished without significant sensory deficits. CTN can recur if either the etiological factors (neurovascular conflict, tumors, multiple sclerosis) produce further damage to the residual fibers or a self-sustaining central sensitization is just present. Radiofrequency thermocoagulation could selectively destroy the smaller B and C pain fibers involved by the ephapsys, because they are more sensitive to the heating than the A fibers [22,23]. The painful attacks can be abolished producing only minimal sensory deficits (hypo or analgesia) involving the pain fibers serving the trigger area. Again CTN can recur due to either a further damage to the residual fibers or a self-sustaining central sensitization.
Radiosurgery probably acts at the second step also, by destroying part of the trigeminal fibers. We do not know yet if there is some kind of specific vulnerability either of the damaged large myelinated fibers or of the smaller pain fibers.
The PTN cases present very different kinds of damage to the trigeminal nerve depending on the different diseases.
In PTN attributed to MS plaque or cerebello-pontine angle slowly growing tumors the pathophysiological mechanisms are very similar. A light demyelinization of the large fibers in the trigeminal REZ is produced by the MS plaque or the compressive effects of the tumor. Actually the clinical presentation is often the same as in CTN. In MS cases the progression of the disease can produce a more severe damage leading to an increasing loss of trigeminal fibers. The same phenomena are caused by the tumor growth. The heavier damage to the trigeminal nerve is indicated by the clinical picture showing the appearance of the atypical findings: mainly spontaneous paroxysms, prolonged pain after paroxysms, evident sensory deficits, neurovegetative phenomena, and resistance to the antiepileptic drugs. The mechanisms of peripheral neuropathic pain are ignited: ectopic activity, peripheral and central sensitization [19].
The surgical treatment should be chosen on the basis of the degree of the deafferentation as shown nowadays mainly by the clinical picture. If the CTN typical findings are prevalent the neuroablative percutaneous procedures or stereotactic radiosurgery are indicated. As far as the atypical findings are more severe the choice should be driven to the neuromodulation procedures. In the cases of cerebollo-pontine angle or more anterior skull base tumors the surgical removal of the lesion is mandatory, wherever is possible.
In the post-herpetic and post-traumatic trigeminal neuropathy, the damage to the peripheral fibers is heavier and the mechanisms of neuropathic pain are progressing quickly. The clinical picture is dominated by the atypical findings. In these cases neuroablative procedures making further trigeminal deafferentation are not indicated, being useless and at risk of worsening pain. The neuromodulative procedures have to be chosen.
Microvascular decompression
The first observations on the compression of the trigeminal root by an artery or tumors as possible cause of TN have been made by Dandy during his approach to the cerebello-pontine angle for trigeminal rhizotomy [24]. But it was only with the introduction of the surgical microscope and the extensive experience of Jannetta [25] that the importance of the neurovascular conflict as a cause of trigeminal neuralgia (as well as of other cranial nerves dysfunction) was recognized and his technique widely accepted [26].
Surgical technique
The patient is positioned in park-bench or lateral position, with the head flexed and tilted of about 10° toward the floor. A round or triangular small retromastoid craniectomy, exposing the inferior border of the transverse sinus and the posterior border of the sigmoid sinus, is performed. The dura is opened in a reversed “Y” or round flap and the borders suspended. By allowing generous drainage of the cerebrospinal fluid the cerebellar hemisphere is gently moved away from the tentorium and the petrous bone. Following the angle between tentorium and the petrous bone via a supracerebellar route the Dandy vein and then the trigeminal root is reached. The careful dissection of the arachnoid around the trigeminal root from its entry in the pons to its exit in the porus trigemini allows to show in about 95% of cases one or more offending arteries and/or veins. The arteries are carefully dissected from the root and kept far from it spontaneously. A nonabsorbable (Teflon, Goretex) or absorbable (oxidized cellulose, fibrin glue) materials are then interposed between the artery/arteries and the pons. In most favourable situations an offending superior cerebellar artery or its branches can be translated between the Dandy vein and the tentorium. In rare cases more complicated techniques requiring the suspension of the offending artery to the tentorium or the petrous bone dura by stitches are needed. Veins are either dissected or, if possible, coagulated and sectioned.
Results
Following the data of the published series [1,27-29] (Table 2), the painful attacks are immediately abolished in 80-98% of cases (mean: 92%). A long-term success is reported in 62-89% of cases (mean 77%) at 5-11 years. In two series the actuarial curve at more than 10 years has been calculated, resulting that 70% of patient are free from pain (without needing medications) at 10 years [30] and 73% at 15 years [31] and remain essentially stable later. Severe complications from vascular accidents in the cerebellum or brainstem and leading to severe neurological deficits or death are reported in 0-1% of cases. Definitive deficits of the VIII, VII, IV cranial nerves appears in 0-5% of cases. Sensory deficits in the face are rare and usually mild (2-15% of cases) and also dysesthesias (>1%).
Percutaneous techinques
These techniques allow producing a suitably discrete lesion in the retrogasserian portion of the trigeminal root. Techniques and results have been summarized in recent revues [1,27-29,32,33] (Table 2).
| Patients outcomes %min-max (mean) |
MVD | RFT | GR | PBC | SRS |
|---|---|---|---|---|---|
| Initial pain relief | 80-98 (92) | 81-99 (94) | 42-98 (75) | 82-100 (96) | 75-92 (80)a |
| Long-term pain relief b | 62-89 (77) | 20-93 (60) | 18-59 (38) | 54-91 (67) | 46-65 (50) |
| Facial hypoesthesiac | 2-15 | 5-98 (40) | 1-29 | 20-35 | 10-42 |
| Facial dysesthesiac | 0-1 | 1-12 | 0.7-12 | 1.5-5 | 0-4 |
| Anesthesia dolorosac | 0 | 0-2 | 0-3 | 0 | 0 |
| Corneal sensory lossc | 0 | 1-20 | 0-5 | rare | rare |
| Masticatory weaknessc | 0 | 3-29 | 0-4 | 0-10 | rare |
| Diplopiac | 0-1 | 0-1 | 0-0.2 | 0-1 | rare |
| Hypoacusiac | 0.8-5 | 0 | 0 | 0 | rare |
| Major neurolgical deficitsc | 0-1 | 0 | 0 | 0 | 0 |
| Mortality | 0-1 | >1/1000 | 0 | >2/1000 | 0 |
MVD: Microvascular decompression. RFT: Radiofrequency thermocoagulation. GR: Glycerol rhizolysis. PBC: Percutaneous microcompression. SRS: Stereotactic radiosurgery.
aPain relief within 1 year from the procedure. bMean values of long-term pain relief are calculated at least at 5 years from the procedures. c Definitive neurological deficits.
Table 2: Patients outcomes after different surgical procedures for TN.
Surgical Technique for Approaching the Meckel’s Cave
The trigeminal root is reached by a needle or trocar. It is introduced following the Hartel’s technique trough the face into the foramen ovale and then in the gasserian ganglion. The patient lies supine with the head extended under heavy sedation with intravenous anaesthetic agents and opioids. General anaesthesia is nowadays rarely required. The needle is inserted in the check 2.5-3 cm aside from the oral commissure, then directed in the sagittal plane toward a point lying 2-3 cm anterior to the external auditory meatus along the orbitaltragus line and in the frontal plane toward a point lying along the midline or the medial line of the pupil on the supraciliar arcade or the inferior margin of the orbit. The skull base is reached hopefully against the pterygoid process. The position of the needle is checked by fluoroscopy. In lateral projection the tip of the needle should be directed toward the angle between the superior margin of the petrous bone and the dorsum sellae. In more difficult cases or during the learning period an Edgart projection showing the phoramen ovale or the neuronavigation technique can be used. The entrance in the phoramen ovale is preceded by a brief contraction of the masticatory muscles due to the irritation of the trigeminal motor root by the needle. Then a characteristic loss of resistance because the needle tip is trespassing the nerve is felt. The penetration should be immediately stopped. The needle tip position checked by a lateral fluoroscopy and subsequent movements in the Meckel’s cave done after the sharp stylet is removed and a blunt stylet inserted.
Radiofrequency thermolesion
The Radiofrequency controlled thermolesion (RFT) has been the first percutaneous technique introduced for avoiding the high risk of excessive damage to the trigeminal root caused by the alcohol or phenol injection in the Meckel cave or the uncontrolled electrocoagulation of the trigeminal root [22]. It has been the most widely used percutaneous technique. It is still nowadays the preferred procedure by the anaesthesiologists dedicated to the trigeminal pain therapy. The high sensitivity of the small fibers to the heat prevent its use in the TN cases where the pain affects the first branch, due to the high risk of the corneal reflex loss and of the neuroparalytic cheratitis. Difficulties in a correct positioning of the thermoelectrode in scarcely collaborating patients can prevents an effective but discrete lesion be produced.
Surgical technique
After the phoramen ovale has been cannulated, an electrode is introduced through the needle up in the root. The patient is awakened from the sedation. By a gentle electrostimulation facial paresthesias that the patient can refer and/or muscular contractions (trigeminofacial reflexes) are produced and allow to position the tip of the electrode between the fibers coming from the trigger area. Then the patient is sedated again and radiofrequency thermocoagulation is produced in a first step by 60-70°C applied during “30-60”. The procedure is repeated in other steps and stopped when an analgesia associated to light tactile hypoesthesia is obtained in the trigger area.
Results
Immediate abolition of the painful attacks is obtained in 81-99% of patients (mean 94%). Long-term abolition is obtained in 20-93% of cases, with a mean of 60% of cases at 5 years. Hypo- or anesthetic areas in the face remains in 5-98% (mean 40% of cases), most often mild. Major dysesthesias affect 1-12% of patients, and anesthesia dolorosa 0-2% of cases. Corneal sensory impairment has been found in 1-20%, and it caused a keratytis in 0.6-3% of cases. Masticatory muscles weakness is reported in 3-29% of cases, and diplopia in 0-1%. Mortality is less than 1 in every 1,000 cases, due to carotid lesion.
Glycerol rhizolysis
Introduced by Hakanson [34] the glycerol rhizolysis (GR) has been and is nowadays the less used percutaneous technique, in spite of its theoretical advantages of automatically finding and selectively destroying the large damaged trigeminal fibers, and then abolishing the pain without significant neurological deficits. But it is not easy to perform correctly because of the impossibility either to get the gasserian ganglion cystern or to measure exactly the quantity of glycerol to be injected.
Surgical technique
The GR is performed by introducing the needle in the gasserian cistern. The patient is in sitting position with the head flexed and rotated toward the affected side. The needle tip is pushed up until the cerebrospinal fluid come from the needle. Then a hydrosolic contrast medium is injected under radiographic control. The operator knows that he is in the correct spot when a radiographic image of the gasserian cistern is obtained. The contrast medium is withdrawn and a similar volume of glycerol is injected (usually 0.2-0.4 ml) and left in the cistern for few minutes. Some operator inject small doses of glycerol, checking the touch and pinprick sensation in the patient face, then stop the procedures when light hypoesthesia is obtained in the painful area. This procedure cannot be performed correctly if the gasserian cistern is not viable, like in patients with previous percutaneous procedures in the gasserian ganglion [35,36].
Results
An immediate abolition of pain is obtained in 42-98% of cases (mean: 75%), and long-term effects in 18-59% of cases (mean 38%). Persistent severe hypoesthesia remains in 1-29% of cases and major dysesthesias affect 0.7-12% of patients. Anesthesia dolorosa, corneal sensory loss, and diplopia are infrequent. Masticatory weakness is rare (0-4%). No intraoperative deaths have been reported.
Balloon microcompression
It was introduced by Mullan [37]. Among the percutaneous techniques, balloon microcompression (PBC) is the easier and less time consuming to perform correctly and does not require any patient collaboration. As in the GR the theoretical high sensitivity of the large damaged myelinated fibers to the compression could allow to automatically find and selectively destroying them, sparing the undamaged large fibers and more the small fibers. In this way the effect on the pain can be obtained without significant sensory deficits. Then this technique can be applied more safely to the TN involving the first trigeminal branch and with more chances of controlling the TN involving more than one trigeminal division territories.
Surgical technique
The PBC is performed by a 14 gauge trocar to reach the Meckel’s cavum. Then a Fogarty 4 French is introduced until its tip having the gonflable balloon exits from the needle. Under radiographic control in lateral projection the balloon is filled by hydrosolic contrast medium until it assumes a “pear-shaped” image (usually with 0.5-0.7 ml of contrast medium). The compression is maintained during about 1’. Sometime only an “oval-shaped” inflation of the balloon can be obtained also with the maximum volume of 1 ml. This can mean that the tip of the catether is outside the Meckel’s cave in the subtemporal arachnoidal space. A more correct positioning drawing back the catheter tip inside the Meckel’s cave can allow to obtain the pearshaped inflation. Sometime the balloon remains “oval-shaped” and this means that the patient’s Meckel’s cave is too wide, the trigeminal root is atrophic, or the dura covering of the cave has been lacerated. In these cases prolonging the compression to 2-3 minutes or more can be useful. An effective compression of the trigeminal root is indicated by ipsilateral conjunctival chemosis arousing from an inhibition of the sympathetic contingent directed to the eye. A trigemino-cardiac reflex causing baradicardia is also a good sign of effective compression. It can arise also at the penetration of the trocar in the trigeminal ganglion. The anaesthesiologist should be aware of this and administer Atropine as needed to correct the bradicardia and prevent dangerous cardiac arrest.
Results
Painful attacks are immediately abolished in 82-100% of cases (mean 96%). Long-term effect has been found in 54-91% of cases (mean 67%), with a rate of recurrence at 5 years between 20 and 30%. Postoperative facial numbness is present in most of the patients, but often resolves within 3 months [38]. Stable sensory deficits, usually mild, remain in 20-35% of patients. The rate of dysesthesias is between 1.5% and 5%, and decreases with the decreasing compression time. Anesthesia dolorosa, loss of corneal reflex, and keratitis are exceptional. Postoperative masseter and masticatory muscles weakness is common, but in about 90-95% of cases resolves within few weeks or months [39,40]. Mortality is less than 2 every 1,000 cases, due to carotid lesion.
Stereotactic radiosurgery
After the first experience of Leksell [41], at the end of the 1990’s the MRI visualization of the trigeminal root has allowed to precisely define a beam for its stereotactic irradiation. Then the treatment of TN by Stereotactic Radiosurgery (SRS) has been growing exponentially, being the least invasive neuroablative procedure for TN.
Technique
Under the guide of MRI or High Definition CT scan, SRS is performed either by Gamma Knife [42], requiring the positioning of a stereotactic frame, or, more recently, by Cyberknife [43], not requiring the stereotactic frame. The target is usually chosen in the cysternal portion of the trigeminal root, between 2 and 14 mm anterior to the emergency of the nerve from the pons. The dose used varies from 60 to 90 Gy, with best effects obtained by doses between 80 and 90 Gy.
Results
As indicated in the four more recent and with a wider patients population reports [44-47] (Table 2), the effect on pain is usually obtained after a mean of 1-6 months after the treatment. Mean followup is between 21 and 44 months. Early pain free patients (at 6 moyhs-1 year) are 75-92%, at 5 years 46-65% (mean 50%). Sensory deficits, usually mild, remain stable in 10-42% of patients, and major dysesthesias appear in 0-4%. Infrequently masticator weakness, diplopia, and decreasing hearing are reported. Higher radiation doses and treating longer segments of the trigeminal nerve has been identified as the cause of increased side effects [48]. Repeated radiosurgery is associated with a slightly decreasing pain relief and increasing facial numbness.
Indications of surgical treatments
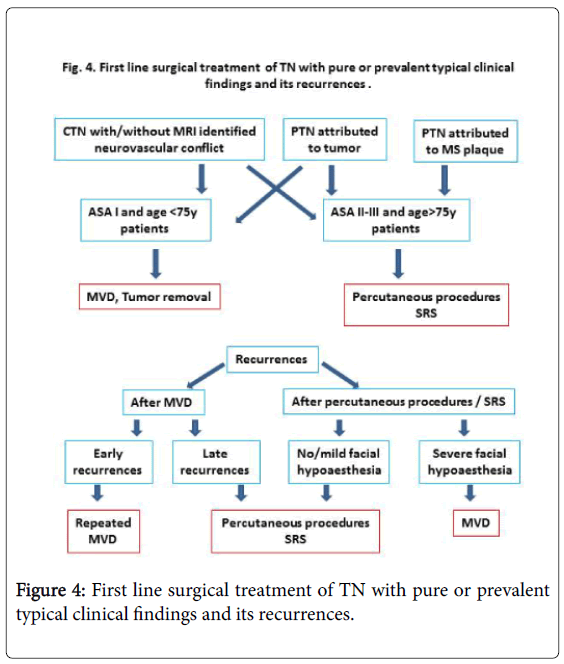
Nowadays a large consensus about the indications of the surgical treatment of TN has been achieved between Neurologists, Pain Therapists and Neurosurgeons [29,49,50] (Figure 4). This in spite of a well-recognized need for further studies better fulfilling the criteria of evidence based medicine [51].
Surgical treatment of TN is indicated when the following criteria are satisfied:
A well-established clinical diagnosis of CTN has been made. This is usually easy, but in cases of either some inveterate neuralgia bearing atypical features (prolonged and burning pain, sensory deficits, etc.) or patients that is not able to adequately report the characters of their painful attacks. Most of the Authors agree that the surgical treatment is not indicated when atypical findings are prevalent. This is mainly the case of PTN. Actually in these cases the results are quite disappointing and the risk of collateral effects (deafferentation pain) is high. Therefore the neuromodulation procedures should be considered.
TN is disabling, that is it affects the patient by frequent painful attacks without prolonged remission periods, in spite of a correct pharmacological treatment.
The pharmacological treatment is not effective at well tolerated doses, that is the pain is not sufficiently controlled and/or the collateral effects of the drugs does affect the quality of life by marked asthenia, cognitive deterioration, instability, gastrointestinal and blood cells disorders.
Most of the Authors agree that the surgical treatment should be proposed early in the history of the disease, to prevent an irreversible damage of the trigeminal fibers and a central self-sustaining sensitization of trigeminal neurons, both causing recurrences of pain attacks after the surgical treatment. Furthermore early surgery relieves the patients from avoidable sufferings.
Due to the different etiology of TN, any patient should undergo a correctly performed MRI study at the beginning of the disease, to define an “Etiology established TN”. This could be achieved in 100% of cases when the cause of TN is multiple sclerosis, cerebello-pontine angle tumors, cavernomas of the pons, aneurysms and arteriovenous malformations. This is not the case of the neurovascular conflict. Only the reports utilizing high-resolution MRI and performed by expert neuroradiologists with special sequences can correctly visualize the conflict in 84-96% of cases [52,53]. Sensitivity and specificity is much lesser in most of the current available MRI examinations. Therefore the neurosurgical decision should be made firstly following the clinical diagnosis of CTN and patients with eventually negative MRI surgically explored for a highly probable neurovascular conflict. On the other hand patients with not well established diagnosis should not be operated on also if they show an “apparent” positive MRI.
The further step is to choose the first surgical treatment that has to be used in any specific case.
MVD is the treatment of choice in patients being good surgical candidates, that is they are less than 70-75 years old without significant systemic diseases (grade 1 of American Society of Anesthesiology scale). This procedure assures the best long-term results without damaging the trigeminal root. The surgical risks are minimal in experienced hands.
Percutaneous techniques are indicated in poor surgical candidates: patients more than 70-75 years old or affected by significant systemic diseases (ASA 2-3). They are indicated also in patients with multiple sclerosis and in patients with not surgically removable tumors compressing the trigeminal root. The choose of the percutaneous technique largely depends on the surgeon’s experience. A well conducted RFT is the procedure offering the best long-term results. GR gives a relatively less probabilities of short and long-term results on pain, but has few risks of post-operative marked sensory deficits if the glycerol injection is prudentially graduated. PBC is the easiest to perform in the correct way, gives less distress to the patient and guarantees results on pain quite as good as the RFT, with less risks of marked sensory deficits, mainly when neuralgia affects the first trigeminal division. The results may be disappointing in patients with a wide Meckel’s cave.
SRS is reaching satisfying results, but not yet so good as the results of RFT and PBC. The main drawback is the late appearance of its effect on pain, sometime of few months, unacceptable for patient in severe pain because of a drug-resistant TN. Furthermore many Radiotherapists utilize low doses of radiations for safety reasons, and this can lower the long term effects of the procedure. In any case SRS is until now the newest and most attractive neuroablative procedure.
When a recurrence of painful attacks appears the pharmacological treatment is restarted. Again only if it becomes ineffective at tolerable doses the surgical treatment should be reconsidered.
In case of recurrence after MVD a new exploration of the trigeminal root in posterior fossa can be performed, to rule out that an incomplete decompression has been performed at the first operation. This is the case, for instance, when the pain recurs early. In late recurrences the decision is more difficult, because late re-explorations offers more technical difficulties due to thick arachnoidal adhesions surrounding the trigeminal root, mainly if the Teflon has been used. This increases the risk of surgical damage to the trigeminal root and the nearby positioned cranial nerves. In this case most of the Authors prefer to choose a percutaneous techniques or SRS.
In case of recurrence after percutaneous techniques or SRS it is important to consider if a facial hypoesthesia is still present. When no or only slight sensory deficits are detectable, the same or another percutaneous procedure can be repeated. Also Radiosurgery option can be considered. If a marked sensory deficit is still present MVD should be considered. The increased surgical risk often overcomes the risk of a deafferentation neuralgia caused by repeated neuroablative procedures. Also in patients with multiple sclerosis in quite good general and neurological condition MVD should be offered as a second option of surgical treatment of TN, mainly if MRI is positive for neurovascular conflict. Actually some experience has shown good results, because vascular conflict can be an additional cause of their TN [54].
Conclusions
The surgical treatment is often curative in most of the patients affected by invalidating TN, not controlled by a well-tolerated pharmacological treatment. The surgical risk either of trigeminal damage (and consequent deafferentation trigeminal neuralgia) or significant neurological and general complications is very low using the modern techniques in experienced hands.
The surgical options should be offered to the patients with pure or prevalent typical clinical findings of TN and performed early in the natural history of the disease, either to improve the quality of life than to avoid an irreversible damage to the trigeminal root and a selfsustaining sensitization of trigeminal neurons. On the other hand surgery should be cautiously considered as much as the atypical clinical findings are evident.
MVD is the first choice treatment in case of CTN patients in good general conditions, giving the best chance that the pain is abolished all along their life without any neurological deficit. Percutaneous techniques and Stereotactic Radiosurgery are the first choice treatment in PTN attributed to MS or tumor and in CTN patients at risk for major surgery. These procedures allow to reach a satisfying percentage of patient with their pain abolished without or with minimal trigeminal sensory deficits.
References
- Tatli M, Satici O, Kanpolat Y, Sindou M (2008) Various surgical modalities for trigeminal neuralgia: literature study of respective long-term outcomes. Acta Neurochir (Wien) 150: 243-255.
- Zakrzewska JM, Coakham HB (2012) Microvascular decompression for trigeminal neuralgia: update. Curr Opin Neurol 25: 296-301.
- Besi E, Boniface DR, Cregg R, Zakrzewska JM (2015) Comparison of tolerability and adverse symptoms in oxacarbazepine and carbamazepine in the treatment of trigeminal neuralgia and neuralgiform headaches using the Liverpool Adverse Events Profile (AEP). J Headache Pain 16: 563.
- Headache Classification Committee of the International Headache Society (IHS) (2013) The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33: 629-808.
- Patel SK, Liu JK2 (2016) Overview and History of Trigeminal Neuralgia. Neurosurg Clin N Am 27: 265-276.
- Burchiel KJ (2003) A new classification for facial pain. Neurosurgery 53: 1164-1166.
- Cruccu G, Finnerup NB, Jensen TS, Scholz J, Sindou M, et al. (2016) Trigeminal neuralgia: New classification and diagnostic grading for practice and research. Neurology 87: 220-228.
- Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, et al. (2008) Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 70: 1630-1635.
- Parmar VK, Gee L, Smith H, Pilitsis JG (2014) Supraspinal stimulation for treatment of refractory pain. Clin Neurol Neurosurg 123: 155-163.
- Maniam R, Kaye AD, Vadivelu N, Urman RD (2016) Facial Pain Update: Advances in Neurostimulation for the Treatment of Facial Pain. Curr Pain Headache Rep 20: 24.
- Hodaj H, Alibeu JP, Payen JF, Lefaucheur JP (2015) Treatment of Chronic Facial Pain Including Cluster Headache by Repetitive Transcranial Magnetic Stimulation of the Motor Cortex With Maintenance Sessions: A Naturalistic Study. S Brain Stimul 8: 801-807.
- Canavero S, Bonicalzi V, Clemente M (2006) No neurotoxicity from long-term (>5 years) intrathecal infusion of midazolam in humans. J Pain Symptom Manage 32: 1-3.
- Chua NH, Halim W, Beems T, Vissers KC (2012) Pulsed radiofrequency treatment for trigeminal neuralgia. Anesth Pain Med 1: 257-261.
- Pagni CA (1993) The origin of tic douloureux: a unified view. J Neurosurg Sci 37: 185-194.
- Devor M, Amir R, Rappaport ZH (2002) Pathophysiology of trigeminal neuralgia: the ignition hypothesis. Clin J Pain 18: 4-13.
- Obermann M, Yoon MS, Ese D, Maschke M, Kaube H, et al. (2007) Impaired trigeminal nociceptive processing in patients with trigeminal neuralgia. Neurology 69: 835-841.
- Watson JC (2007) From paroxysmal to chronic pain in trigeminal neuralgia: implications of central sensitization. Neurology 69: 817-818.
- DeSouza DD, Hodaie M, Davis KD (2014) Abnormal trigeminal nerve microstructure and brain white matter in idiopathic trigeminal neuralgia. Pain 155: 37-44.
- Costigan M, Scholz J, Woolf CJ (2009) Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci 32: 1-32.
- Brown JA, Hoeflinger B, Long PB, Gunning WT, Rhoades R, et al. (1996) Axon and ganglion cell injury in rabbits after percutaneous trigeminal balloon compression. Neurosurgery 38: 993-1003.
- Lunsford LD, Bennet MH, Martinez AJ (1995) Experimental trigeminal glycerol injection. Electrohysiologic and morphologic effects. Arch Neurol 42: 146-49.
- Sweet WH, Wepsic JC (1974) Controlled thermocoagulation of trigeminal ganglion and rootlets for differential destruction of pain fibers. Part 1: Trigeminal neuralgia. J Neurosurg 40: 143-156.
- Frigyesi TL, Siegfried J, Broggi G (1975) The selective vulnerability of evoked potentials in the trigeminal sensory root of graded thermocoagulation. Exp Neurol 49: 11-21.
- Dandy WE (1932) The treatment of trigeminal neuralgia by the cerebellar route. Ann Surg 96: 787-795.
- Jannetta PJ (1997) Outcome after microvascular decompression for typical trigeminal neuralgia, hemifacial spasm, tinnitus, disabling positional vertigo, and glossopharyngeal neuralgia (honored guest lecture). Clin Neurosurg 44: 331-383.
- McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, et al. (1999) Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg 90: 1-8.
- Pagni CA, Fariselli L, Zeme S (2008) Trigeminal neuralgia. Non-invasive techniques versus microvascular decompression. It is really available any further improvement?. Acta Neurochir (Wien) Suppl 101: 27-33.
- Sindou M, Keravel Y, Simon E, Mertens P (2005) Névralgie du trijumeau et neurochirurgie. EMC, Neurologie 17-25.
- Zakrzewska JM, Linskey ME (2014) Trigeminal neuralgia. BMJ Clin Evid 2014.
- Barker FG, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD (1996) The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 334: 1077-1083.
- Sindou M, Leston J, Howeydi T, Decllier E, Chauis F (2006) Microvascular decompression for rimary trigeminal neuralgia (typical or atypical). Long-term effectiveness on pain: prospective study with survival analysis in a consecutive series of 361 patients. Acta Neurochir (Wien) 148: 1235-1245.
- Taha J (2004) Trigeminal Neuralgia: Percutaneous Procedures. Seminars in Neurosurgery 15(2/3): 115-34.
- Bender MT, Bettegowda C (2016) Percutaneous Procedures for the Treatment of Trigeminal Neuralgia. Neurosurg Clin N Am 27: 277-295.
- Hakanson S (1981) Trigeminal neuralgia treated by the injection of glycerol into the trigeminal cistern. Neurosurgery 9: 638-646.
- Saini SS (1987) Retrogasserian anhydrous glycerol injection therapy in trigeminal neuralgia. Observations on 552 patients. J Neurol Neurosurg Psychiatry 80: 1536-38.
- Bender M, Praduillo G, Batra S, See A, Bhutiani N, et al. (2012) Effectiveness of repeat glycerol rhizotomy in treating recurrent trigeminal neuralgia. Neurosurgery 70: 1125-1133.
- Mullan S, Lichtor T (1983) Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia. J Neurosurg 59: 1007-1012.
- Skirving DJ, Dan NG (2001) A 20-year review of percutaneous balloon compression of the trigeminal ganglion. J Neurosurg 94: 913-917.
- Lichtor T, Mullan JF (1990) A 10-year follow-up review of percutaneous microcompression of the trigeminal ganglion. J Neurosurg 72: 49-54.
- Abdennebi B, Guenane L (2014) Technical considerations and outcome assessment in retrogasserian balloon compression for treatment of trigeminal neuralgia. Series of 901 patients. Surg Neurol Int 5: 118.
- Leksell L (1971) Sterotaxic radiosurgery in trigeminal neuralgia. Acta Chir Scand 137: 311-314.
- Rand RW, Jacques DB, Melbye RW, Copcutt BG, Levenick MN, et al. (1993) Leksell Gamma Knife treatment of tic douloureux. Sterotact Funct Neurosurg 61(Suppl 1): 93-102.
- Romanelli P, Heit G, Chang SD, Martin D, Pham C, et al. (2003) Cyberknife radiosurgery for trigeminal neuralgia. Stereotact Funct Neurosurg 81: 105-109.
- Regis J, Tuleasca C, Resseguier N, Carron R, Donnet A, et al. (2016) Long-term safety and efficacy of Gamma Knife surgery in classical trigeminal neuralgia: a 497-patient historical cohort study. J Neurosurg 124: 1079-1087.
- Kondziolka D, Zorro O, Lobato-Polo J, Kano H, Flannery TJ, et al. (2010) Gamma Knife stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg 112: 758-765.
- Lucas JT, Nida AM, Isom S, Marshall K, Bourland JD, et al. (2014) Predictive monogram for the durability of pain relief from gamma knife radiation surgery in the treatment of trigeminal neuralgia. Int J Radiat Oncol Biol Phys 89: 120-126.
- Marshal K, Chan MD, McCoy TP, Aubuchon AC, Bourland JD, et al. (2012) Predictive variables for the successful treatment of trigeminal neuralgia with gamma knife radiosurgery. Neurosurgery 70: 566-572.
- Villavicencio AT, Lim M, Burneikiene S, Romanelli P, Adler JR, et al. (2008) Cyberknife radiosurgery for trigeminal neuralgia treatment: a preliminary multicenter experience. Neurosurgery 62: 647-55.
- Sindou M, Keravel Y, Laurent B (2014) Aspects cliniques et therapeutiques des nevralgies essentielles du trijumeau et du glossopharingien. EMC-Neurologie 11:1-21.
- Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, et al. (2008) AANS-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol 71: 1183-1190.
- Zakrzewska JM, Relton C (2016) Future Directions for Surgical Trial Designs in Trigeminal Neuralgia. Neurosurg Clin N Am 27: 353-363.
- Leal PR, Hermier M, Froment JC, Souza MA, Cristino-Filho G, et al. (2010) Preoperative demonstration of the neurovascular compression characteristics with special emphasis on the degree of compression, using high-resolution magnetic resonance imaging: a prospective study, with comparison to surgical findings, in 100 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Acta Neurochir (Wien) 152: 817-825.
- Hitchon PW, Zanaty M, Moritani T, Uc E, Pieper CL, et al. (2015) Microvascular decompression and MRI findings in trigeminal neuralgia and hemifacial spasm. A single center experience. Clin Neurol Neurosurg 139: 216-220.
- Broggi G, Ferroli P, Franzini A, Nazzi V, Farina L, et al. (2004) Operative findings and outcome of microvascular decompression for trigeminal neuralgia in 35 patients affected by multiple sclerosis. Neurosurgery 55: 830-839.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 18462
- [From(publication date):
specialissue-2016 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 17274
- PDF downloads : 1188