Review Article Open Access
The Sleeping Stimuli of Oral Cavity
Khushboo Rastogi1 and Rajul Rastogi2*
1Department of Dentistry, Saraswathi Institute of Medical Sciences, Hapur, Uttar Pradesh, India
2Department of Radiodiagnosis, Teerthanker Mahaveer Medical College and Research Center, Moradabad-244001, Uttar Pradesh, India
- *Corresponding Author:
- Rastogi R
Assistant Professor
Department of Radiodiagnosis
Teerthanker Mahaveer Medical College
and Research Center
Moradabad-244001
Uttar Pradesh, India
E-mail: eesharastogi@gmail.com
Received Date: November 05, 2016 Accepted Date: December 19, 2016 Published Date: December 26, 2016
Citation: Rastogi K, Rastogi R (2016) The Sleeping Stimuli of Oral Cavity. Pediatr Dent Care 1: 126.
Copyright: © 2016 Rastogi K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Several silent changes occurring in our dietary habits are apparently sleeping for decades before becoming active. These changes are responsible for severe mucosal and tissue changes affecting lifecycle of oral cavity. These alterations force us to seek medical and dental attention. The purpose of this article is to create awareness among the clinicians and patients about these sleeping stimuli for optimal prevention of these related medical and dental problems.
Keywords
Cusp; Dentinal hypersensitivity; Gingivitis; Periodontitis; Sleeping stimuli
Introduction
A healthy periodontium is stated when there are no gingival and tissue changes seen in the oral cavity. There are several features of healthy gingiva including coral pink colour with no signs of bleeding and inflammation, proper scalloping and contour, thus determining healthy tooth support. Any change in the dietary and food habits can trigger changes in oral mucosa resulting in major alterations in oral cavity. Sleeping stimuli can be defined as those stimuli or points which are present in oral cavity and once triggered cause severe damage to the periodontium. These stimuli are sharp tooth cusp due to improper dietary habits which can cause acidic pH resulting in abrasion; improper brushing habits which can lead to caries, irreversible and reversible pulpitis, abscesses and cysts; extreme hot and cold intake resulting into dentinal hypersensitivity, increased clenching of teeth due to hypertension and habits like smoking and tobacco chewing resulting into periodontal and mucosal changes [1].
Sharp Cusp or Teeth under Constant Trauma
Oral cavity cancer involves five significant and potent “S” - smoking, spirits (alcohol), syphilis, spices and sharp teeth [2]. The role of chronic dental trauma on the mucosa of oral cavity has only been included in few case studies and has never been well elucidated. In one previous study, it was observed that the edge of the tongue, a site for potential dental trauma accounted for 35% of oral cavity cancers in smoker patients [3]. In a 10 year study conducted in Queensland in the year-2011, it was observed that non-smoking women developed oropharyngeal cancer in only 12 cases but 53 women developed oral cancer on the edge of the tongue where teeth were having sharp cusp [4]. In another retrospective study, it was observed that several premalignant conditions were cured within 2-3 weeks when the traumatized tooth was relieved from trauma [5]. Abnormal positioning of teeth also plays an important role in creating sharp cusps thus indicating the importance of treating sharp cusp teeth.
Dental Erosion due to Altered Dietary Habits
Dental erosion is defined as the loss of dental hard tissue, associated with extrinsic and / or intrinsic acid that is not produced by bacteria [6]. Dental erosion is common and its prevalence has increased tremendously in recent years [7]. The prevalence varies in literature; however the median prevalence of dental erosion is 34.1% in children and 31.8% in adults [8-11]. Dental erosion is caused by a direct contact between tooth surfaces and acidic substances. In a previous study it was observed that demineralization of dental enamel occurs when the oral environment pH crosses the critical threshold of 5.5 [12]. Clearance of acidic beverages has been found in direct relationship with salivary flow rate. In another study, it was observed that reduced salivary flow rate and decreased buffering capacity of saliva resulted in accelerated erosive process of enamel [13]. However intrinsic acids released via gastro-intestinal disturbances also causes significant dental erosion. A thorough evaluation of dietary habits was found to be effective in assessing the erosive potential of several food stuffs. These several food stuffs are listed below in the given tables (Tables 1 and 2) added from a source [14-16].
| Fruits | pH | Fruits | pH |
|---|---|---|---|
| Apples | 2.9-3.5 | Cranberry sauce | 2.3 |
| Apricots | 3.2-3.6 | Fruit jams/jellies | 3.0-4.0 |
| Blueberries | 3.2-3.5 | Italian salad dressing | 3.3 |
| Cherries | 3.2-4.7 | Ketchup | 3.7 |
| Grapes | 3.3-4.5 | Mayonnaise | 3.8-4.0 |
| Grapefruits | 3.0-3.5 | Mustard | 3.6 |
| Lemon/Limes | 1.8-2.4 | Pickles | 2.5-3.0 |
| Oranges | 2.8-4.0 | Relish | 3.0 |
| Peaches | 3.1-4.2 | Rhubarb puree | 2.8 |
| Pears | 3.4-4.7 | Sauerkraut | 3.1-3.7 |
| Pineapples | 3.3-4.1 | Sour cream | 4.4 |
| Plums | 2.8-4.6 | Tomatoes | 3.7-4.7 |
| Raspberries | 2.9-3.7 | Fermented vegetables | 3.9-5.1 |
| Strawberries | 3.0-4.2 | Yogurt | 3.8-4.2 |
Table 1: pH values of common food stuffs.
| Drinks | pH |
|---|---|
| Coke | 2.7 |
| Pepsi | 2.7 |
| Seven-up | 3.2-3.5 |
| Sprite | 2.6 |
| Mountain dew | 3.2 |
| Dr. Pepper | 2.9 |
| Lemon nestea | 3.0 |
| Root beer | 3.0-4.0 |
| Ginger ale | 2.0-4.0 |
| Orange juice | 3.4 |
| Grapefruit juice | 3.2 |
| Cranberry juice | 2.3-2.5 |
| Apple juice | 3.4 |
| Pineapple juice | 3.4 |
| Kiwi juice | 3.6 |
| Grape juice | 3.4 |
| Carrot juice | 4.2 |
| Beetroot juice | 4.2 |
| Iced tea | 3.0 |
| Fanta orange | 2.9 |
| Red bull | 3.4 |
| Gatorade | 3.3 |
| Isostar | 2.4-3.8 |
| Coffee | 2.4-3.3 |
| Black Tea | 4.5 |
| Beer | 4.0-5.0 |
| Wine | 2.3-3.8 |
Table 2: pH values of common beverages.
Improper brushing also triggers this reaction, hence correct preventive measures like proper and appropriate method of brushing along with proper dietary intake will prevent this sleeping stimulus to cause abrasion [17].
Dentinal Hypersensitivity (DH)
Dentin hypersensitivity has been defined as a short, sharp pain arising from exposed dentin in response to stimuli- typically thermal, evaporative, tactile, osmotic or chemical and which cannot be ascribed to any other dental defect or disease (Canadian Advisory Board on Dentin hypersensitive teeth,2003) [18]. DH is a widespread condition with a reported prevalence varying from as low as 4.5% to as high as 57% (Cummins) [19]. The commonly involved sites are buccal cervical regions and occlusal/buccal sites, mostly found in young adults. Sometimes, the patient is too sensitive and cannot undergo even minor surgical procedure. DH is mainly caused by an external stimulus which acts over exposed dentinal tubules creating a pressure that triggers pain. Hence, it is important for the clinician to make the patients aware against this sleeping stimulus which can cause extreme discomfort to the patient.
Gingivitis and Periodontitis
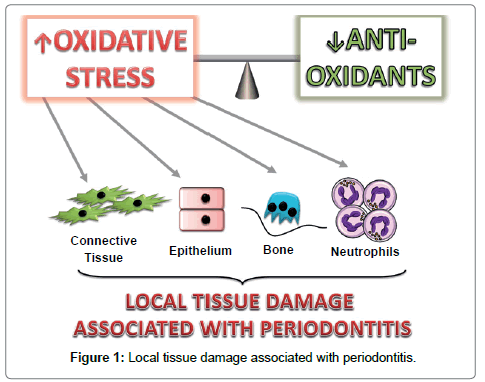
Dietary changes have significant influence over microflora of oral cavity which once altered results in gingivitis and periodontitis. Gingivitis is defined as the inflammation of the gingiva which is a non-destructive form of periodontitis [20]. Large sugary intake alters the flora of the oral cavity that contributes to the growth of dental plaque which has the potential to cause inflammation associated with periodontal disease. Research studies have shown using an experimental gingivitis model that there were increased levels of bleeding on probing when participants were fed with rich carbohydrate diet as compared to individuals with low carbohydrate [21]. Another study supported this by investigating volunteers placed on a primitive diet which was high in fibre, anti-oxidants, and fish oils but were low in refined sugars and with no oral hygiene measures resulting into increased plaque levels but with reduced gingival bleeding from 35% to 13%.22 However till date, few elucidative studies exists on the mechanism of dietary effect on periodontium. Oxidative stress is found to be an important link between periodontitis and systemic disease. If this fine balance gets altered by excess production of oxidants and /or depletion of local antioxidants, the resulting oxidant excess causes oxidative stress resulting in local tissue damage as seen in periodontitis (Figure 1) [23].
Hence, sugary diet in the form of sucrose is a sleeping trigger for the alteration of flora of oral cavity which can be prevented with adequate awareness.
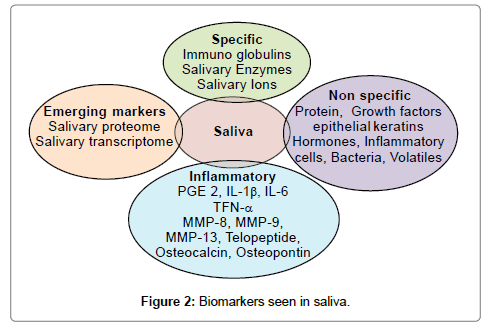
Gustatory Saliva
Saliva plays an important role in the digestion, lubrication and diagnosis of underlying major systemic disease. Its alteration can occur in many systemic diseases like xerostomia, hypothyroidism, diabetes mellitus, etc. leading to various oral diseases including dental caries & periodontitis. Hence, it becomes all the way more important to diagnose a disease as early as possible as most of the systemic diseases gets diagnosed only when morbid symptoms become apparent in the late phase. To overcome this, it is important to find molecular disease biomarkers that are able to reveal a hidden lethal threat even before the disease becomes apparent. Saliva is one such diagnostic tool which is becoming popular due to its easy approachability and handling. Proposed salivary diagnostic markers are serum and salivary molecules such as immunoglobulins, enzymes constituents of gingival crevicular fluid, bacterial components or products, volatile compounds and phenotypic markers such as epithelial keratins (as shown in Figure 2) [24]. Many studies have attempted to determine a relationship between salivary levels of secretory IgA and various forms of periodontal diseases. Eggert et al. reported that saliva from treated periodontitis patients had higher IgA and IgG levels to periodontal pathogens Porphyromonas gingivalis and Treponema denticola than as compared to saliva from control subjects [25]. Sandholm et al. found increased concentrations of salivary IgG to Aggregatibacter actinomycetemcomitans in patients of aggressive periodontitis [26] (Figure 2).
Antioxidative Capacity of Saliva
Physiologically free radical/reactive oxygen species in the mouth are derived mainly from polymorphonuclear neutrophils (PMN), which may also help to control bacterial growth by the well-known ‘‘respiratory burst’’ (RB). Such physiological processes are usually efficiently counteracted by intrinsic antioxidant systems: if such systems fail, tissue damage results [27].
Saliva may constitute a first line of defence against free radicalmediated oxidative stress, since the process of mastication promotes a variety of such reactions, including lipid peroxidation [28]. Moreover, during gingival inflammation, gingival crevicular fluid (GCF) flow increases, adding to saliva with products from the inflammatory response. This is why the antioxidant capacity of saliva is of increasing interest. Saliva is an important antioxidant having uric acid in abundance followed by lesser contribution from albumin, ascorbate and glutathione [29]. The use of saliva for translational and clinical application has emerged in the form of salivary proteomes and transcriptomes for early diagnosis, disease progression and therapeutic monitoring which provide an important platform for the diagnosis of fatal diseases like oral cancer and Sjogren’s syndrome. Thus these upcoming markers are stage-set to provide a definitive platform for keeping an eye on the triggering of these sleeping stimuli.
Improper Brushing
Improper brushing plays a key role in development of almost all diseases related to oral cavity. Abrasion, erosion, dental caries, gingivitis and periodontitis are often the result of improper brushing, in addition to other factors. In one study, it was observed that improper brushing plays a key role in developing all the major diseases of oral cavity [17]. Hence; it is extremely important to educate the patient and clinician against this sleeping stimulus that trigger such conditions.
Conclusion
To summarize, proper education and awareness of the patient and the clinician about the sleeping stimuli of oral cavity can go a long way in maintaining good oral health and preventing common dental and gingival diseases.
References
- Saraswathi TR, Ranganathan K, Shanmugams (2006) Prevalence of oral lesion in relation to habits. Cross-sectional study. Ind J Dent Res 17: 121-25.
- Perry BJ, Zammit AP, Lewandowski AW (2015) Sites of origin of oral cavity cancer in non-smokers vs smokers: Possible evidence of Dental trauma carcinogenesis and its importance compared with Human papilloma virus. JAMA Otolaryngeal Head Neck Surg 141: 5-11.
- American Cancer Society (2016) Cancer Facts & Figures 2016 Atlanta: American Cancer Society.
- Perry C (2011) Study of oral and oropharyngeal cancer in non-smoker women. Quennsland Scand. Jr 141: 6-9.
- Scully C, Felix DH (2005) Oral Medicine- update for the dental practitioner. Brit. Dent. Jr 199: 565-72.
- Ren FY (2011) Dental erosion: etiology, diagnosis and prevention ADA CERP 77-81.
- Jaeggi T, Lussi A (2006) Prevalence, incidence and distribution of erosion. Monographsin Oral Sci 20: 44-65.
- Dugmore CR, Rock WP (2003) The progression of tooth erosion in a cohort of adolescents of mixed ethnicity. Int. J Paediatr Dent 13 (5): 295-303.
- El Aidi H, Bronkhorst EM, Truin GJ (2008) A longitudinal study of tooth erosion in adolescents. J. Dent Res 87: 731-5.
- Lussi A, Schaffner M (2000) Progression of and risk factors for dental erosion and wedge-shaped defects over a 6-year period. Caries Res 34: 182-7.
- Lussi A, Schaffner M, Hotz P, Suter P (1991) Dental erosion in a population of Swiss adults. Comm Dent Oral Epidemiol 19: 286-90.
- Hicks J, Garcia-Godoy F, Flaitz C (2005) Biological factors in dental caries enamel structure and the caries process in the dynamic process of demineralization and remineralisation (part 2). J Clin Pediatr Dent 29: 119-24.
- Moazzez R, Smith BG, Bartlett D (2000) Oral pH and drinking habit during ingestion of a carbonated drink in a group of adolescents with dental erosion. J Dent 28: 395-7.
- Clark DC, Woo G, Silver JG, Sweet D, Grisdale JC (1990) The influence of frequent ingestion of acids in the diet on treatment for dentin sensitivity. J Can Dent Assoc 56:1101-03.
- Jain P, Nihil P, Sobkowski J, Agustin MZ (2007) Commercial soft drinks :pH and in vitro dissolution of enamel. Gen. Dent 55:150-155.
- Lussi A, Jeggi T (2006) Chemical factors. Monographs Oral Sci 20: 77-87.
- Addy M, Hunter ML (2003) Can toothbrushing damage your health? Effects on oral and dental tissues. Int Dent Jr 3: 12-14.
- Walters PA (2005) Dentinal Hypersensitivity. A Review. Jr. Contemp Dent Pract 6: 107-17.
- Cummins D (2009) Dentin Hypersensitivity: From diagnosis to a breakthrough therapy for a everyday sensitivity relief. J Clin Dent 20: 1-9.
- The American Academy of Periodontology (1989) Proceedings of the world workshop in clinical periodontics. Chicago: The American Academy of Periodontology 1: 23-24.
- Sidi A, Ashley E (1984) Influence of frequent sugar intakes on experimental gingivitis. J Periodontol 55:419-423.
- Baumgartner S, Imfeld T, Schicht O (2009) The impact of the stone age diet on gingival conditions in the absence of oral hygiene. J. Periodontol 80: 759-768.
- Sies H, Jones DP (2007) Oxidative stress. Encyclopedia of stress. San Diego: Elesvier.
- Patil PB, Patil BR (2011) Saliva: A diagnostic biomarker of periodontal diseases. J Indian Soc Periodontol 15: 310-317.
- Eggert FM, Maenz L, Tam YC (1987) Measuring the interaction of human secretory glycoproteins to oral bacteria. J Dent Res 66: 610-612.
- Sandholm L, Tolo K, Olsen I (1987) Salivary IgG, a parameter of periodontal disease activity? High responders to actinobacillus actinomycetemcomitans Y4 in juvenile and adult periodontitis. J Clin Periodontol 14: 289-94.
- Sandholm L, Tolo K, Olsen I (1987) Salivary IgG, a parameter of periodontal disease activity? High responders to actinobacillus actinomycetemcomitans Y4 in juvenile and adult periodontitis. J Clin Periodontol 14: 289-94.
- Battino M, Ferreiro MS, Gallardo I, Newman HN, Bullon P (2002) The antioxidant capacity of saliva. J Clin Periodontol 29: 189-94.
- Terao J, Nagao A (1991) Antioxidative effect of human saliva on lipid peroxidation. Agr Biol Chem 55: 869-72.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 4528
- [From(publication date):
specialissue-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 3602
- PDF downloads : 926