The SIX Cs model for Immediate Cognitive Psychological First Aid: From Helplessness to Active Efficient Coping
Received: 01-Jan-1970 / Accepted Date: 01-Jan-1970 / Published Date: 30-Jun-2018 DOI: 10.4172/1522-4821.1000395
Abstract
Acute stress reactions immediately after exposure to trauma or crisis have received growing attention in recent years and are gaining momentum in light of recent mass traumatic events worldwide including conflicts, terrorist attacks and natural disasters. Unlike routine life, traumatic or emergency situations are unexpected and unstructured events. Early helping responses in these situations is of utmost importance: immediate, focused and efficient interventions are beneficial for the reduction of acute stress reactions and a return to normal functioning as well as decreasing the risk for future onset of post-traumatic stress disorder symptoms. However, many early efforts were either found to be ineffective or are based on narrative expression and empathy alone. The aim of this paper is to present the SIX Cs model - a new psychological first aid approach - immediate cognitive-functional psychological first aid - for the global nonprofessional community as well as for first responders. The model addresses the need to standardize interventions during an Acute Stress Reaction and intends to help shift the person from helplessness & passiveness into active effective functioning, within minutes, in the immediate aftermath of a perceived traumatic event. The model is based on four theoretical and empirically tested concepts: (1) Hardiness, (2) Sense of Coherence, (3) Self-Efficacy, and (4) on the Neuro-psychology of the stress response, focusing on shifting people from a limbic system hyperactivity to a prefrontal cortex activation during stressful events. Preliminary results on the effectiveness of the SIX Cs model in terms of increasing resiliency, reducing anxiety and improving perceived self-efficacy are presented. To date, this approach has been recognized by the Israeli Ministry of Health as the Israeli national model for psychological first aid.
Keywords: Traumatic stress, Psychological first aid, Self-efficacy, Resilience, Cognitive-functional first aid
Introduction
Acute Stress reactions immediately after exposure to trauma or crisis have received growing attention in recent years (Rowlands, 2013) and are gaining momentum in light of recent mass traumatic events worldwide including conflicts, terrorist attacks and natural disasters.
Perception of an event as a potentially traumatic event (e.g., traffic accident, injury, terror attacks, and natural disasters) is rooted in the individual’s feelings of fear, sense of threat and subsequent sense of helplessness (ICD-10) (World Health Organization, 2015). Furthermore, the event may be perceived as traumatic depending on the cognitive appraisals and fear responses people experience during or soon after exposure to such events. The pioneering study of Speisman et al. (Speisman, Lazarus, Mordkoff, & Davison, 1964) demonstrated the causal role cognitive appraisals have in determining the stress response. More recent studies have shown the role of appraisal using other methods and participants including affecting distress and emotion-modulating brain regions (Buhle et al., 2014; Gidron & Nyklicek, 2009; Goldin, McRae, Ramel, & Gross, 2008; Lazarus & Folkman, 1984; Walker, Smith, Garber, & Claar, 2005).
The natural course of post-traumatic responses following the Acute Stress Reaction (ASR, up to 48 hours after the event) could include spontaneous remission, development of Acute Stress Disorder (ASD) up to one month later, and the subsequent development of Post-Traumatic Stress Disorder (PTSD) more than a month after the event. The ASR, ASD and PTSD include the symptom clusters of intrusions, avoidance and arousal according to the ICD-10 (World Health Organization, 2015), and differ only in the timeframe ascribed to the symptoms to separate the diagnostic entities.
The incidence of ASD after a traumatic event ranges from 14% among victims of motor vehicle accidents (Harvey & Bryant, 2000) to 33% among survivors of mass shootings (Classen, Koopman, Hales, & Spiegel, 1998). However, there is a dearth of information on the incidence of the ASR, mostly due to the fact that this response needs to be assessed during the early hours or days after the event. Soldatos et al. (2006), in a study among earthquake victims, found that 85.3% of subjects fulfilled the criteria for ASR according to ICD-10 criteria (World Health Organization, 2015). In that study, 97.1% of those diagnosed with ASR went on to develop the most protracted form of the stress related disorders, PTSD, finding a significant associations between the occurrence of ASR and the development of PTSD (Soldatos et al., 2006).
It has been estimated by the Israel Home Front Command (Colonel A. Bar, personal communication, January 4, 2010) that on the micro and macro levels, the ratio between casualties suffering from physical injuries and mental health injuries is 1:4-1:8. In other words, for every individual incurring in a physical injury, four to eight others will suffer from acute anxiety and may develop an ASR, which could potentially become an ASD. Unlike routine life, traumatic or emergency situations are unexpected and unstructured events – An individual does not know where or when they will occur or who will be in need of help. Such a situation demands, among other things, instant mental health interventions and adaptation of these interventions to the particular characteristics of the event (Schreiber et al., 2004). Some authors have studied the challenges involved in early and long-term interventions to reduce distress and prevent chronic mental health problems after disasters. They concluded that evidence based mental health interventions should be in place in the immediate aftermath of a traumatic event (Dyregrov, 2008; Yule, 2006). Early response in these situations is of utmost importance. Immediate, focused and efficient interventions are beneficial for the reduction of acute stress reactions and a return to normal functioning, as well as for decreasing the risk of future onset of post-traumatic symptoms (Shapiro, 2012; Zohar, Sonnino, Juven-Wetzler, & Cohen, 2009). Furthermore, studies in both animal (Cohen, Matar, Buskila, Kaplan, & Zohar, 2008) and human (Zohar, Yahalom, et al., 2011) models have suggested that there is a window of opportunity in the immediate hours of a perceived traumatic event, to reduce anxiety and confusion, restore stability and effective coping, and that this “window of opportunity” is not wider than six hours (Cohen et al., 2008; Zohar, Yahalom, et al., 2011).
Up to this day, the only generalized approach to early intervention in the immediate aftermath of a traumatic event is Psychological First Aid (PFA). PFA is an approach built on the concept of resilience and designed to help people in the immediate aftermath of any emergency situation (Brymer et al., 2006). It was originally developed to be used by mental health and other disaster responders in emergency situations and is currently recommended by the World Health Organization (WHO) as an alternative to debriefing (World Health Organization, War Trauma Foundation, World Vision International, & 2011), the latter found in several reviews to be ineffective in preventing PTSD or even harmful (Bastos, Furuta, Small, McKenzie-McHarg, & Bick, 2015; Forneris et al., 2013). PFA is based on an understanding that people affected by traumatic events will experience early stress reactions which may cause sufficient distress to impede adaptive coping and recovery (Brymer et al., 2006; Ruzek et al., 2007). Therefore, PFA is intended to reduce the initial ASR caused by events which are perceived as traumatic and to foster short- and long-term adaptive functioning and coping.
Hobfoll (2007) recommended five core principles that should be used to guide intervention efforts in communities following exposure to crises and emergencies: (1) to foster a sense of safety, (2) to provide calmness, (3) to induce a sense of self- and community efficacy, (4) connectedness, and (5) hope. Following these principles and since the first approach to PFA was established, several guidelines have been developed worldwide such as the guidelines developed by the National Child Traumatic Stress Network and National Center for PTSD in the US (NCTSNNCPTSD (Brymer et al., 2006), the European Network for Traumatic Stress (Bisson & Tavakoly, 2008), the WHO (World Health Organization et al., 2011) and the Australian Red Cross (Burke, Richardson, & Whitton, 2013). All these guidelines share similar approaches, all based on Hobfoll’s principles, although tailored to the particular needs of the countries and frameworks in which they are to be applied. For example, the comprehensive manual developed by the WHO is stated to be applicable only for low and middle income countries.
However useful and providing a framework to intervene during the immediate hours or days after a Perceived Traumatic Event (PTE), current PFA guidelines suffer from two crucial limitations. First, as reported in a critical review, PFA guidelines lack empirical scientific evidence for their effectiveness (Dieltjens et al., 2014). This situation risks repeating the same errors done with other untested methods which were and are still provided to people soon after perceived traumatic events. Second, they were originally intended for professional teams and focus on “what to do” and “what not to do” but fall short to explain exactly “how to do it”. In the absence of a formal protocol management system, individuals (i.e., volunteers, first responders) carry out first response interventions using only their personal judgment, which may sometimes cause additional chaos beyond the event itself in the affected community (Dyregrov, 2008; Fernandez, Barbera, & Van Dorp, 2006; Hantman & Farchi, 2015). Additionally, and most importantly, to the best of our knowledge, the current guidelines for PFA are basically designed to provide supportive help, care and calmness, all of which lead to increased sense of helplessness which is one of the major triggers for PTE (ICD-10, World Health Organization, 2015). Moreover, the current protocols are provided for emergency response systems that are in place, that is, to operate only within the framework of an authorized disaster response system. In other words, they are not specifically designed to be use in the immediate minutes following an emergency event, but hours or even days after the event has occurred and once a disaster response system is in place. Such responses may be too late to reduce the ASR that follows a PTE and eventually prevent PTSD. Furthermore, PFA guidelines are not specific enough for first responders (people who attend to victims before or at the same time security or medical teams arrive at the scene), as well as any other non-professionals who are involved in the event. Such specific instructions are needed to feel competent to provide the necessary immediate emotional first aid intervention to reduce ASR symptoms and to return the person to a more functional state. In addition, as mentioned before, some of these guidelines, following Hobfoll’s and other PFA principles, put the emphasis on providing comfort, calmness and sense of safety to the victim of a PTE. These compassionate efforts may eventually increase passiveness and enhance the sense of helplessness, which is one of the main triggers for perceiving an event as traumatic (ICD- 10, World Health Organization, 2015) and predict PTSD later (Simeon, Greenberg, Nelson, Schmeidler, & Hollander, 2005).
Previous attempts at treating ASR and preventing PTSD have included psychological debriefing and treatment with benzodiazepines which have been showed to be either ineffective or even harmful (Bastos et al., 2015; Forneris et al., 2013; Zohar, Juven-Wetzler, et al., 2011). Furthermore, reviews of the effectiveness of early interventions in preventing PTSD have concluded that only Trauma Focused Cognitive-Behavioral Therapy (TF-CBT), Cognitive Behavioral Therapy (CBT) and modified prolonged exposure may help prevent PTSD (Howlett & Stein, 2016; Qi, Gevonden, & Shalev, 2016; Roberts, Kitchiner, Kenardy, & Bisson, 2010). However, their effectiveness may depend upon type of traumatic event (Rothbaum et al., 2012), and may not be helpful in all cases (Shalev et al., 2012). Yet, all the above treatments may be administered only by professional mental health workers and are not intended for immediate administration. The main aim of the above treatments is the reduction of risk for PTSD symptoms. In our perspective, the main objective of immediate interventions should be increasing one’s functional ability, and as a result, decreasing the sense of helplessness and confusion that follows the immediate minutes and hours after a PTE; subsequently, these may reduce PTSD risk in the long run.
The focus on first responders is as a consequence of their higher risk of developing negative mental health outcomes including ASD and PTSD themselves, compared to the general population, first due to their higher exposure to either natural or manmade disasters (Benedek, Fullerton, & Ursano, 2007; Sakuma et al., 2015) and second, due to their continuous exposure to traumatized populations rendering them at risk for secondary traumatic stress (STS) (Bride, 2007; Cieslak et al., 2013; Sifaki-Pistolla, Chatzea, Vlachaki, Melidoniotis, & Pistolla, 2017). However, this risk has been shown to be mediated by previous low resilience status and preparedness (Lee, Ahn, Jeong, Chae, & Choi, 2014; Sakuma et al., 2015), emphasizing the importance of developing a working model by which first responders are provided with the right and empowering tools to confront emergency situations as early as possible (Cacciatore, Carlson, Michaelis, Klimek, & Steffan, 2011).
From our point of view, ideally, just as every lay person should know how to provide basic physical emergency first aid in order to help those who are physically injured and prevent further harm before emergency teams arrive to the scene, the same should exist for PFA. There should be a common knowledge base throughout all community levels concerning brief interventions that can reduce distress sufficiently, so that each person who perceives any event as traumatic can be helped to return to normal effective functioning. The SIX Cs model was created to fill this gap and to provide a simple user-friendly working model for professionals, nonprofessionals, first responders and the general population, based on the neuropsychological and psychological correlates of stress.
The aim of this paper is to present the SIX Cs model - a new PFA approach-immediate cognitive-functional psychological first aid (ICF-PFA) designed to provide the global nonprofessional community as well as professionals and first responders, with practical tools that equip them with the necessary knowledge base and intervention skills to assist others who are currently perceiving an event as traumatic and developing ASR symptoms. The justification for the model leans on two assumptions. The first assumption, supported by recent studies, is that intervening during the first minutes/hours following the PTE provides the best “window of opportunity” for reducing an ASR and helps the person return to normal functioning (Bremner, 2006; Hantman & Farchi, 2015; Hobfoll, 2007; Schulenberg, 2016; Zohar, Juven- Wetzler, et al., 2011). The second assumption, as noted before, is that the skills needed to provide basic immediate cognitivefunctional psychological first aid (ICF-PFA) interventions should be accessible to the global nonprofessional community, as well as to professional first responders, just as basic medical first aid skills are accessible. Furthermore, teaching ICF-PFA skills to the general nonprofessional community will decrease their dependency on professional mental health personnel while increasing the independence of nonprofessionals in managing stressful events, and improving their resilience, self-efficacy and sense of trust – all leading to increased sense of safety.
The Six Cs Model
Theoretical Background
The SIX Cs model addresses the need to standardize PFA interventions during an Acute Stress Reaction (ASR) and intends to help shift the person from a helpless, passive and functional incompetent state to active effective coping, within minutes, in the immediate aftermath of a PTE. The model is based on four theoretical and empirically tested concepts: 1) Hardiness (Kobasa, 1979; Maddi, 2006); 2) Sense of Coherence (Antonovsky, 1979); 3) Self-Efficacy (Bandura, Cioffi, Taylor, & Brouillard, 1988) and; 4) on the Neuro-psychology of the stress response, specifically the interaction between the limbic system and the prefrontal cortex during stressful events (Arnsten, Mazure, & Sinha, 2012; Arnsten, 2009; Arnsten, Raskind, Taylor, & Connor, 2015; Bremner, 2006; Hendler, Rotshtein, & Hadar, 2001; Shin et al., 2004; Taylor et al., 2008).
The Concept of Hardiness
Originally introduced by Suzanne C. Kobasa in 1979 (Kobasa, 1979) and later developed by Maddi, Kobasa and colleagues (Khoshaba & Maddi, 1999; Maddi, 2006; Maddi, Khoshaba, & Pammenter, 1999), the concept of hardiness refers to a personality construct which combines three attitudes that provide resistance to stressful events: commitment, control and challenge. Commitment is the willingness to be involved with people, things and situations rather than to be disconnected, isolated or alienated. Control involves struggling to be in charge of the events taking place in our lives through our own ability to make choices between available options, instead of sinking into passivity and helplessness. Challenge implies being willing to learn constantly from one’s experience instead of avoiding uncertainties and potential threats (Maddi, 2002). According to the authors, these three factors are needed for people to find the necessary stimulus and courage to turn potentially threatening stressful circumstances into opportunities for personal growth. Indeed, hardiness is inversely related to longterm PTSD (Zerach & Elklit, 2017).
Sense of Coherence (SOC)
Developed by Aaron Antonovsky (1979), describes the resources (i.e., psychological, social, and cultural) that people successfully use to defy illness. According to Antonovsky, the sense of coherence has three components:
A) Comprehensibility: A conviction that things happen in an ordered and expected way and a feeling that one can understand and predict events in life;
B) Manageability: A belief that one has the necessary skills and the resources to take care of what happens in life, that events are controllable and can be managed and;
C) Meaningfulness: A sense that what happens in life is appealing and a source of satisfaction, that things in life are worthwhile one’s efforts, that the world in some way makes sense.
According to the author, SOC is a major factor in managing stress in a healthy way. In addition, SOC has been found to increase quality of life (Eriksson & Lindström, 2007) and to be strongly related to perceived mental health (Eriksson & Lindström, 2006). Importantly, in people with high SOC, stressful events have less impact on biological outcomes than people with low SOC (Lutgendorf, Vitaliano, Tripp-Reimer, Harvey, & Lubaroff, 1999).
Self-Efficacy
The concept of self-efficacy (Bandura et al., 1988) represents the confidence in one’s ability to influence events that affect one’s life. People with high self-efficacy - that is, those who believe they can achieve things based on their own abilities - and are more likely to think that difficulties are challenges to overcome instead of being avoided. During stressful situations, people commonly exhibit signs of distress. People with high self-efficacy tend to interpret this ”distress” as normal and unrelated to their ability to control the situation, therefore responding better and more “in control” when confronted with stressful situations. Indeed, self-efficacy predicts long-term recovery after assaults (Nygaard, Johansen, Siqveland, Hussain, & Heir, 2017).
The Neuropsychology of the Stress Response
The focus is on the brain circuits responsible for the stress response and the interaction between the limbic system and the Prefrontal Cortex (PFC) during stressful events (Arnsten et al., 2012; Arnsten, 2009; Arnsten et al., 2015; Bremner, 2006; Hendler et al., 2001; Shin et al., 2004; Taylor et al., 2008). The PFC has extensive connections that accentuate or inhibit actions in other brain regions, including inhibiting the fear responses of the amygdala, providing top-down regulation of behavior, thought and emotion related to the stress response (Arnsten et al., 2015). It has been shown that the PFC is very sensitive to the damaging effects of stress and that even mild acute unmanageable stress can cause a rapid failure of prefrontal cognitive function (Arnsten et al., 2012; Arnsten, 2009). Studies have underlined the negative correlation between amygdala hyperactivity and the prefrontal cortex activity (Arnsten, 2009; Banks, Eddy, Angstadt, Nathan, & Phan, 2007; Motzkin, Philippi, Wolf, Baskaya, & Koenigs, 2015). During stressful events, hyperactivity of the amygdala tends to “shut down” the PFC, thus reducing its cognitive capacities and its ability to down regulate and control the amygdala’s fear response. This creates a vicious circle in which primitive circuits of the brain control behavior (Arnsten et al., 2015). Activation of the PFC, through cognitive focused interventions or appraisals, helps reduce the stress response and down regulate the amygdala (Goldin et al., 2008). These provide the best environment for a calmer, more rational and flexible response after trauma exposure. In contrast, lack of PFC activity that maintains dominance of the limbic system, increasing the sense of helplessness, which is one of the major triggers for perceived trauma (Hantman & Farchi, 2015). Interestingly, activating the ventromedial prefrontal cortex can prevent the adverse effects of uncontrollable stress (Amat, Paul, Watkins, & Maier, 2008).
Studies have revealed that memories of events perceived as traumatic, are processed in more fragmented and automatic ways (Foa, Feske, Murdock, Kozak, & McCarthy, 1991; Liberzon et al., 1999; van der Kolk & Fisler, 1995). Furthermore, post-traumatic pathological conditions are associated with trauma processing with reduced prefrontal activity, which deals with cognitive processing, and enhanced limbic (amygdala) activation, responsible for negative emotional processing (Bremner, 2006; Hendler et al., 2001; Shin et al., 2004). In contrast, sense of mastery (akin to self-efficacy) and future orientation, among other psychosocial resources, are positively related to frontal activation and inversely related to amygdala activity (Taylor et al., 2008). These findings form the base to attempt to shift the processing of traumatic memories from a fragmented and limbic dominance mode to a more organized and prefrontal processing; a shift from narrative-based and emotionfocused interventions into cognitive focused interventions.
The SIX Cs Model: Its Basic Elements
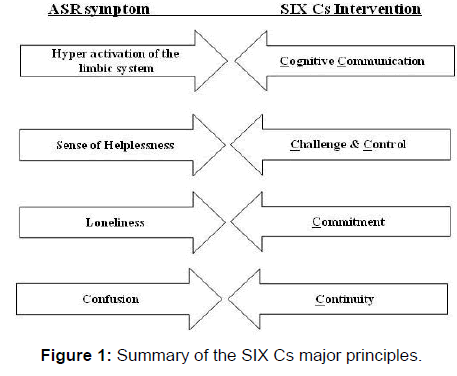
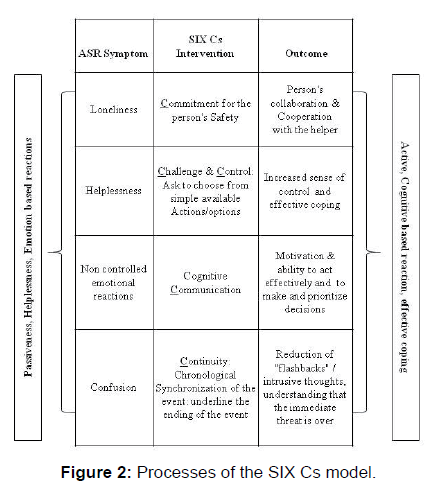
The SIX Cs model integrates these concepts and neurobiological underpinnings of stress and resilience into six main intervention elements, each one addressing different symptoms of the acute stress reaction or reflecting resilience factors as shown in Figures 1 and 2.
Amygdala hyper activity => Cognitive verbal communication: As previously mentioned, right after a PTE, hyperactivity of the amygdala tends to “shut down” the PFC creating a vicious circle in which primitive circuits of the brain control behavior, therefore calling for the need to have the PFC down regulate and control the amygdala’s response. This is accomplished by asking short cognitive questions that are related to the event. The questions focus on three main dimensions: Time e.g., “how long have you been here?” Quantity: e.g., “how many people are injured?” And choosing from simple options: e.g., “Do you want to talk first to your parents or your teacher?” The intention is to stimulate cognitive verbal communication to reduce the hyperactivity of the amygdala while increasing activation of the prefrontal cortex. The main objective is to “snap” the person out of the emotionally loaded reactions and induce the person to think more clearly, set priorities and make effective decisions.
Helplessness => Challenge: One of the most frustrating outcomes resulting from experiencing an acute stress reaction is the sense of inability and failure, which can increase helplessness and passiveness (Hantman & Farchi 2016). In order to reduce the sense of failure, we need to provide the person with a sense of success (Antonovsky, 1979) and self-efficacy (Bandura et al., 1988). This can be achieved by challenging the person to succeed in small simple cognitive based behavioral tasks related to the event (we will NOT try to distract the person’s mind from the event), e.g., “Please collect all your things into your bag and make sure that nothing is missing”. In this way, we challenge the person for effective activity related to the event as well as providing cognitive challenges, all decreasing one’s sense of helplessness and restoring a sense of self-efficacy and mastery. These may then increase activity of the ventromedial prefrontal activity and reduce amygdala activity (Amat et al., 2008; Taylor et al., 2008).
Helplessness => Control: According to ICD-10, helplessness is one of the factors that define the event as traumatic; therefore it is important to reduce this sensation immediately in order to shift the person to a more functional state without trying to distract the person from the event. This is accomplished by providing the person with several simple options to choose from, (e.g., “We need to count all the people, do you want to start counting or help with the registration of everybody?”; “In which area do you prefer the blood perfusion?”). This activity reinforces the cognitive activation of the PFC, improving the individual’s sense of control as opposed to the sense of helplessness and incompetence, and again, may modulate an over-active amygdala (Amat et al., 2008; Taylor et al., 2008).
Loneliness => Commitment: Loneliness is one of the frequent symptoms present after a PTE leading to difficulties to return to normal functioning; therefore it is important to reverse this symptom as soon as possible. This is accomplished by providing the person with a verbal commitment to his/her safety and support, assuring the person the helper will stay until the stressful event is over; e.g., “We are here with you, we are not going anywhere until you are safe again”. This alleviates the feeling of loneliness and fear and therefore increases the ability to collaborate with the helpers.
Confusion => Continuity: Confusion is the inability to create a synchronized narrative of the event. The confusion in the aftermath of a PTE results from the hyper arousal of the sympathetic nervous system (Hantman & Farchi, 2016). In addition, when the narrative is not synchronized, the person also fails to determine the accurate ending point of the event –which may contribute to the intrusive thoughts because, from the perspective of the person suffering from the ASR, the event has not ended and is still happening. Studies in both animal and human models have suggested that the window of opportunity to intervene and resolve this confusion state is no longer than six hours (Cohen et al., 2008; Zohar, Yahalom, et al., 2011). This underlines the need to help the person to reconstruct the event in an orderly and continuous manner as soon as possible in the immediate aftermath of the PTE. Providing “Continuity” entails explaining the person the basic chronological elements of the event and emphasizing the ending point, e.g., “Three minutes ago, you where involved in a car accident. Right now, the medics are here and are starting to treat the people who are injured. In the next 2-3 minutes, we will walk to the ambulance and you will be taken to the hospital for further checkups. The accident has ended!” Traumatized women, who were able to chronologically organize their recollection of the event, had reduced symptomatology (Foa, Riggs, Massie, & Yarczower, 1995).
To date, this approach has been recognized by the Israeli Ministry of Health as the Israeli national PFA model. The model has already been implemented and adopted as the main model for immediate assistance in stressful and emergency situation by several ministries and institutions such as the Ministries of Education, Health, and Internal Security; Israel traffic police; and by the Israel Defense Forces (IDF); under the assumption that, while interventions in emergencies are brief, at times lasting only seconds or minutes, their subsequent consequences may reverberate for many years after the event (Herman, 1992). Up until now, the model’s operational viability has been proven in extreme emergency conditions (Operation Pillar of Defense, Operation Protective Edge, earthquakes, etc.) as well as in many local events like rescues and accidents. We now demonstrate some standard empirical evidence for the method’s effectiveness.
The Six Cs Model: Preliminary Empirical Evidence For Its Efficacy
For obvious ethical and logistical reasons, it is extremely difficult to conduct randomized controlled trials during very urgent events or during war time, to test this model. Nevertheless, in order to empirically evaluate this intervention, several studies were conducted and two are briefly reported here. Study one tested the actual efficacy of the model in reducing anxiety symptoms in the aftermath of the event as well as PTSD symptoms two and four months following the event. Study two tested the effectiveness of the model in improving general self-efficacy, professional self-efficacy and resiliency, and in reducing perceived stress in high school students who received training in the SIX Cs model, compared to controls who did not receive the training.
Study One: A Six C’s Intervention during War-Time in the Community of Ofakim
Ofakim is a small town in the south of Israel, which was targeted by Hamas rockets during Operation “Protective Edge” in 2014. Over a period of 51 days, 280 individuals were treated for various stress reactions. Interventions were based on the SIX Cs protocols which included a 24/7 hotline, face-to-face interventions and community outreach. The hotline was available to individuals who were too frightened to leave their bomb shelters and reach the Center For Traumatized Persons (CTP). Most calls were from parents asking for advice regarding their children’s anxiety and stress, caused by the massive rocket and missile attacks. The faceto- face intervention included individual or small group treatment for those who came to the center. Community outreach included day and night patrols throughout the various neighborhoods and shelters carried out by trained students. People identified as suffering from ASR received the intervention on the spot. We sought to measure the effects of the intervention in reducing anxiety levels immediately after the event, as well as PTSD symptoms at four months follow-up after the event.
Materials and Methods
Participants and Procedures
Data was collected from 211 individuals 18 years and older who received a face-to-face intervention at the center for traumatized persons (CTP). Of the 211, 81.7% were women and 18.3% were men, 77.9% where urban dwellers (vs. 22.1% rural), 87% where Jewish and 13% were Bedouin Arabs.
Anxiety measures were taken upon arrival at the center before the intervention and right after the intervention, which lasted no longer than 45 minutes. Every person who entered the CTP and asked for assistance received the intervention. Baseline levels of General Self-Efficacy (GSE) and Post Traumatic Stress Disorder (PTSD) symptoms were collected two months after the event and follow up measures of GSE and PTSD symptoms were collected four months later, using phone-calls. The data collection was mandated by the Ministry of health as part of clinical Routine Outcome Monitoring (ROM) to evaluate clinical status as well as the effect of the intervention right after the event, and at the two month and four month follow up. Therefore, the need for obtaining informed consent was waived. Participants were asked for their permission to be contacted by telephone to ascertain their clinical status at follow up. Aggregated and anonymous data was used for the research purposes of this study.
Measurements and Statistical Analysis
Anxiety scores were collected as an integral part of the intervention using the one item question: Please rate your current anxiety from 1 (very low) to 10 (very high). This question reflected the person’s current anxiety state, and was validated by Davey et al. (2007) showing good correlations with the State Trait Anxiety Inventory (STAI). At the two and four month clinical routine evaluation follow ups, General self-efficacy (GSE) scores were collected using the GSE 20 items questionnaire (Schwarzer & Jerusalem, 1995) and PTSD symptoms were collected using Foa’s 17-item PTSD questionnaire (Foa, Riggs, Dancu, & Rothbaum, 1993). Means and standard deviations (SD) where calculated and paired sample t-tests of change over time were performed using SPSS© statistical package version 23.
Summary of Results
Mean anxiety level at baseline was 7.34 (SD±2.55). Mean anxiety level post-intervention dropped to 3.47 (SD±2.31), (t=16.28; p<0.000). There was a significant 52% reduction in the mean anxiety level as measured with the one-item anxiety scale.
Clinical follow up measures of PTSD symptoms and GSE are depicted in Table 1. PTSD symptoms dropped significantly and were below the clinical threshold (score lower than 15) while GSE increased only slightly but significantly at follow up.
| Variables | Two-month post intervention (baseline) | Four-month post intervention | t-value | ||
|---|---|---|---|---|---|
| M | SD | M | SD | t | |
| PTSD symptoms | 21.75 | 12.33 | 12.99 | 10.52 | 7.335 *** |
| GSE | 29.77 | 6.33 | 30.83 | 6.05 | 1.76 * |
| *** p<0.001; *p<0.05 | |||||
Table 1. Baseline and follow up PTSD symptoms and general self efficacy scores
The data presented here are unique since they were collected during real emergency events, during missile threat. The use of the SIX C’s model as IC-PFA during the very early minutes after arriving to the CTP was found to be successful in terms of reducing anxiety levels immediately after the intervention and PTSD symptoms below clinical threshold levels at the four month followup, while GSE scores increased less, but significantly as well. The main limitation of this preliminary study was the lack of a control group and the non-random nature of the study. However, due to ethical and logistic reasons of conducting a randomized controlled trial under an ongoing war and since the results are part of good clinical practice of monitoring patients’ outcomes, these were not possible. However, statistical data published by the Ministry of Health showed that the percentage of people who had to be referred to hospitals from other CTPs not using the SIX Cs intervention was approximately 25%, while only 0.5% of those in the CTP that provided the SIX Cs intervention had to be hospitalized (one person out of 250 who entered the CTP). Again, though not based on a randomized controlled trial, these figures provide additional preliminary evidence that the results obtained may be ascribed to the SIX Cs intervention.
Study Two: Effectiveness of a Six Cs Training Program for Adolescents
From October 2015 to September 2016, a longitudinal controlled study on the effects of training in the SIX Cs method on various outcomes was conducted among high school students. The study evaluated students’ general self-efficacy (GSE), Professional Self-Efficacy (PSE), resilience and perceived stress, before the intervention and at two weeks and three months follow-up.
Materials and Methods
Participants and Procedures
A total of 232 high school students between grades nine to eleven participated in the study. Of those, 108 students (42.59% males; mean age 15.84±0.48) went through two days of training, for three hours each day, of the SIX Cs model, and 124 controls (44.35% males; mean age 16.64±0.44) completed the questionnaires, but did not receive the SIX Cs training. The trainers were third year students in the stress, trauma & resilience program of Tel-Hai College, who completed an eight-hour training on the SIX Cs model in order to train others. Data on GSE, PSE, resilience and perceived stress were collected before the SIX Cs training (baseline, time 1), at two weeks follow-up after the training (time 2) and at three months follow-up after the training (time 3). Ethical approval was granted by the Ministry of Education’s review board prior to the study and informed consent was obtained from all participants.
Measurements and Statistical Analysis
The General Self-Efficacy scale (GSE) (Schwarzer & Jerusalem, 1995), was used to assess general self-efficacy. Cronbach’s alpha in this study was adequate: 0.84. Professional Self-efficacy (PSE) was assessed by a modified scale (Farchi, Cohen, & Mosek, 2014) based on an adaptation of the measure for specific self-efficacy developed by Boehm (Boehm, 2006). The measure consists of seven statements that refer to the respondent’s perception of selfefficacy concerning the capacity to act successfully in the field of stress and trauma; ability to influence people or organizations; knowledge of useful informants and contacts; proficiency in negotiation skills; expertise in using stress and trauma techniques; ability to form an appropriate support network; and mastery of required skills. The students were asked to indicate the degree of their agreement with each statement. The internal reliability of the original scale was α=0.85, and the scale’s Cronbach’s alpha for the present study was adequate, α=0.86.
The Connor-Davidson Resilience scale (CD-RISC) (K. M. Connor & J. R. T. Davidson, 2003); was used as a measure of the ability to cope with stress. This is a five-factor scale that includes 25 items, each rated on a 5-point scale (0-4). Factor 1 reflects the notion of personal competence, high standards, and tenacity. Factor 2 corresponds to trust in one’s instincts, tolerance of negative affect, and the strengthening effects of stress. Factor 3 relates to the positive acceptance of change and of secure relationships. Factor 4 is related to control and Factor 5 to spiritual influences. The CDRISC has been tested in the general population as well as in clinical samples and demonstrates good psychometric properties, with sound internal consistency (Cronbach’s alpha=0.89), test–retest reliability, and good distinction between those with greater and lesser resilience (K. Connor & J. Davidson, 2003). The Cronbach’s alpha of this scale in the present study was adequate, α=0.80.
Perceived stress was assessed by the Perceived Stress Scale (PSS) (Cohen, Kamarck, & Mermelstein, 1983). This scale has been widely used to assess perception of stress in daily life and has proven to have good psychometric properties in several studies. The scale includes 14 items regarding feelings and thoughts in the past month and provides responses on the frequency of these thoughts and feelings during the last month according to a Likertscale ranging from 0=never to 4=very frequently. The scale reflects perceptions of stress and the ability to cope with it. A total score was calculated for each participant. Reliability of the PSS in the present study was adequate as well: α=0.81.
Means and standard deviations (SD) were calculated for GSE, PSE, perceived stress and resiliency scores. A repeated measures ANOVA was conducted to explore the impact of change from baseline to time 2 and 3 and effects of intervention on students’ scores on GSE, PES, resilience and perceived stress, using the SPSS© statistical package version 23. In all analyses, we focused on the Time x Group interaction in relation to all outcomes.
Summary of Results
After excluding participants from the analyses due to missing information at follow up, the final sample was n=69 (63.8% of the initial sample) for the intervention group and n=86 (69.3% of the initial sample) for the control group, in relation to the outcomes of GSE, PSE and resilience. For perceived stress, 23 cases in the intervention group (21.29%) and 13 cases in the control group (10.48%) had to be excluded from the analysis due to missing data. Changes in GSE, PSE, Resiliency and Perceived stress scores among intervention and control groups are shown in Table 2.
| Variables | Intervention (n=69) |
Control (n=86) |
||
|---|---|---|---|---|
| M | SD | M | SD | |
| GSE | ||||
| Baseline | 32.38 | 2.98 | 32.87 | 3.29 |
| Time 2 | 32.00 | 5.08 | 32.59 | 4.75 |
| Time-3 | 33.42 | 3.94 | 20.78 | 9.25 |
| PSE | ||||
| Baseline | 29.39 | 7.04 | 33.40 | 9.01 |
| Time-2 | 38.23 | 6.99 | 34.77 | 8.21 |
| Time-3 | 34.59 | 8.68 | 25.59 | 5.86 |
| Resiliency | ||||
| Baseline | 26.77 | 6.38 | 28.76 | 6.70 |
| Time-2 | 28.30 | 6.29 | 29.71 | 6.29 |
| Time-3 | 29.16 | 6.25 | 19.98 | 8.75 |
| Perceived Stress | ||||
| Baseline | 25.74 | 5.97 | 23.44 | 6.36 |
| Time-2 | 23.62 | 5.57 | 22.51 | 7.35 |
| Time-3 | 22.48 | 6.33 | 30.09 | 7.57 |
Table 2. Group differences at baseline and follow up: GSE, PSE, Resiliency, Perceived Stress
At baseline, groups were significantly different on GSE, PSE, perceived stress and resilience. Controls scored significantly higher on GSE (t(234)=1.78, p<0.005), PSE (t(233)=3.49, p=0.001), resilience (t(234)=2.15, p<0.05) and perceived stress (t(232)=1.98, p<0.05). Therefore, and due to significant group differences at baseline, we statistically adjusted for all baseline measures in the following Analyses of Covariance (ANCOVA), except when analyzing each outcome variable, whose levels were considered in a within-subjects analysis, while the remaining baseline variables were entered as covariates.
The ANCOVA for GSE revealed a significant Time x Group interaction (F(2,256)=64,66), p<0.001). Simple effects analyses revealed that Time significantly affected GSE scores only in the SIX Cs group (F(2,128)=4.10, p<0.05) but not in controls (F(2,122)=0.76, p>0.05). We nevertheless examined certain mean differences within each condition separately, over time. Baseline GSE scores increased significantly at T2 for both the SIX Cs group (F(1,74)=4.49, p<0.05) and in controls (F(1,70)=5.47, p<0.05), independent of covariates. Additionally, GSE scores tended to decrease significantly in controls from baseline to T3 (F(1,82)=3.74, p<0.06) and increased significantly in the SIX Cs group (F(1,83)=10.64, p<0.005). At T3, the SIX Cs group scored significantly higher on GSE than controls, independent of baseline covariates (F(1,164)=74.51, p<0.001).
The ANCOVA for PSE revealed a significant Time x Group interaction (F(2,262)=44,60), p<0.001). Simple effects analyses revealed that time significantly affected PSE scores only in the SIX Cs group (F(2,126)=4.38, p<0.05) but not in controls ((F(2,130)=1.78, p>0.05). However, subsequent analyses found that PSE scores increased significantly in the SIX Cs group (F(1,73)=6.60, p<0.05) and in controls (F(1,70=4.04, p<0.05), independent of covariates. Furthermore, PSE levels were still significantly higher at T3 in the SIX Cs group compared to baseline (F(1,83)=5.60, p<0.05) but decreased, though not significantly in the controls (F(1,87)=0.64, p>0.05). At T3, the SIX Cs group scored significantly higher on PSE than controls, independent of baseline covariates (F(1,169)=90.04, p<0.001).
The ANCOVA for perceived stress revealed a significant Time x Group interaction (F(2,260)=24,00), p<0.001). Simple effects analyses revealed that time tended to significantly affected perceived stress scores only in the SIX Cs group (F(2,126)=2.75, p<0.07) but not in controls ((F(2,128)=0.99, p>0.05). Nevertheless, subsequent analyses found that perceived stress scores were reduced significantly in the SIX Cs group from baseline to T3 (F(1,83)=4.52, p<0.05) but increased though not significantly in the control group (F(1,86)=1.22, p>0.05). At T3, the SIX Cs group scored significantly lower on perceived stress than controls, independent of baseline covariates (F(1,168)=62.46 p<0.001).
Finally, the ANCOVA for resilience revealed a significant Time x Group interaction (F(2,262 )=51.26, p<0.001). Following this interaction, Time had a significant effect only in the SIX Cs condition (F(2,126)=4.26, p<0.05) while in controls time had not effect (F(2,130)=1.22, p>0.05). Indeed, from T1 to T2, resilience scores significantly increased in both the SIX Cs (F(1,74)=6.37, p<0.05) and controls (F(1,70)=4.34, p<0.05), independent of covariates. Furthermore, levels of resilience significantly increased from T1 to T3 in the SIX Cs group (F(1,82)=4.14, p<0.05) and tended to decrease in controls (F(1,87)=2.76, p=0.10). At T3, the SIX Cs group scored significantly higher on resilience than controls, independent of baseline covariates (F(1,168)=69.50, p<0.001).
These results were mediated by a tragic event that happened between time 2 and 3, an unfortunate car accident occurred and one of the participants in the control group, well known by both groups, died as a consequence of the accident. This event had an important impact on the study results. Following the car accident, the intervention group maintained a better score at 3 months followup compared to baseline while controls did not in all measures. Furthermore, at T3 the SIX Cs group scored significantly better on all outcomes compared to controls independent of covariates. Thus, this event could have partly affected the observed results.
This study was originally aimed to test the effects of the SIX Cs model ICF-PFA training on GSE and PSE as well as resilience and perceived stress, among high school students. As a result of a traffic accident, in which a very popular girl who belonged to the control group, but well known to both groups, control and intervention, died, the study was able to actually test the immediate effectiveness of the training in the aftermath of a perceived traumatic event. Scores for all variables measured were better at T3 (after the accident) for the intervention group compared to the control group. These results support the effectiveness of the SIX Cs interventions in providing and maintaining improved GSE, PSE and resilience and reduced levels of perceived stress in the long term. In addition, these results show improvement in actual resilience, (i.e., the ability to bounce back after a disaster), and reduced perception of stress for the intervention group in the face of a PTE
Conclusion
This article presents a new PFA approach - Immediate Cognitive-Functional Psychological First Aid (ICF-PFA) designed to provide the global nonprofessional community, professionals, and first responders, with practical tools that equip them with the necessary knowledge base and intervention skills to manage and assist others who perceive an event as traumatic and are at risk of developing ASR symptoms. The model emphasizes the need to shift a person who experienced a perceived traumatic event, from being in a helpless and passive state to an active and effective functioning person. This approach is based on the ICD-10 criteria for perceived trauma and on studies concerning the negative relationship between the activation of the amygdala and cognitive processing. Based on these two understandings, the SIX Cs model tries to directly target common ASR symptoms such as confusion, loneliness and emotional overflow. It aims to enable a person who experienced a PTE to return to previous effective functioning levels shortly (usually in less than two minutes) after receiving the intervention. Preliminary results point at the effectiveness of the SIX Cs model in terms of increasing resiliency and improving selfefficacy in non-professionals trained to respond to traumatic events. In addition, preliminary results observed during war-time suggest that this method may reduce anxiety and symptoms associated with PTSD in victims of a PTE. To the best of our knowledge, the SIX Cs model is the first PFA method designed to be implemented in all community levels, including first responder and both professionals and non-professionals. From this perspective, just like emergency medical first aid, each person, regardless of his or her profession, should have the basic knowledge, skills and ability to provide basic PFA to any other person in need. The SIX Cs approach is only meant as initial immediate cognitive-functional psychological first aid (ICF-PFA) to be used on the site of the event, on people showing signs of an ASR and as long as the person has not returned to his previous state of normal functioning.
Recommendation For Further Studies
The SIX Cs model has already been recognized by the Israeli Ministry of Health as the Israeli National PFA model, and has been adopted by most of the Israeli governmental offices, the Ministry of Education, Israel’s Internal Security Agency, Israel’s traffic police, and Israel Defense Forces (IDF) and it also has now several sub-protocols for emergency responders, educational system staff and high school children in place. Yet, there is a need for further evaluation of its effectiveness in the field, with greater samples and stronger methodological designs. Given the particular environment in which this model is implemented (i.e., terrorist attacks, war operations, earthquakes, etc.), it is a serious challenge, both ethically and methodologically, to test the model. These issues need to be tackled and resolved. The SIX Cs is a PFA model but also can be considered as a philosophic approach to handling crises and emergencies. In that sense, we hope and expect that the wide use of the model will contribute to increased personal, community and national resiliency and wellbeing. Currently, the model is being evaluated by the Israeli Defense Forces among soldiers that are being trained to provide psychological first aid in combat and in other situations, and among victims of trauma in the emergency room at several hospitals in Israel.
Disclosure Statement
The authors have no conflict of interest to report.
Acknowledgement
We would like to acknowledge the Ministry of health’s Mental Health Branch, for their support and professional help in developing and promoting the model. We would also like to acknowledge the Israeli ministry of education in particular Dr. Yochi Siman Tov, Head of the stress intervention unit for their support and willingness to host the study in the Israeli education system. Last but not least, we would like to thanks the students
from the Stress, Trauma & Resilience studies program Tel-Hai College who were instrumental in collecting the data on Study One during the attack escalation in the town of Ofakim.
References
- Amat, J., Paul, E., Watkins, L. R., & Maier, S. F. (2008). Activation of the ventral medial prefrontal cortex during an uncontrollable stressor reproduces both the immediate and long-term protective effects of behavioral control. Neurosci, 154(4): 117. Antonovsky, A. (1979). Health, Stress and Coping. San Francisco, CA: Jossey-Bass, Inc . Arnsten, A., Mazure, C.M., & Sinha, R. (2012). Neural circuits responsible for conscious self-control are highly vulnerable to even mild stress. When they shut down, primal impulses go unchecked and mental paralysis sets in. SciAm, 306(4): 48-53. Arnsten, A.F.T. (2009). Stress signalling pathways that impair prefrontal cortex structure and function. Nature reviews. Neurosci, 10(6): 410-422. Arnsten, A.F.T., Raskind, M.A., Taylor, F.B., & Connor, D.F. (2015). The effects of stress exposure on prefrontal cortex: Translating basic research into successful treatments for post-traumatic stress disorder. Neurobiol Stress, 1: 89-99. Bandura, A., Cioffi, D., Taylor, C.B., & Brouillard, M.E. (1988). Perceived self-efficacy in coping with cognitive stressors and opioid activation. J Pers Soc Psychol, 55(3): 479-488 . Banks, S.J., Eddy, K.T., Angstadt, M., Nathan, P. J., & Phan, K. L. (2007). Amygdala–frontal connectivity during emotion regulation. Soc Cogn Affect Neurosci, 2(4): 303-312. Bastos, M.H., Furuta, M., Small, R., McKenzie-McHarg, K., & Bick, D. (2015). Debriefing interventions for the prevention of psychological trauma in women following childbirth. Cochrane Database Syst Rev, 4: Cd007194. Benedek, D.M., Fullerton, C., & Ursano, R.J. (2007). First responders: Mental health consequences of natural and human-made disasters for public health and public safety workers. Annu Rev Public Health, 28: 55-68. Bisson, J. & Tavakoly, B. (2008). The TENTS guidelines for psychosocial care following disasters and major incidentsRetrieved from Wales, United Kingdom. Boehm, A. (2006). The involvement of social workers in fundraising. J Soc Serv Res, 32(3): 41-67. Bremner, J.D. (2006). Traumatic stress: Effects on the brain. Dialogues Clin Neurosci, 8(4):  445-461 . Bride, B.E. (2007). Prevalence of secondary traumatic stress among social workers. Soc Work, 52(1): 63-70 . Brymer, M.J., Jacobs, A.K . , Layne, C., Pynoos, R., Ruzek, J., Steinberg, A., et al. (2006). National Center for PTSD. Psychological First Aid: Field Operations Guide. (second edition ed). Buhle, J.T., Silvers, J.A., Wager, T.D., Lopez, R., Onyemekwu, C., Kober, H., et al. (2014). Cognitive reappraisal of emotion: A meta-analysis of human neuroimaging studies. Cereb Cortex, 24(11): 2981-2990. Burke, S., Richardson, J., & Whitton, S. (2013). Psychological first aid. An Australian guide to supporting people affected by disaster. Retrieved from Victoria, Australia. Cacciatore, J., Carlson, B., Michaelis, E., Klimek, B., & Steffan, S. (2011). Crisis intervention by social workers in fire departments: An innovative role for social workers. Soc Work, 56(1): 81-88 . Cieslak, R., Anderson, V., Bock, J., Moore, B.A., Peterson, A.L., & Benight, C.C. (2013). Secondary traumatic stress among mental health providers working with the military: Prevalence and its work-and exposure-related correlates. J Nerv Ment Dis, 201(11): 917-925. Classen, C., Koopman, C., Hales, R., & Spiegel, D. (1998). Acute stress disorder as a predictor of posttraumatic stress symptoms. Am J Psychiatry, 155(5): 620-624. Cohen, H., Matar, M.A., Buskila, D., Kaplan, Z., & Zohar, J. (2008). Early post-stressor intervention with high-dose corticosterone attenuates posttraumatic stress response in an animal model of posttraumatic stress disorder. Biol Psychiatry, 64(8): 708-717. Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. J Health Soc Behav, 24(4): 385-396. Connor, K., & Davidson, J. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). 18: 76-82. Connor, K.M., & Davidson, J.R.T. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2): 76-82. Davey, H.M., Barratt, A.L., Butow, P.N., & Deeks, J.J. (2007). A one-item question with a Likert or Visual Analog Scale adequately measured current anxiety. J Clin Epidemiol, 60(4): 356-360. Dyregrov, A. (2008). Psychological interventions in disasters - reflections from professional experience. Tidskrift for Norsk Psykologforening, 45(12): 1512-1516 . Eriksson, M., & Lindström, B. (2006). Antonovsky's sense of coherence scale and the relation with health: a systematic review. J Epidemiol Community Health, 60(5): 376-381. Eriksson, M., & Lindström, B. (2007). Antonovsky's sense of coherence scale and its relation with quality of life: a systematic review. J Epidemiol Community Health, 61(11): 938-944. Farchi, M., Cohen, A., & Mosek, A. (2014). Developing specific self-efficacy and resilience as first responders among students of social work and stress and trauma studies. Journal of Teaching in Social Work 34(2): 129-146. Fernandez, L., Barbera, J., & Van Dorp, J. (2006). Strategies for managing volunteers during incident response: A systems approach. Homeland Security Affairs. Foa, E.B., Feske, U., Murdock, T.B., Kozak, M.J., & McCarthy, P.R. (1991). Processing of threat-related information in rape victims. J Abnorm Psychol, 100(2): 156-162 . Foa, E. B., Riggs, D.S., Dancu, C.V., & Rothbaum, B.O. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress, 6(4):  459-473. Foa, E.B., Riggs, D.S., Massie, E.D., & Yarczower, M. (1995). The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behav Ther, 26(3): 487-499. Forneris, C.A., Gartlehner, G., Brownley, K.A., Gaynes, B.N., Sonis, J., Coker-Schwimmer, E., et al. (2013). Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med, 44(6): 635-650. Gidron, Y., & Nyklicek, I. (2009). Experimentally testing Taylor's stress, coping and adaptation framework. Anxiety Stress Coping, 22(5): 525-535. Goldin, P.R., McRae, K., Ramel, W., & Gross, J.J. (2008). The neural bases of emotion regulation: Reappraisal and suppression of negative emotion. Biol Psychiatry, 63(6): 577-586. Hantman, S., & Farchi, M. (2015). From helplessness to active coping in israel: psychological first aid. In E. W. Schott, E.L. (Ed.), Transformative Social Work Practice. California, USA: Sage . Harvey, A.G., & Bryant, R.A. (2000). Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry, 157(4): 626-628. Hendler, T., Rotshtein, P., & Hadar, U. (2001). Emotion–Perception Interplay in the Visual Cortex: “The Eyes Follow the Heartâ€. Cellular and Molecular Neurobiology, 21(6): 733-752. Herman, J.L. (1992). Trauma and recovery. New York. NY: Basic Books . Hobfoll, S.E., Hall, B.J., Canetti-Nisim, D., Galea, S .,  Johnson, R.J., & Palmieri, P.A. (2007). Refining our understanding of traumatic growth in the face of terrorism: Moving from meaning cognitions to doing what is meaningful. Appl Psychol, 56(3): 345-366. Howlett, J.R., & Stein, M.B. (2016). Prevention of Trauma and Stressor-Related Disorders: A review. Neuropsychopharmacology, 41(1): 357-369. Khoshaba, D.M., & Maddi, S.R. (1999). Early experiences in hardiness development. Consult Psychol J Pract Res, 51(2): 106-116. Kobasa, S.C. (1979). Stressful life events, personality, and health: an inquiry into hardiness. J Pers Soc Psychol, 37(1): 1-11 . Lazarus, R.S., & Folkman, S. (1984). Stress Appraisal and Coping. New York: Spring . Lee, J.S., Ahn, Y.S., Jeong, K.S., Chae, J.H., & Choi, K.S. (2014). Resilience buffers the impact of traumatic events on the development of PTSD symptoms in firefighters. J Affect Disord, 162: 128-133. Liberzon, I., Taylor, S.F., Amdur, R., Jung, T.D., Chamberlain, K.R., Minoshima, S., et al. (1999). Brain activation in PTSD in response to trauma-related stimuli. Biol Psychiatry, 45(7): 817-826. Lutgendorf, S.K., Vitaliano, P.P., Tripp-Reimer, T., Harvey, J.H., & Lubaroff, D.M. (1999). Sense of coherence moderates the relationship between life stress and natural killer cell activity in healthy older adults. Psychol Aging, 14(4): 552-563 . Maddi, S.R. (2002). The story of hardiness: Twenty years of theorizing, research, and practice. Consult Psychol J Pract Res, 54(3): 173-185. Maddi, S.R. (2006). Hardiness: The courage to grow from stresses. J Positive Psychol, 1(3): 160-168. Maddi, S.R., Khoshaba, D.M., & Pammenter, A. (1999). The hardy organization: Success by turning change to advantage. Consult Psychol J Pract Res, 51(2): 117-124. Motzkin, J.C., Philippi, C.L., Wolf, R.C., Baskaya, M.K., & Koenigs, M. (2015). Ventromedial prefrontal cortex is critical for the regulation of amygdala activity in humans. Biol Psychiatry, 77(3): 276-284. Nygaard, E., Johansen, V.A., Siqveland, J., Hussain, A., & Heir, T. (2017). Longitudinal relationship between self-efficacy and posttraumatic stress symptoms 8 years after a violent assault: An autoregressive cross-lagged model. Front Psychol, 8(913). Qi, W., Gevonden, M., & Shalev, A. (2016). Prevention of post-traumatic stress disorder after trauma: Current evidence and future directions. Curr Psychiatry Rep, 18(2): 20. Roberts, N.P., Kitchiner, N.J., Kenardy, J., & Bisson, J.I. (2010). Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database Syst Rev, 3: Cd007944. Rothbaum, B.O., Kearns, M.C., Price, M., Malcoun, E., Davis, M., Ressler, K.J., et al. (2012). Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biol Psychiatry, 72(11): 957-963. Rowlands, A. (2013). Social work training curriculum in disaster management. Journal of Social Work in Disability & Rehabilitation, 12(1-2): 130-144. Ruzek, J.I., Brymer, M.J., Jacobs, A.K., Layne, C.M., Vernberg, E.M., & Watson, P.J. (2007). Psychological First Aid. J Ment Health Couns, 29(1): 17-49. Sakuma, A., Takahashi, Y., Ueda, I., Sato, H., Katsura, M., Abe, M., et al. (2015). Post-traumatic stress disorder and depression prevalence and associated risk factors among local disaster relief and reconstruction workers fourteen months after the Great East Japan Earthquake: A cross-sectional study. BMC Psychiatry, 15: 58. Schreiber, S., Yoeli, N., Paz, G., I Barbash, G., Varssano, D., Fertel, N., et al. (2004). Hospital preparedness for possible nonconventional casualties: An Israeli experience. Ann Gen Psychiatry, 26: 359-366. Schulenberg, S.E. (2016). Disaster mental health and positive psychology-considering the context of natural and technological disasters: An introduction to the special issue. J Clin Psychol, 72(12): 1223-1233. Schwarzer, R., & Jerusalem, M. (1995). Generalized self-efficacy scale. In S.W.J. Weinman, & M. Johnston (Eds.) (Ed.), Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs, (pp. 35-37). Windsor, UK: NFER-NELSON . Shalev, A.Y., Ankri, Y., Israeli-Shalev, Y., Peleg, T., Adessky, R., & Freedman, S. (2012). Prevention of posttraumatic stress disorder by early treatment :  Results from the jerusalem trauma outreach and prevention study. Arch Gen Psychiatry, 69(2): 166-176. Shapiro, E. (2012). EMDR and early psychological intervention following trauma. Eur J Appl Psychol, 62(4): 241-251. Shin, L.M., Orr, S.P., Carson, M.A., Rauch, S.L., Macklin, M. L., Lasko, N.B., et al. (2004). Regional cerebral blood flow in the amygdala and medial prefrontal cortex during traumatic imagery in male and female Vietnam veterans with PTSD. Arch Gen Psychiatry, 61(2): 168-176. Sifaki-Pistolla, D., Chatzea, V.E., Vlachaki, S.A., Melidoniotis, E., & Pistolla, G. (2017). Who is going to rescue the rescuers? Post-traumatic stress disorder among rescue workers operating in Greece during the European refugee crisis. Soc Psychiatry Psychiatr Epidemiol, 52(1): 45-54. Simeon, D . ,  Greenberg, J., Nelson, D., Schmeidler, J., & Hollander, E. (2005). Dissociation and posttraumatic stress 1 year after the World Trade Center disaster: Follow-up of a longitudinal survey. J Clin Psychiatry, 66(2): 231-237 . Soldatos, C.R., Paparrigopoulos, T.J., Pappa, D.A., & Christodoulou, G.N. (2006). Early post-traumatic stress disorder in relation to acute stress reaction: An ICD-10 study among help seekers following an earthquake. Psychiatry Res, 143(2-3): 245-253. Speisman, J.C., Lazarus, R.S., Mordkoff, A., & Davison, L. (1964). Experimental reduction of stress based on ego-defense theory. J Abnor Soc Psychol, 68(4): 367-380. Taylor, S.E., Burklund, L.J., Eisenberger, N.I., Lehman, B.J., Hilmert, C.J., & Lieberman, M.D. (2008). Neural bases of moderation of cortisol stress responses by psychosocial resources. J Pers Soc Psychol, 95(1): 197-211. van der Kolk, B.A., & Fisler , R. (1995). Dissociation and the fragmentary nature of traumatic memories: Overview and exploratory study. J Trauma Stress, 8(4): 505-525 . Walker, L.S., Smith, C.A., Garber, J., & Claar, R.L. (2005). Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol, 24(4): 364-374. World Health Organization. (2015). The ICD-10 Classification of Mental and Behavioural Disorders. Version: 2015.Retrieved November 23, 2014 . World Health Organization, War Trauma Foundation, & World Vision International. (2011). Psychological first aid: Guide for field workers: World Health Organization . Yule, W. (2006). Theory, training and timing: Psychosocial interventions in complex emergencies. Int Rev Psychiatry, 18(3): 259-264. Zerach, G., & Elklit, A. (2017). Polyvictimization and psychological distress in early adolescence: A mediation model of defense mechanisms and coping styles. J Interpers Violence. Zohar,  J., Juven-Wetzler, A., Sonnino, R., Cwikel-Hamzany, S., Balaban, E., & Cohen, H. (2011). New insights into secondary prevention in post-traumatic stress disorder. Dialogues Clin Neurosci, 13(3): 301-309 . Zohar, J., Sonnino, R., Juven-Wetzler, A., & Cohen, H. (2009). Can posttraumatic stress disorder be prevented? CNS Spectr, 14(1): 44-51. Zohar, J., Yahalom, H., Kozlovsky, N., Cwikel-Hamzany, S., Matar, M.A., Kaplan, Z., et al. (2011). High dose hydrocortisone immediately after trauma may alter the trajectory of PTSD: Interplay between clinical and animal studies. Eur Neuropsychopharmacol, 21(11): 796-809.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 26375
- [From(publication date): 0-2018 - Nov 27, 2025]
- Breakdown by view type
- HTML page views: 22950
- PDF downloads: 3425