The Seasonal Pattern of Acute Pericarditis and Concurrence of Recurrent Pericarditis with Vitamin D Deficiency
Received: 26-Oct-2018 / Accepted Date: 12-Nov-2018 / Published Date: 19-Nov-2018 DOI: 10.4172/2332-0877.1000385
Keywords: Acute pericarditis; Viral infections; Seasonal pattern; Vitamin D deficiency
Introduction
Acute pericarditis is a disease caused by the inflammation of the pericardium [1]. Pericarditis is responsible for 0.1% of all hospital admissions and 5% of emergency room admissions for chest pain [2,3]. The causes of the acute pericardial diseases are aetiologically classified into infectious and non-infectious [4]. The most frequent cause of acute pericarditis is idiopathic in developed countries [5,6]. Idiopathic pericarditis is believed to be associated with a viral infection [7,8]. The most frequently seen viral pathogens are enteroviruses (Coxsackie viruses, Echoviruses), Herpes Viruses (Epstein–Barr Virus, Cytomegalovirus, and Human Herpes Virus-6), Adenoviruses, and Parvovirus B19 [4]. It has been known that climatic conditions affect infectious diseases for centuries [9]. Influenza and several other infectious diseases exhibit cyclic seasonal patterns, which may be explained by climate. A sudden drop in outdoor temperature might trigger the annual influenza epidemic [10]. The transition periods from summer to autumn or from winter to spring may be related with this condition. For example, Coxsackie virus B heart infections arise mainly during autumn and winter and other enterovirus infections peak in September to November [11-13]. Several environmental, behavioral, and immunological mechanisms have been proposed for the distinct seasonality of many viral pathogens [14,15]. If concomitance of viral infections and seasonality exist, the relationship between seasonality and acute viral pericarditis can be expected as well. However, there is little research into such a possible relationship. Moreover, vitamin D has an important role in the modulation of both innate and cellular immune responses [16]. The presence of vitamin D deficiency in the recurrent pericarditis is not known. Therefore, we investigated seasonal variations of acute pericarditis and concurrence of recurrent pericarditis with vitamin D level.
Methods
We retrospectively examined 216 patients diagnosed with acute pericarditis between February 2012 and November 2017. A written informed consent was obtained from each patient. The study protocol was approved by Medicana International Ankara Hospital Ethics Committee [Numbered: 2017/1]. The study was conducted in accordance with the principles of Declaration of Helsinki. The database was searched for all patients admitted with a first episode of acute pericarditis between February 1, 2012 and November 1, 2017. The patients with non-infectious pericarditis (post-cardiac injury syndrome, autoimmune causes, neoplastic, metabolic, traumatic and iatrogenic, drug-related) were excluded. Myocardial involvement (myopericarditis) was another exclusion criterion. To identify possible seasonal patterns, the incidence rates of acute pericarditis were categorized according to months. The diagnostic examination included physical examination, blood tests (chemistry including renal and liver function tests and C-reactive protein, high-sensitivity cardiac troponin I, complete blood count, chest x-ray, electrocardiogram, echocardiogram. The cardiac tomography imaging was used when indicated. The diagnosis of acute pericarditis was made by the presence of at least 2 of the following 4 criteria: typical pleuritic chest pain, characteristic electrocardiographic changes, pericardial friction rub, and new or worsening pericardial effusion. To identify possible seasonal patterns, the incidence rates of acute pericarditis were categorized according to months. The recurrent pericarditis (57 patients) was defined as the recurrence of pericarditis after a documented first episode of acute pericarditis and a symptom-free interval of 4–6 weeks or more. The nonsteroidal anti-inflammatory drugs (NSAIDs) were used as first-line treatment unless contraindicated. Colchicine was used as additional therapy. Prednisone was not used. Pericardiocentesis was not performed. Demographic, clinical, radiologic, and biochemical information, and follow-up findings obtained during the acute attack were collected. The recurrence was recorded only if there was evidence of hospital readmission or emergency room examination. Moreover, the vitamin D levels tests were done only in 50 recurrent pericarditis cases and in the 40 patients in time first episode of acute pericarditis cases. The blood samples were collected within 12-months. The vitamin D levels of pericarditis cases were compared.
Statistical analysis
Statistical analyses were performed using SPSS software (version17.0; SPSS Inc., Chicago, IL, USA). Continuous variables were presented as mean ± SD. Freedman's test (for any deviation from a uniform incidence) was used to analyze deviations, and Edwards's test was used to identify peaks and trough periods (for a harmonic curve (6 months between peak and trough)). The Ratchet circular test was used to identify short seasonal peaks, and Hewitt's rank sum test was used to evaluate a seasonal peak. A P value of <0.05 was considered statistically significant.
Results
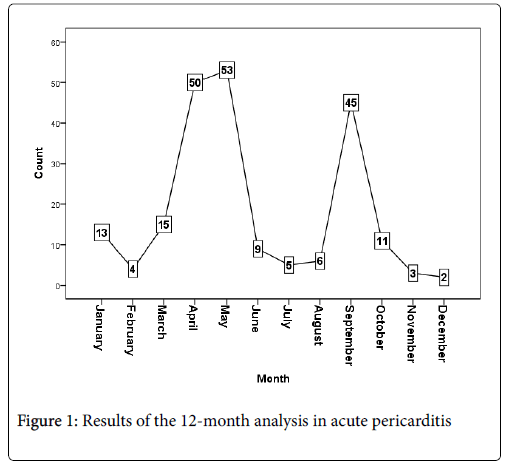
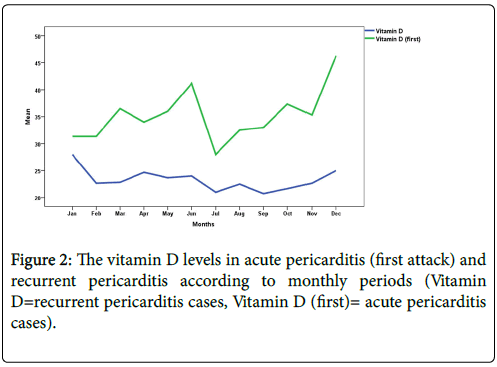
Out of 216 patients with acute pericarditis, 173 were male (80%) and 44 were female (20%). The patient characteristics are given in Table 1. Mean ages was 32 ± 6.3 years (min 17-maximum 56 years). Leukocyte count (WBC) was mean 6.54 (minimum 3.0- maximum 12.0 109 per L). High-sensitivity troponin I was 0.26 ± 1.19 ng/mL. High-sensitivity C-reactive protein was 0.99 ± 0.74 mg/L. Data on follow-up were available for 216 patients. The duration of follow-up ranged from 12 to 36 months. Recurrence ratio of acute pericarditis was 57 (26.3%). There were two peak appearances in the 12-month analysis (Figure 1). The incidence of acute pericarditis reached a peak in April and May (50 and 53 patients, respectively) and in September (45 patients). Peak date in Edwards's test (for a harmonic curve (6 months between peak and trough)) was May 21st, P=0.000 (7.2E-11). 2-month peak in Ratchet circular scan test (for a short seasonal peak) was April to May, p< 0.005. 3-month peak in Ratchet circular scan test was March to May, p<0.005. Hewitt's rank-sum test (for a seasonal peak); 4-month peak: March to June. Rank sum: 38, P > 0.089. 5- month peak: January to May Rank sum: 43, p>0.094. 6-month peak: January to June, Rank sum: 49, P>0.130While serum 25- hydroxyvitamin D levels in the recurrent pericarditis was 23.31 ± 4.16 ng/ml, this value in first pericarditis attack was 35.70 ± 6.81 ng/ml, p<0.001. The vitamin D levels in acute pericarditis and recurrent pericarditis according to monthly periods were showed Figure 2.
| Characteristics | Results |
|---|---|
| Male n (%) | 173 (79.7%) |
| Age (year), mean | 32 ± 6.3 (min 17-maximum 56) |
| Leukocyte Count (WBC), 109 per L | 6. 54 ± 22 (minimum 3.0-maximum 12.0) |
| High-sensitivity troponin I (cTn, ng/mL) | 0.26 ± 1.19 |
| High-sensitivity C-reactive protein (hs-CRP, mg/L) | 0.99 ± 0.74 |
| Recurrence n (%) | 57 patients (26.3%) |
| Vitamin D levels (ng/ml) in acute pericarditis and in the recurrent pericarditis, respectively (<20 deficient, ≥ 20-30 insufficient, ≥ 30 to optimal) | 35.70 ± 6.81 23.31 ± 4.16 p<0.001 |
Table 1: Characteristics of patients with acute idiopathic pericarditis (n=216)
Discussion
Humans have known that climatic conditions affect epidemic diseases for a long time before the role of infectious agents was discovered in the late nineteenth century (9). On the other hand, numerous environmental, behavioral and immunological mechanisms have been proposed for the distinct seasonality of many viral pathogens [14,15]. For example, a sudden drop in outdoor temperature might activate the annual influenza epidemic in a temperate climate by facilitating aerosol spread in dry air [10].
The most frequent cause of acute idiopathic pericarditis is the unrecognized viral infections. Therefore, it is not productive to try to isolate or identify the potential virus for pericarditis [17]. The most frequent viral pathogens are enteroviruses (coxsackie viruses, echoviruses), herpes viruses (Epstein–Barr virus, Cytomegalovirus, and Human Herpes Virus-6), Adenoviruses, Parvovirus B19 [4]. Rey et al. reported on higher frequency of a recent episode of upper respiratory tract infection or gastroenteritis in patients with acute idiopathic pericarditis [18].
If viral infections and seasonality coexist, the relationship between seasonality and acute pericarditis can be expected as well. For example, as a support to this hypothesis, enteroviruses typically appear in late summer or early autumn periods [19]. Zanettini at al. reported, in 2004, that idiopathic pericarditis had a seasonal pattern in a small (23 patients) group patients and coincided with the period for influenza vaccination [20]. They informed that pericarditis peaked in May and June months. Hammer et al. reported that acute idiopathic pericarditis appears to have a seasonal pattern with a distinct late winter peak, but seasonal pattern was not identified for recurrent episodes [21]. In our study, we found that idiopathic pericarditis had a seasonal pattern. This pattern had two peak appearances in the 12-month analysis. The incidence of acute pericarditis reached its peak in April and May and in September. However, recurrent pericarditis cases were not coexistence with seasonal pattern. Recurrent pericarditis cases included time except for peaked September and April. Our results support the abovementioned studies. In general, the acute pericarditis peaks occurred not only after the winter, which was the expected time for the lowest vitamin D levels, but also in September, when vitamin D levels were expected to be the highest of the year due to the elevations in circulating 25-hydroxyvitamin D levels that follow the summer time. However, vitamin D levels in the patients with recurrent pericarditis was found to be lower level than first pericarditis attack levels and no co-existence with seasonal pattern. We thought whether recurrent pericarditis cases had immunological pattern, and recurrent pericarditis cases should be examined in terms of immunological defect and vitamin D metabolism. Therefore, these cases may be due to low vitamin D levels anytime (figure 2). If acute pericarditis emerges seasonally, can this help in acute pericarditis therapy? Some authors have suggested that the immunological impact of shortened photoperiods during the winter months could increase population susceptibility to wintertime respiratory illness [15,22]. In addition, the striking mechanism for enhanced wintertime susceptibility would diminish production of active vitamin D metabolites in temperatezone populations in wintertime [23]. By concentrating on the associations between climate and disease, infection can be decreased by environmental and behavioral factors [24]. As a limitation, it can be stated that serology for common cardiotropic viruses, and immune panels were not examined due to technical insufficiencies.
Conclusion
We found that idiopathic pericarditis had a seasonal pattern and no seasonal pattern in recurrent pericarditis cases. In addition, relationship between recurrent pericarditis cases and vitamin D deficiency were established. Therefore, care should be taken for seasonality and disease preventive measures in acute pericarditis and recurrent pericarditis.
References
- Tonini M, MeloDT, Fernandes F (2015) Acute pericarditis. Revista Da Associacao Medica Brasileira 61: 184-90.
- Imazio M (2012) Contemporary management of pericardial diseases. Curr Opin Cardiol 27: 308-317.
- Imazio M, Gaita F (2015) Diagnosis and treatment of pericarditis. Heart 101: 1159-68.
- Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, et al. (2015) 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). See comment in PubMed Commons belowEur Heart J 36: 2921-2964.
- Imazio M, Gaita F, LeWinter M (2015) Evaluation and treatment of pericarditis: a systematic review. JAMA 314: 1498-1506.
- Troughton RW, Asher CR, Klein AL (2004) Pericarditis. Lancet 363: 717-727.
- LeWinter MM (2014) Acute pericarditis. New Eng J Med 371: 2410–2416.
- Imazio M, Spodick DH, Brucato A, Trinchero R, Adler Y (2010) Controversial issues in the management of pericardial diseases. Circulation 121: 916-928.
- World Health Organization (2003) Climate change and human health: risks and responses.
- Sundell N, Andersson LM, Brittain-Long R, Lindh M, Westin J (2016) A four-year seasonal survey of the relationship between outdoor climate and epidemiology of viral respiratory tract infections in a temperate climate. J Clin Virol 84: 59-63.
- Gaaloul I, Riabi S, Harrath R, HunterT, Hambda KB, et al. (2014) Coxsackievirus B detection in cases of myocarditis, myopericarditis, pericarditis and dilated cardiomyopathy in hospitalized patients. Mol Med Rep 10: 2811-2818.
- Bahri O, Rezig D, Nejma-Oueslati BB, Yahia AB, Sassi JB, et al. (2005) Enteroviruses in Tunisia: virological surveillance over 12 years (1992-2003). J Med Microbiol 54: 63-69.
- Kirkelis V, Spyrou N, Markoulatos P, Serie C (1985) Seasonal distribution of enteroviruses and adenoviruses in domestic sewage. Can J Microbiol 31: 24-25.
- Dowell SF, Ho MS (2004) Seasonality of infectious diseases and severe acute respiratory syndrome - what we don’t know can hurt us. Lancet Infect Dis 4: 704-708.
- Dowell SF (2001) Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis J 7: 369-374.
- Cantorna MT, Zhu Y, Froicu M, Wittke A (2004) Vitamin D status, 1,25- dihydroxyvitamin D3, and the immune system. Am J Clin Nutr 80: 1717S-1720S.
- Sagristá SJ, Almenar BL, Angel FJ, Bardajà RA, Bosch GX, et al. (2000) The clinical practice guidelines of the Sociedad Española de CardiologÃa on pericardial pathology. Rev Esp Cardiol 53: 394-412.
- Rey F, Delhumeau-Cartier C, Meyer P, Genne D (2015) Is acute idiopathic pericarditis associated with recent upper respiratory tract infection or gastroenteritis? A case-control study. BMJ Open 5: e009141.
- Fisman D (2012) Seasonality of viral infections: mechanisms and unknowns. Clinic Microbiol Infect 18: 946-1054.
- Zanettini MT, Zanettini JO, Zanettini JP (2004) Pericarditis. Series of 84 consecutive cases. Arq Bras Cardiol 82: 360-369.
- Hammer Y, Bishara J, Eisen A, Iakobishvili Z, Kornowski R, et al. (2017) Seasonal patterns of acute and recurrent idiopathic pericarditis. Clinic Cardiol 40: 1152-1155.
- Lofgren E, Fefferman NH, Naumov YN, Gorski J, Naumova EN (2007) Influenza seasonality: underlying causes and modeling theories. J Virol 81: 5429-5436.
- Cannel JJ, Vieth R, Umhau JC, Holick MF, Grant WB, et al. (2006) Epidemic influenza and vitamin D. Epidemiol Infect 134: 1129-1140.
- Kelly-Hope LA, Purdie DM, Kay BH (2004) El Nino Southern Oscillation and Ross River virus outbreaks in Australia. Vector-Borne Zoonotic Dis 4: 210-213.
Citation: Saricam E, Saglam Y (2018) The Seasonal Pattern of Acute Pericarditis and Concurrence of Recurrent Pericarditis with Vitamin D Deficiency. J Infect Dis Ther 6: 385. DOI: 10.4172/2332-0877.1000385
Copyright: ©2018 Saricam E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4758
- [From(publication date): 0-2018 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 4089
- PDF downloads: 669