Review Article Open Access
The Role of Endoscopy in the Management of Cholangiocarcinoma
Giacomin D1*, Fasoli R1, Tasini E1, Ciarleglio F2, Brolese A2 and de Pretis G1
1Department of Gastroenterology and Digestive Endoscopy, Trento, Italy
2Department of Surgery, HPB unit, Trento, Italy
- *Corresponding Author:
- Davide Giacomin
S.Chiara Hospital, Gastroenterology Largo medaglie d'oro
Trento, Trento 38122, Italy
Tel: +390461903954
E-mail: davide.giacomin@apss.tn.it
Received date: September 24, 2014; Accepted date: December 21, 2014; Published date: December 26, 2014
Citation: Giacomin D, Fasoli R, Tasini E, Ciarleglio F, Brolese A, et al. (2014) The Role of Endoscopy in the Management of Cholangiocarcinoma. J Gastrointest Dig Syst 4:248. doi:10.4172/2161-069X.1000248
Copyright: © 2014 Giacomin D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Cholangiocarcinoma is a complex disease, in most cases unresectable at the diagnosis. The cornerstone of management is biliary drainage. The endoscopic approach, in particular, is the treatment of choice both preoperatively and in the forms that require palliation. It makes use of a wide range of stents: plastic, metal self-expanding, bare, covered. Complicated hilar strictures require appropriate work-up, technical skill, strategy. Photodynamic therapy has proved to offer significant advantages in terms of survival and quality of life and favorable results as neo-adjuvant and adjuvant therapy against a discrete tolerability and fewer side effects than chemotherapy.
Keywords
Cholangiocarcinoma; Endoscopic biliary drainage; Photodynamic therapy; EUS; Quality of life
Introduction
Cholangiocarcinoma (CC) is a relatively rare tumor, being second in frequency after hepatocarcinoma as regards to malignant liver tumors and being responsible for approximately 3% of all gastrointestinal invasive neoplasms [1].
It may affect both the intra- and extra-hepatic biliary tree. About 20-30% of them are localized in distal main biliary tract, approximately 10% of them have an intra-hepatic involvement, whereas about two thirds develop at the carrefour, being called Klatskin tumors [2]
According to the Bismuth-Corlette classification [3], we recognize four types, based on involvement of hepatic left and right ducts. This classification is helpful not only in case of surgical treatment, but also in view of stent insertion both endoscopically and percutaneously. Endoscopic and percutaneous techniques allow access to obstructed bile ducts for subsequent diagnostic and therapeutic procedures. Both methods have advantages and disadvantages. Choosing between one or the other depends on several factors, such as anatomy of the upper gastrointestinal tract (for example, previous gastric resection), the stricture site and local expertise. Percutaneous approach (PTC) is more invasive and is usually adopted when endoscopic approach (ERCP) has failed or it could fail due to the stenosis difficulty [4]. The cornerstone of management is biliary drainage, both for symptomatic relief and for prevention of potential hepatotoxicity due to the chemotherapic agents, should the patient have an indication to chemotherapy. Drainage achieved through PTC is deemed to have a higher success rate than through ERCP. In a recent retrospective comparison, however, no difference between the two techniques was observed in terms of incidence of cholangitis, overall complications, procedure-related mortality and stent patency [5] (Table 1).
| No. of patients [%] [n = 85] | Endoscopic | Percutaneous | P value | |
|---|---|---|---|---|
| SEMS [%] | SEMS [%] | |||
| [n = 44] | [n = 41] | |||
| Successful | 72 [84.7] | 34 [77.3] | 38 [92.7] | 0.049 |
| palliation of | ||||
| cholestasis | ||||
| Procedure- related | 26 [30.6] | 13 [29.5] | 13 [31.7] | 13 [31.7] |
| complication | ||||
| Cholangitis | 22 [25.9] | 13 [29.5] | 9 [22.0] | 0.424 |
| Pancreatitis | 2 [2.4] | 0 | 0.138 | |
| Bleeding | 2 [2.4] | 0 | 0.138 | |
| Procedure-related | 1 [1.2] | 1 [2.3] | 0 | 0.229 |
| mortality |
Table 1: [by Paik WH et al. Gastrointestinal Endoscopy 2009] Initial clinical outcomes after biliary decompression by biliary drainage procedure [long-term clinical outcomes in 72 patients who underwent initial successful biliary decompression and in all 85 enrolled patients] SEMS: selfexpandable metal stent.
Pre-operative biliary drainage
The physiopathological premise of a pre-operative biliary drainage [PBD] should be to increase hepatic parenchyma resistance to ischemia, allowing it to overcome the surgically-induced damage. Through that way blood loss would also be reduced [6].
Part of the previous literature indeed, suggests a reduction of peri-operative morbidity and mortality [7,8] when patients were sent to surgery after undergoing a biliary drainage
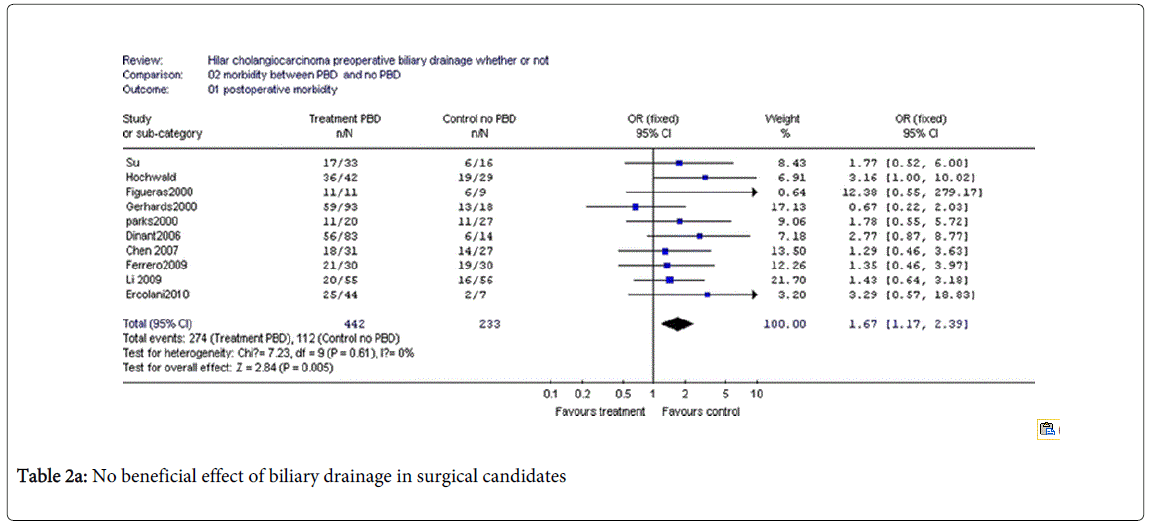
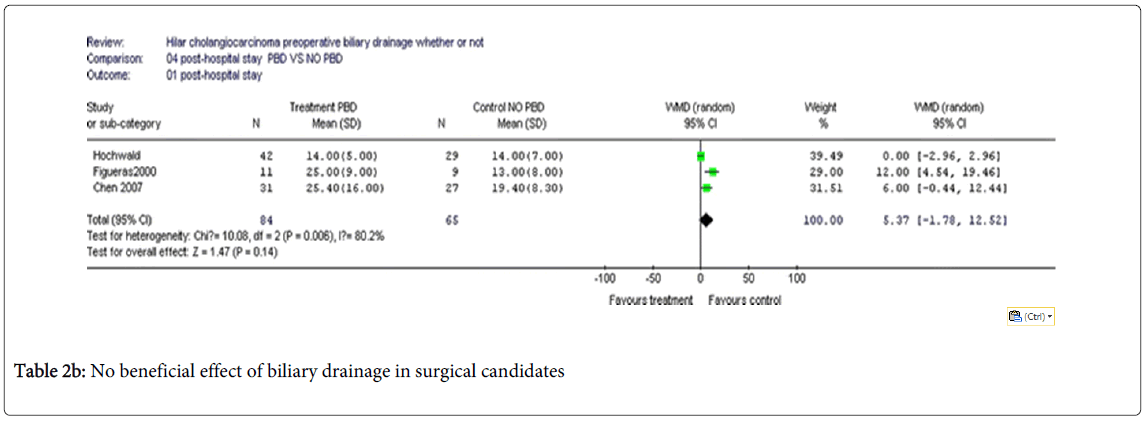
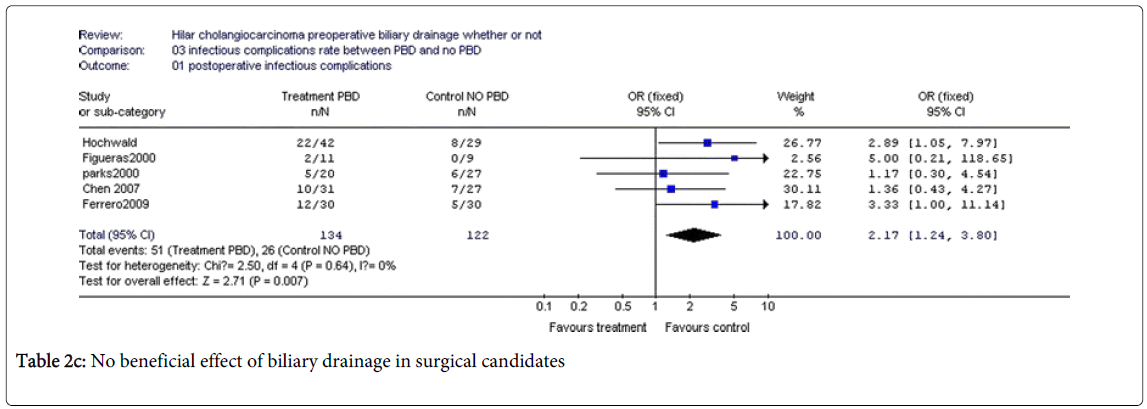
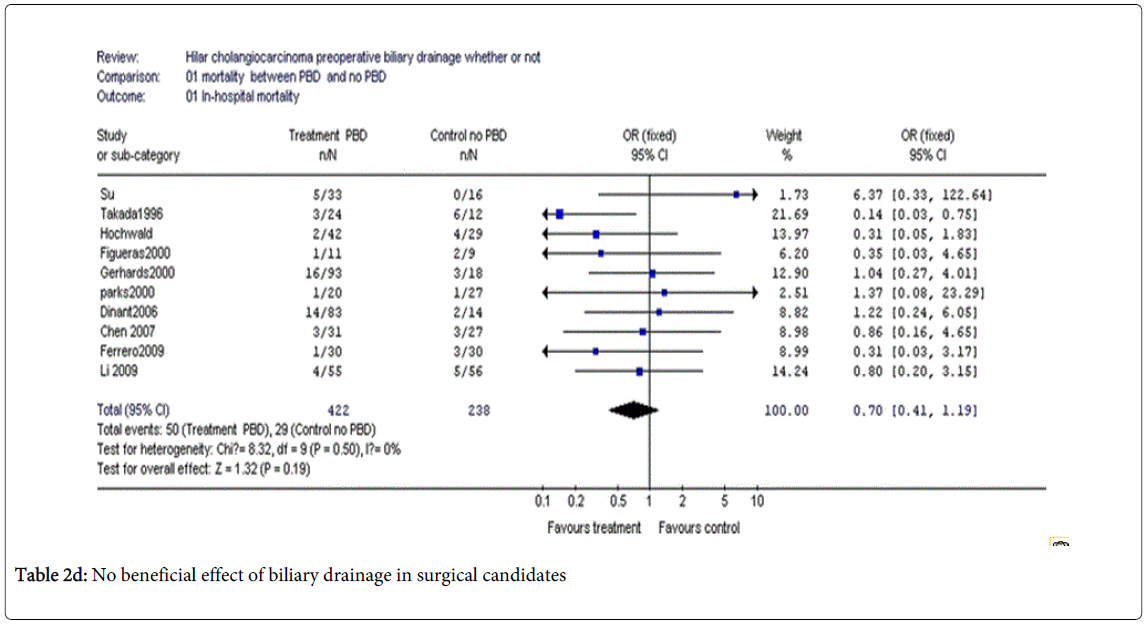
Coming to recent clinical studies, however, Liu et al. [9] – in a review published in 2011 – concluded that – by and large – there is no evidence of a clinical benefit in performing PBD in surgical candidates (Table 2).
Series of Tables 2a-2d by Fei Liu [9] showing no beneficial effect of biliary drainage in surgical candidates. Nevertheless, they identified a few clinical exceptions, mainly portal embolization, a procedure used to induce hypertrophia in residual segments in case of enlarged hepatectomy, which is impaired by hyperbilirubinemia. The role of routine PBD in resectable hilar cholangiocarcinoma remains controversial mainly due to the potential procedure–related morbidity and mortality when using one of the three available methods [percutaneous transhepatic biliary drainage-PTBD, endoscopic retrograde biliary drainage-ERBD and endoscopic naso-biliary drainage-ENBD].
Each of the above mentioned methods have some advantages over the other in relation to the risk of complications, capability to clearly define the correct tumor morphology and extension, patient compliance and finally the surgeon’s preference and skillness.
The ENBD seems to be the most appropriate procedure of PBD, because of the lower risk of tract tumor seeding and inflammatory response [10]. However, it implies the following drawbacks that make it unpopular and not accepted everywhere: poor tolerability, risk of accidental removal and a long hospital stay. So far, ERBD and PTBD continue to be the most common techniques worldwide adopted. However, regardless of the surgical center’s preferred technique, the main recommended concept is a short duration of PBD whenever a surgical procedure is scheduled.
In clinical practice, if the patient is due for surgery within two weeks, biliary drainage is considered not indicated, mainly because it carries a sensible complication rate [cholangitis, pancreatitis and perforation] [11]. Otherwise, once the drainage is achieved, it needs a certain time frame to act. In fact, Liu et al. [9], relying on a study of Koyama [12], hypothesized a 4-6 weeks time necessary to the hepatocyte in order to recover from damage secondary to prolonged jaundice. A shorter interval could be insufficient, whereas a longer one could expose the patient to the risk of infection. The studies that analyzed pre-operative biliary drainage in hilar cholangiocarcinoma patients undergoing surgical resection are described in Table 3.
| Studies which have analyzed preoperative biliary drainage in hilarcholangiocarcinoma patients undergoing surgical resection | ||||||||
|---|---|---|---|---|---|---|---|---|
| Ref. | Total number of patients with PBD | PBD associated morbidity | Serum bilirubin before surgery [mg/dL] | Duration of PBD [d] | Post-oper. morbidity | Postoperative complications | Infectious complications | 5-year survival rate |
| Hochwaldet al, Arch Surg1999 | 42 [PTBD 23; ERBD 13; intraoperative 3; ENBD 1; PTBD and ERBD 1; ERBD and ENBD 1] |
--- |
5.6 ± 0.9 |
--- |
90% |
5% |
52% |
-- |
| Figueraset al, Liver Transpl 2000 | 11 [PTBD 11] | --- | 11 ± 9.4 | 16 ± 10 | 100% | 9% | 18% | 25% |
| Ferrero et al, world J Surg 2009 | 30 [PTBD 18; ERBD 7; ERBD and PTBD 3; intra-operative 2] |
23% | 3.1 | 27.5 | 70% | 3% | 11% | --- |
| Kloeket al, j GastrointestSurg 2010 | 101 [PTBD 11; ERBD 90] |
76% | PTBD 1.1 ± 0.8; ERBD 1.3 ± 1.2 |
PTBD 11 [3-21]; ERBD 15 [4-29] |
--- | --- | 48% | --- |
| Grandadamet al, Ann SurgOncol 2010 | 12 [PTBD 12] | 25% | 4.1 ± 2.5 | 32 ± 9 | 13% | 0 | --- | 42% |
| Kawakami et al, J Gastroenterol2011 | 128 [PTBD 48; ERBD 20; ENBD 60] |
Total 40% [PTBD 31%; ERBD 65%; ENBD 38%] |
10.5 [2.2-29.3] |
11.4 [1-154] |
13% | 3% | --- | --- |
| Rattiet al,Worl J Surg 2013 | 55 [PTBD 51; ERBD 4] | 18% | 3.4 ± 1.5 | 24 [10-36] | 46% | 5% | 7% | 29% |
| Fargeset al, Br J Surg 2013 | 180 [PTBD 104; ERBD 63; PTBD and ERBD 13] |
33% | 2.8 [1.2-5.6] |
32 | 68% | 9% | --- | --- |
Table 3: By Paik WH et al. Preoperative biliary drainage in hilar cholangiocarcinoma, World J Gastrointestinal Endosc 2014
All reports were retrospective studies. Data are expressed as mean ± SD or median [range]. PBD: Preoperative biliary drainage; PTBD: Percutaneous transhepatic biliary drainage; ERBD: Endoscopic retrograde biliary drainage; ENBD: Endoscopic nasobiliary drainage.
Palliative endoscopic biliary drainage
Based on the fact that around 80% of hilar CCs are inoperable at the time of diagnosis, most experiences in biliary stenting has taken place in palliation cases. Different studies have shown self-expanding metals stents (SEMS) to be more efficacious than plastic stents (PS) in the management of malignant biliary strictures [13,14]. Likewise, also in hilar complex malignant strictures SEMS have shown a longer patency, a lower rate of re-intervention and longer survival [15,16].
Of course plastic stents still have a role when diagnosis has not yet been confirmed, when there is a chance of subsequent surgery and when photodynamic therapy is in program.
In everyday clinical practice it is not infrequent that the endoscopic biliary drainage is carried out without having a clear etiologic diagnosis and an accurate staging of the lesion. For this reason, choosing a “definitive” option (uncovered metal stents are not removable) might compromise more appropriate solutions for the patient.
Covered metal stents are on the other hand not feasible due to the risk of occlusion of hepatic branches adjacent to the drained ones.
Finally, plastic stents could be substituted by metal stents in case of occlusion of the former, once the diagnosis and prognosis are known, confirming the indication thereof.
Our institution is a secondary referral center representative of Northern Italy scenario and serving a population of just above half a million people. In the last 6 years 53 cases of cholangiocarcinoma [29 hilar, 18 located at the proximal common bile duct-CBD – 6 located at the distal CBD] have been diagnosed over a period of time ranging from January 2007 to December 2012. This is a figure in keeping with the incidence reported in the United States, i.e. about 2 cases per 100000 people per year [17]. Uncovered SEMS were initially positioned in 4 hilar cases and in 2 with a proximal CBD lesion; at this latter site, 3 further SEMS were subsequently inserted in substitution of obstructed plastic stents. None of the patients treated with SEMS underwent restenting. Histology and/or cytology confirmed diagnosis in 26 cases [49%], showing a doubtful finding in 7 further cases, whereas in the remaining it relied on imaging studies and clinical evidence. In a study by Domagk D et al. endoscopic transpapillary forceps biopsies had a similar diagnostic sensitivity and a specificity of 100% [18], while brush cytology alone has a much lower sensitivity [19]. The peroral cholangioscopy is suggested to have a higher accuracy with regard to malignancy in patients with indeterminate biliary lesions [20]. This might result advantageous in sparing further investigations and in shortening the diagnostic work-up. A recent prospective study, carried out by a group of Modena, Italy [21], shows that the SpyGlass system has a high accuracy for diagnosing or excluding malignancy in patients with indeterminate strictures or equivocal ERCP findings. They report sensitivity, specificity, positive predictive value and negative predictive value as 88, 94, 96 and 85% respectively. A similar conclusion is expressed by a Korean group [22] that conducted a small retrospective study. SpyGlass with SpyBite biopsies are still under evaluation in our center. The major concern about the system comes from the poor definition of the image. We need a technological improvement of the equipment before it can be considered a diagnostic standard.
Quality of life
There is growing evidence concerning improvement of quality of life [QoL] thanks to biliary drainage. Few studies have evaluated it in patients with malignant biliary obstruction, and variable methodology and scores were employed. Only recently a specific European Organization for Research and Treatment of Cancer [EORTC] questionnaire for biliary tumors has been implemented, QLQ-Bil 21 [23], and we await results on its applicability in everyday clinical experience.
Measurement of quality of life does not include only relief of itching and cosmetic effects on jaundice, but also the consequences of the disease on physical, relational and emotional well-being.
Whereas in distal malignant biliary strictures, the universal approach is to relieve jaundice no matter what associated symptoms are, with only few exceptions,[mainly the presence of a moribund patient], in hilar complex strictures the management is more articulated.
In particular, due to more difficult technical approaches and a higher rate of procedure-related complications, the anatomy of the lesion, a reasonable prognosis of the patient and the degree of both invalidating and ancillary symptoms must all be taken into consideration.
Nowadays various authors consider the use of metal stents to provide advantage in improving QoL [24,25] as well as survival [15,16]. A different, less optimistic view has been suggested by Robson et al. [26] who conducted a study on quality of life in patients treated with percutaneous drainage.
Negative aspects of endoscopic drainage include costs, complication rates, hospitalization for treatment of complications, further procedures for stent substitution due to clogging, migration, occlusion of an undrained hepatic segment. In fact, patients who undergo stent insertion might have a higher risk of cholangitis secondary to manipulation of the biliary tree and stent occlusion than for natural causes.
For these reasons we believe it is sound to be doubtful as regards stent positioning in elderly patients whose only symptom is painful jaundice or bed bound by irreversible disabilities. In these cases costs and/or complications may outweigh benefits [27]
Pros and cons of unilateral and bilateral biliary drainage
As far as Bismuth I strictures are concerned, there is unanimous consent as to the fact that a single stent is sufficient.
In more proximal strictures the most popular approach is to drain both hepatic lobes. Some Authors [28] have shown-in patients in whom a “complete drainage” had been reached through two plastic stents insertion – better survival, lower 30 days mortality, lower rate of cholangitis, lower rate of death due to sepsis.
Taking special precautions other Authors [29] have come to similarly encouraging results using a single stent: the operator should choose the obstructed duct easiest to cannulate, aiming at draining at least 25% of liver parenchyma [30]; administer antibiotic prophylaxis; inject a very low amount of contrast medium to avoid inappropriate filling of ducts not bound to be drained; once the access is gained, relieve pressure of the obstructed segment aspirating bile; shorten procedure times; perform aggressive treatment of the endoscopic failure through percutaneous approach.
In other words, should both lobes be reached by contrast, stents must be inserted bilaterally; if only one lobe is injected, unilateral drainage could be sufficient.
French Authors, estimating through Ct-scan volumetry of obstructed hepatic segments, have demonstrated that it is necessary to drain more than 50% of liver volume to obtain an efficacious palliation, particularly in Bismuth III strictures [31].
This implies almost invariably cannulation of two distinct liver territories and underlines the importance of pre-ERCP imaging [triphasic CT, cholangioRMN]. The latter allows tridimensional visualization of biliary tree, which offers to the operator information concerning which ducts to drain and which is wise to save injection to. These concepts are expressed in the recent European Society of Gastrointestinal Endoscopy guidelines to which we have spontaneously aligned over time [32].
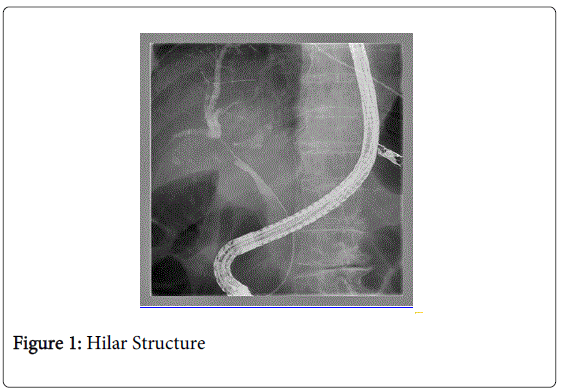
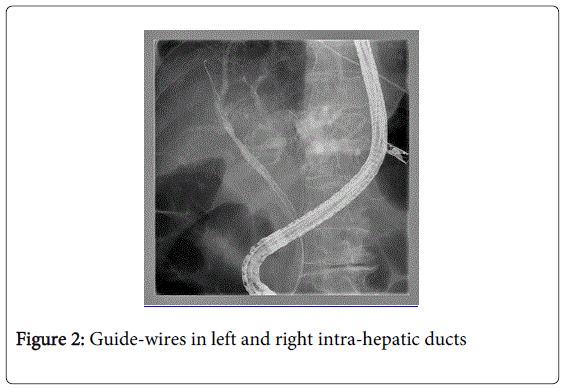
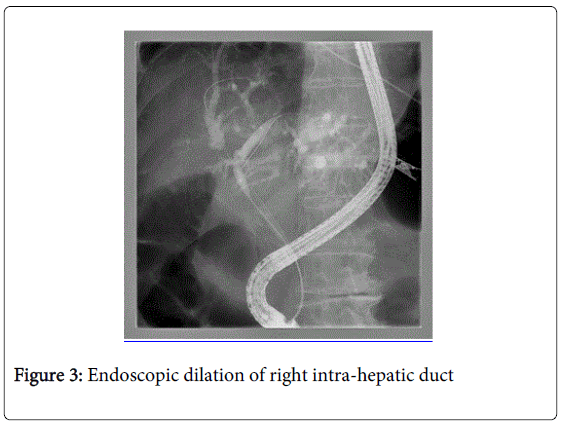
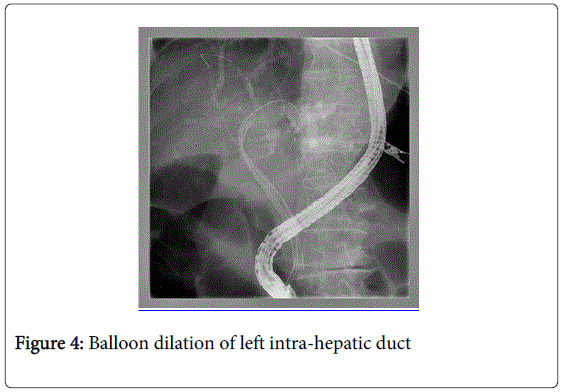
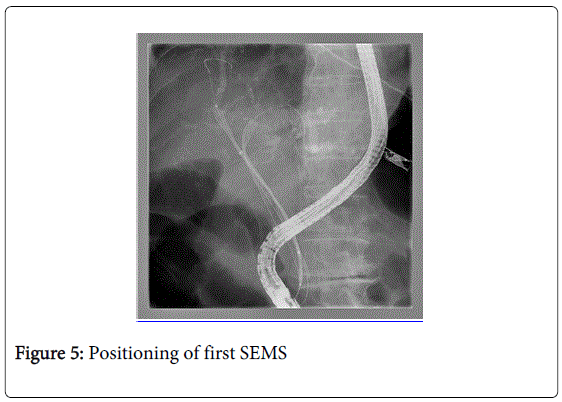
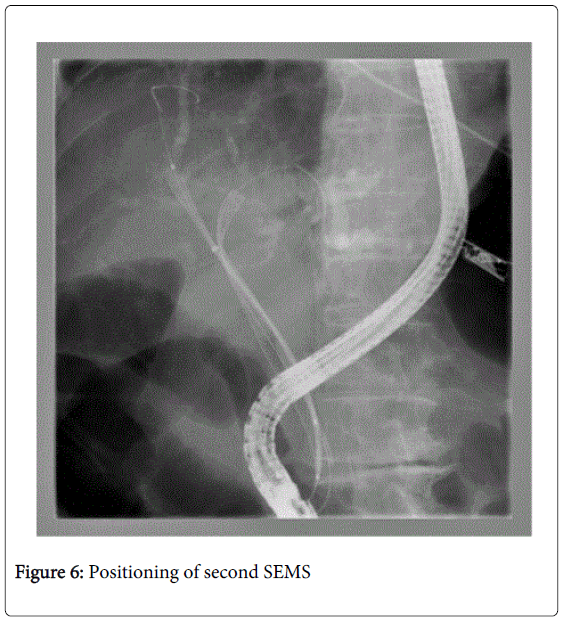
Endoscopic operating sequence (Figures 1-6): the methodology step-by-step is synthesized in our center through the acronimous “igwapri sphidiste”: imaging, guide-wire, aspiration, proximal injection [to the stricture], sphincterotomy, dilation, stenting.
Endoscopic ultrasonography [EUS]
Although EUS does not have a primary role in the treatment of CC, it may be considered in case of failure of the endoscopic drainage. In this context we need to mention the possibility to accomplish a EUS-guided rendez-vous procedure, as well as novel and partly experimental techniques of EUS-guided biliary drainage, which include: EUS-guided choledoco-duodenostomy and EUS-guided hepatico-gastrostomy.
EUS-guided rendez-vous – first described in 2004 [33] – consists of a puncture of the obstructed biliary duct [after a failed ERCP-guided access], passing in anterograde fashion a guide-wire through the papilla to the duodenal lumen in order to make feasible a subsequent ERCP. The aim of this procedure is to avoid a percutaneous trans-hepatic biliary drainage [PTBD], both less safe and less appreciated by patients.
Although biliary tree dilation makes EUS approach easier, the possibility to get EUS-guided access even to a CBD with a less than 10 mm calibre has been described.
Global success rate of the procedure has been described in the range of 80% [34]
EUS-guided biliary drainage [35] should be taken into consideration only in patients with proved biliary obstruction and after repeated failures of endoscopic drainage, with involvement of expert operators.
Choledoco-duodenostomy may be carried out in case of distal CBD obstruction , whereas – if the obstacle is proximal [hilar] – a EUS-guided intra-hepatic drainage is necessary [Hepatico-gastrostomy].
Post-surgical modifications of gastro-duodenal anatomy [gastrectomy with gastro-jejunostomy] make EUS-guided choledoco-duodenostomy impossible, because EUS visualization of choledocus typically occurs having the tip of the instrument in duodenal bulb or distal stomach.
Choledoco-duodenostomy has been first described in 2001 [36]. More than 100 cases have been reported in the literature, and in expert hands success rate is higher than 90% .
The technique implies positioning of a plastic or fully covered metal stent, which creates a communication between the CBD and the duodenal lumen. Possible complications are generally of mild degree and include retro-or intra-peritoneal biliary leakage, stent clogging or migration and may be treated either conservatively or endoscopically; occasionally surgical intervention is required [frank peritonitis].
EUS-guided hepatico-gastrostomy has been described for the first time in 2003 [37,38]; more than 50 cases have been described in the literature, with – in expert hands-a success rate higher than 90% and a complication rate of approximately 20%.
Regarding this kind of biliary drainage, the choice of positioning SEMS is gaining more and more popularity [39], and this is mainly due to three reasons: better prevention of biliary drainage; longer patency; easier management of malfunctioning secondary to ingrowth or obstruction.
The risk of biliary peritonitis, which is related to shortening and subsequent dislocation of metal stent, must be taken in particular consideration, due to its severity.
In conclusion, these EUS-guided procedures, although relatively simple to describe in their logical sequence, are indeed invasive and complex and require expert operators and an accurate selection of patients.
Their role is still a second-line approach after ERCP failure and possibly before PTBD.
Photodynamic therapy in cholangiocarcinoma
As stated above, CC has a dismal prognosis due to the fact that most cases come to our attention when the disease has already progressed to an inoperable stage. Furthermore, radiotherapy has shown disappointing results, and chemotherapy has also been demonstrated to be poorly effective only offering symptomatic palliation in occasional reports [40,41].
Biliary decompression-the main therapeutic goal in non-resectable cases – unfortunately affects prognosis only marginally, improving only slightly survival time [88-270 days in published series] [42].
Photodynamic therapy [PDT] is based on the injection of an intravenous porphyrin photosensitizer, followed by the endoscopic application of a particular wavelength light to the tumor tissue. The interaction between light and the photoagent-presumably by means of generation of oxygen free radicals – provokes cell death through a mechanism of apoptosis. Other effects of this interaction include an anti –angiogenetic effect and an immune-modulatory response, mainly due to a decrease of interleukin-6, a bile duct epithelium growth factor related to tumor mass.
After feasibility and promising phase II studies, the first randomized trial of PDT in the management of CC, utilizing Photofrin plus insertion of endoprosteses versus insertion of endoprostheses alone, had to be terminated because the survival advantage of additional PDT was highly significant [493 versus 98 days; p>0.0001], in addition to a relevant amelioration of jaundice and quality of everyday life [43].
These results have been confirmed in a subsequent European trial [44], in which a different photosensitizer was used [photosan].
A third randomized trial carried out in Korea [45] further confirms these figures (Table 4), whereas a study from Germany examines the problem from a different angle, suggesting that PDT plus stent insertion offers a similar survival to a R1/R2 surgical resection [approximately 12 months] [46].
| Study | Median Survival Time [days] | Mean Bilirubin Decrease [mg/dL] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Study Design | N [PDT/Stent] | PDT | Stent | Difference in means | CI 95% | p value | PDT | Stent | Difference in means | CI 95% | p value |
| Dumoulin [48] | Historical Control | 44 [24/20] | 297 | 168 | 129 | 2.29 - 255.71 | 0.05 | -10.7 | -5.8 | -4.9 | -8.73 - -1.07 | 0.01 |
| Ortner [43] | RCT | 39 [20/19] | 493 | 98 | 395 | 172.07 - 617.93 | 0.00 | -8.05 | -0.95 | 7.1 | -9.27 - -4.93 | 0.00 |
| Zoepf [44] | RCT | 32 [16/16] | 630 | 210 | 420 | 296.94 - 543.06 | 0.01 | -1.45 | -1.2 | 0.25 | -7.38 - +6.88 | 0.95 |
| Witzigmann [46] | Controlled Cohort design | 124 [68/56] | 360 | 192 | 168 | 45.69 -290.31 | 0.01 | -7.9 | -4.3 | -3.6 | -6.83 - -0.37 | 0.03 |
| Kahaleh [49] | Historical Control | 48 [19/29] | 486 | 222 | 264 | 11.41 - 516.59 | 0.04 | -4.8 | -6.5 | 1.7 | +0.76 - +2.64 | 0.78 |
| Quyn [50] | Controlled Cohort design | 40 [23/17*] | 425 | 169 | 256 | 59.81- 452.19 | 0.01 | / | / | / | / | / |
| Cheon [51] | Historical Control | 143 [72/71] | 294 | 219 | 75 | 39.79 - 106.21 | 0.03 | / | / | / | / | / |
Table 4: Controlled trials of PDT in the treatment of cholangiocarcinoma
Prasad et al. [47] have analyzed factors associated with increased survival after PDT: absence of a visible mass on imaging studies and a short time between diagnosis and PDT turned out to indicate a better response to treatment.
Further clinical aspects: A longer survival – although in a limited series of patients – has been observed extending the number of PDT sessions [beyond four ], associating in a few cases courses of chemotherapy [52]. PDT has also been reported to have a favorable outcome as adjuvant and neo-adjuvant therapy for CC, although published series are indeed very limited and Bismuth subtypes variable [42]. In the considered studies, palliative biliary stent placement was performed with either plastic or uncovered metal stents, which have shown a higher patency rate compared with the formers. However, uncovered metal stents have the potential disadvantage of damaging laser fibers used in PDT. Furthermore, stent removal is often necessary during PDT courses, and this is not possible with uncovered metal stents. For these reasons, plastic stent insertion is recommended in view of a possible PDT [53].
Tolerance: PDT seems to be a rather well-tolerated treatment, and side-effects are fewer than with chemo-or radio-therapy. Reports of cases of cholangitis have to be considered with caution, as they might be due to co-existing intra-hepatic strictures or insufficient endoscopic stenting after PDT.
PDT main adverse reaction-is photosensitivity: For this reason, treated patients should receive thorough explanations and advice. Their domestic situation, daily activities and support of relatives must be precisely assessed. Precautions and possible problems have to be discussed. A sun screen has to be provided, and emphasis should be put on the fact that the patient is highly photosensitive and sun creams alone are not able to protect them.
Conclusion
Trying to synthesize all the experiences available in the literature, we can conclude that PDT – if available as a reasonable opportunity – should be taken in serious consideration in patients with unresectable hilar CC with a life expectancy of at least 3 months, provided the option has been deeply discussed with the patient and an accurate informed consent has been taken, with particular care in dealing with precautions to be taken during treatment.
References
- Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, et al. (2002) Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol 37: 806-813.
- klatskin G (1965) Adenocarcinoma of the Hepatic Duct At Its Bifurcation within the PortaHepatis. An Unusual Tumor with Distinctive Clinical and Pathological Features. Am J Med 38: 241-256.
- Bismuth H, Corlette MB (1975) Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. SurgGynecolObstet 140: 170-178.
- Gerges C, Schumacher B, Terheggen G, Neuhaus H (2011) Expandable metal stents for malignant hilar biliary obstruction. GastrointestEndoscClin N Am 21: 481-497, ix.
- Paik WH, Park YS, Hwang JH, Lee SH, Yoon CJ, et al. (2009) Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilarcholangiocarcinoma: a percutaneous versus endoscopic approach. GastrointestEndosc 69: 55-62.
- Clements WD, Diamond T, McCrory DC, Rowlands BJ (1993) Biliary drainage in obstructive jaundice: experimental and clinical aspects. Br J Surg 80: 834-842.
- Miyagawa S, Makuuchi M, Kawasaki S (1995) Outcome of extended right hepatectomy after biliary drainage in hilar bile duct cancer. Arch Surg 130: 759-763.
- Nagino M, Nimura Y, Kamiya J (1995) Preoperative management of hilarholangiocarcinoma. J HepatobilPancreatSurg 2: 215-223.
- Liu F, Li Y, Wei Y, Li B (2011) Preoperative biliary drainage before resection for hilarcholangiocarcinoma: whether or not? A systematic review. Dig Dis Sci 56: 663-672.
- Kawakami H, Kuwatani M, Onodera M, Haba S, Eto K, et al. (2011) Endoscopic nasobiliary drainage is the most suitable preoperative biliary drainage method in the management of patients with hilarcholangiocarcinoma. J Gastroenterol 46: 242-248.
- Lee JH (2011) Self-expandable metal stents for malignant distal biliary strictures. GastrointestEndoscClin N Am 21: 463-480, viii-ix.
- Koyama K, Takagi Y, Ito K, Sato T (1981) Experimental and clinical studies on the effect of biliary drainage in obstructive jaundice. Am J Surg 142: 293-299.
- Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K (1992) Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet 340: 1488-1492.
- Soderlund C, Linder S (2006) Covered metal versus plastic stents for malignant common bile duct stenosis: a prospective, randomized, controlled trial. GastrointestEndosc 63: 986-995.
- Hong WD, Chen XW, Wu WZ, Zhu QH, Chen XR (2013) Metal versus plastic stents for malignant biliary obstruction: an update meta-analysis. Clin Res HepatolGastroenterol 37: 496-500.
- Sangchan A, Kongkasame W, Pugkhem A, Jenwitheesuk K, Mairiang P (2012) Efficacy of metal and plastic stents in unresectable complex hilarcholangiocarcinoma: a randomized controlled trial. GastrointestEndosc 76: 93-99.
- Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD (2005) Cholangiocarcinoma. Lancet 366: 1303-1314.
- Domagk D, Poremba C, Dietl KH, Senninger N, Heinecke A, et al. (2002) Endoscopic transpapillary biopsies and intraductal ultrasonography in the diagnostics of bile duct strictures: a prospective study. Gut 51: 240-244.
- Harewood GC, Baron TH, Stadheim LM, Kipp BR, Sebo TJ, et al. (2004) Prospective, blinded assessment of factors influencing the accuracy of biliary cytology interpretation. Am J Gastroenterol 99: 1464-1469.
- Ramchandani M, Nageshwar Reddy D, Gupta R (2011) Role of single-operator peroralcholangioscopyin the diagnosis of indeterminate biliary lesions: a single-center, prospective study. GastrointestEndosc 74: 511-519.
- Manta R, Frazzoni M, Conigliaro R, Maccio L, Melotti G, et al. (2013) SpyGlass single-operator peroralcholangioscopy in the evaluation of indeterminate biliary lesions: a single-center, prospective, cohort study. SurgEndosc 27: 1569-1572.
- Woo YS, Lee JK, Oh SH, Kim MJ, Jung JG, et al. (2014) Role of SpyGlassperoralcholangioscopy in the evaluation of indeterminate biliary lesions. Dig Dis Sci 59: 2565-2570.
- Friend E, Yadegarfar G, Byrne C, Johnson CD, Sezer O, et al. (2011) Development of a questionnaire (EORTC module) to measure quality of life in patients with cholangiocarcinoma and gallbladder cancer, the EORTC QLQ-BIL21. Br J Cancer 104: 587-592.
- Mihalache F, Tantau M, Diaconu B, Acalovschi M (2010) Survival and quality of life of cholangiocarcinoma patients: a prospective study over a 4 year period. J Gastrointestin Liver Dis 19: 285-290.
- Saluja SS, Gulati M, Garg PK, Pal H, Pal S, et al. (2008) Endoscopic or percutaneous biliary drainage for gallbladder cancer: a randomized trial and quality of life assessment. ClinGastroenterolHepatol 6: 944-950.
- Robson PC, Heffernan N, Gonen M, Thornton R, Brody LA, et al. (2010) Prospective study of outcomes after percutaneous biliary drainage for malignant biliary obstruction. Ann SurgOncol 17: 2303-2311.
- Sherman S (2001) Endoscopic drainage of malignant hilar obstruction: is one biliary stent enough or should we work to place two? GastrointestEndosc 53: 681-684.
- Deviere J, Baize M, de Toeuf J, Cremer M (1988) Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. GastrointestEndosc 34: 95-101.
- Polydorou AA, Chisholm EM, Romanos AA, Dowsett JF, Cotton PB, et al. (1989) A comparison of right versus left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy 21: 266-271.
- Dowsett JF, Vaira D, Hatfield AR, Cairns SR, Polydorou A, et al. (1989) Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology 96: 1180-1186.
- Vienne A, Hobeika E, Gouya H, (2010) Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. GastrointestEndosc 72: 728-735.
- Dumonceau JM, Tringali A, Blero D, Devière J, Laugiers R, et al. (2012) Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 44: 277-298.
- Mallery S, Matlock J, Freeman ML (2004) EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: Report of 6 cases. GastrointestEndosc 59: 100-107.
- Kim YS, Gupta K, Mallery S, Li R, Kinney T, et al. (2010) Endoscopic ultrasound rendezvous for bile duct access using a transduodenale approach: cumulative experience at a single center. A case series. Endoscopy 42: 496-502.
- Artifon EL, Ferreira FC, Otoch JP, Rasslan S, Itoi T, et al. (2012) EUS-guided biliary drainage: a review article. JOP 13: 7-17.
- Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, et al. (2001) Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy 33: 898-900.
- Burmester E, Niehaus J, Leineweber T, Huetteroth T (2003) EUS-cholangio-drainage of the bile duct: report of 4 cases. GastrointestEndosc 57: 246-251.
- Giovannini M, Dotti M, Bories E, Moutardier V, Pesenti C, et al. (2003) Hepaticogastrostomy by echo-endoscopy as a palliative treatment in a patient with metastatic biliary obstruction. Endoscopy 35: 1076-1078.
- Park do H, Koo JE, Oh J, Lee YH, Moon SH, et al. (2009) EUS-guided biliary drainage with one-step placement of a fully covered metal stent for malignant biliary obstruction: a prospective feasibility study. Am J Gastroenterol 104: 2168-2174.
- Hejna M, Pruckmayer M, Raderer M (1998) The role of chemotherapy and radiation in the management of biliary cancer: a review of the literature. Eur J Cancer 34: 977-986.
- Shinchi H, Takao S, Nishida H, Aikou T (2000) Length and quality of survival following external beam radiotherapy combined with expandable metallic stent for unresectablehilarcholangiocarcinoma. J SurgOncol 75: 89-94.
- Tomizawa Y, Tian J (2012) Photodynamic therapy for unresectablecholangiocarcinoma. Dig Dis Sci 57: 274-283.
- Ortner ME, Caca K, Berr F, Liebetruth J, Mansmann U, et al. (2003) Successful photodynamic therapy for nonresectablecholangiocarcinoma: a randomized prospective study.Gastroenterology 125:1355-1363.
- Zoepf T, Jakobs R, Arnold JC, Apel D, Riemann JF (2005) Palliation of nonresectable bile duct cancer: improved survival after photodynamic therapy. Am J Gastroenterol 100: 2426-2430.
- Cheon YK, Cho YD, Baek SH (2004) Comparison of survival of advanced hilarcholangiocarcinoma after biliary drainage alone versus photodynamic therapy with external drainage, Korean J Gastroenterol 44: 280-287.
- Witzigmann H, Berr F, Ringel U, Caca K, Uhlmann D, et al. (2006) Surgical and palliative management and outcome in 184 patients with hilarcholangiocarcinoma: palliative photodynamic therapy plus stenting is comparable to r1/r2 resection. Ann Surg Aug 244: 230-239.
- Prasad GA, Wang KK, Baron TH, Buttar NS, Wongkeesong LM, et al. (2007) Factors associated with increased survival after photodynamic therapy for cholangiocarcinoma. ClinGastroenterolHepatol 5: 743-748.
- Dumoulin FL, Gerhardt T, Fuchs S, Scheurlen C, Neubrand M, et al. (2003) Phase II study of photodynamic therapy and metal stent as palliative treatment for nonresectablehilarcholangiocarcinoma. GastrointestEndosc 57: 860-867.
- Kahaleh M, Mishra R, Shami VM, Northup PG, Berg CL, et al. (2008) Unresectablecholangiocarcinoma: comparison of survival in biliary stenting alone versus stenting with photodynamic therapy. ClinGastroenterolHepatol 6: 290-297.
- Quyn AJ, Ziyaie D, Polignano FM, Tait IS (2009) Photodynamic therapy is associated with an improvement in survival in patients with irresectablehilarcholangiocarcinoma. HPB (Oxford) 11: 570-577.
- Cheon YK, Lee TY, Lee SM, Yoon JY, Shim CS (2012) Longterm outcome of photodynamic therapy compared with biliary stenting alone in patients with advanced hilarcholangiocarcinoma. HPB (Oxford) 14: 185-193.
- Höblinger A, Gerhardt T, Gonzalez-Carmona MA, Hüneburg R, Sauerbruch T, et al. (2011) Feasibility and safety of long-term photodynamic therapy (PDT) in the palliative treatment of patients with hilarcholangiocarcinoma. Eur J Med Res 16: 391-395.
- Leggett CL, Gorospe EC, Murad MH, Montori VM, Baron TH, et al. (2012) Phodynamic therapy for unresectablecholangiocarcinoma: a comparative effectiveness systematic review and meta-analyses Photodiagnosis and Photodynamic therapy 9: 189-195.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14548
- [From(publication date):
December-2014 - Apr 11, 2025] - Breakdown by view type
- HTML page views : 9944
- PDF downloads : 4604